Blood sugar levels: what the numbers mean and how to act
Ever stared at a glucose reading and wondered if it's bad or not? Small swings are normal, but patterns matter more than a single number. Knowing common targets, how to test, and what to do when numbers go up or down gives you control—without stress.
Normal ranges and common targets
For people without diabetes, typical numbers are: fasting 70–99 mg/dL and about under 140 mg/dL one to two hours after a meal. For many people with diabetes, common targets used by clinicians are fasting or pre-meal 80–130 mg/dL and under 180 mg/dL one to two hours after eating. Hemoglobin A1c reports average control over 2–3 months; many aim for A1c below 7%, though individual goals vary. Always follow the targets your health care team gives you—individual needs change with age, pregnancy, and other illnesses.
How to test and track readings
Use a fingerstick glucometer for spot checks, or a continuous glucose monitor (CGM) for steady tracking. Schedule checks: fasting (first thing), before meals, 1–2 hours after meals, and when you feel off. During workouts, illness, or medication changes do extra checks. Write down the reading plus what you ate, what meds you took, and your activity. A week of notes often shows patterns that a single number hides.
When you review results, look for trends: are mornings high? Is one meal causing spikes? Patterns point to clear fixes—timing of meds, portion sizes, or changing meal composition.
Apps and simple spreadsheets work fine. If you use a CGM, check time-in-range (how often you’re within target), not just isolated highs and lows.
Quick fixes and everyday habits that move numbers
If a reading is mildly high after a meal, try a brisk 10–20 minute walk—walking helps muscles use glucose without extra medication. Cut back on sugary drinks and refined carbs, add fiber and protein at each meal, and watch portions. Spreading carbs across the day instead of one big meal reduces big spikes. Losing even 5% of body weight can improve insulin response for many people.
Low blood sugar (usually <70 mg/dL) needs fast action: 15–20 grams of simple carbs—juice, glucose tablets, regular soda—then recheck in 15 minutes. If you use insulin or certain pills, keep fast carbs handy and tell friends or family what to do in an emergency.
High, persistent readings (over 300 mg/dL) or symptoms like fast breathing, severe thirst, vomiting, or confusion may need urgent care—call your provider or go to the ER. Medication changes, illness, or missed doses often cause highs and require a provider review.
Practical rule: test smart, record clearly, act quickly on patterns. If you’re unsure what to do with your readings, schedule a short call with your health care team—changing one habit or one med can make readings steadier and life simpler.
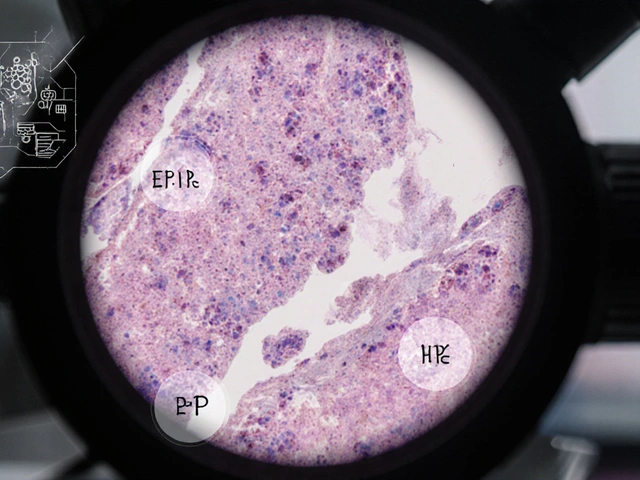
I recently came across a fascinating study about Amiloride, a medication commonly used to treat high blood pressure, and its potential impact on blood sugar levels in diabetic patients. Researchers have discovered that Amiloride may help to regulate blood sugar levels, providing a promising new treatment option for those struggling with diabetes. This is particularly exciting as it could mean a reduction in the need for insulin injections and other diabetes medications. However, further research is needed to fully understand the extent of Amiloride's impact on blood sugar levels and its long-term safety. I'll be keeping a close eye on this development and can't wait to share more updates with you all!
Read more