Integrated Recovery Plans: A Practical Guide to Coordinated Care
An integrated recovery plan puts every part of your care on the same page — doctors, medications, therapy, family support and daily habits. The goal is simple: speed recovery, reduce setbacks, and keep you out of needless ER visits. This page gives clear steps you can use right away to build a working plan.
Core parts of an integrated recovery plan
Start by breaking the plan into parts you can manage. Each part answers one question: who does what, when, and why.
1) Medical management: list diagnoses, meds, dosages, timing, who prescribes them, and known interactions. Include allergies and a single contact for urgent questions.
2) Rehabilitation and therapy: specify physical therapy exercises, speech or occupational goals, frequency, and expected milestones. Note any assistive devices needed.
3) Daily routine and lifestyle: sleep, nutrition, hydration, and activity limits. Small, consistent steps beat dramatic one-day changes.
4) Mental health and social support: link to counseling, peer support or caregiver plans. Recovery often stalls when stress or isolation goes unaddressed.
5) Monitoring and follow-up: set check-in dates, who tracks progress, which signs need immediate attention, and when to adjust treatment.
How to start — a practical checklist
Use this short checklist to turn ideas into action:
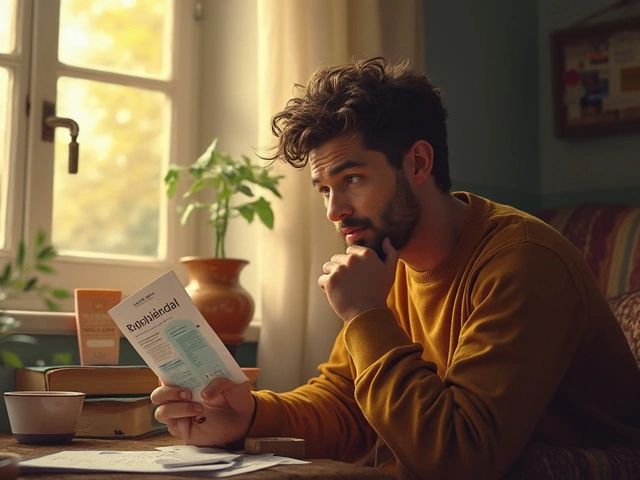
- Do a quick needs review. Write down current symptoms, current meds, mobility limits, and one short-term goal (for example: walk 10 minutes without stopping).
- Set three clear goals. One medical (finish antibiotic course), one function (return to work part-time), one lifestyle (sleep 7 hours). Make them specific and time-bound.
- Pick your team. Name the main clinician, therapist, pharmacist and a family contact. Share the plan with each person so responsibilities aren’t guessed.
- Make a medication plan. Note doses, when to refill, and an action if a dose is missed. Ask your pharmacist about interactions and simple reminders like pill boxes or phone alarms.
- Schedule checkpoints. Short, frequent reviews beat long gaps. Weekly at first, then extend as you improve.
- Write a short crisis plan. Include emergency contacts, red-flag symptoms, current meds, and where a live copy of the plan is stored (phone, fridge, caregiver).
Small examples work best. After surgery, a plan might include: stop certain meds 48 hours before, start gentle walking day 2, physical therapy twice weekly, and a wound check at day 10. For a flare of a chronic condition, the plan could list when to increase meds, who to call, and when to come in.
Keep the plan flexible. Recovery rarely follows a straight line. Track what changes things for you and update the plan quickly. If progress stalls, ask your core clinician to review and adjust meds or therapies.
Need a printable template or quick checklist to share with your doctor? Use the site’s downloadable plan (or ask a clinician to help convert your notes). A clear, shared plan saves time and reduces worry — and that helps you recover faster.
This article explores how pairing Antabuse (disulfiram) alternatives with structured counseling can transform alcohol dependence treatment. It unfolds the science behind new medication options, highlights counseling methods that drive results, and shows how combining these tools creates a more potent path to recovery. Real-life tips, practical examples, and up-to-date research take readers deep into modern integrated treatment plans. Whether you're comparing current therapies or searching for a new approach, you'll get actionable guidance on making the most out of medication and counseling together. Discover how a truly blended treatment can set the stage for lasting change.
Read more