Melasma Coping Strategy Planner
Your Personalized Coping Plan
Living with melasma is more than a cosmetic concern; it can stir up a mix of feelings that affect daily life. This guide breaks down why the patches appear, how they can shape emotions, and what practical steps you can take to feel better in your own skin.
What Is Melasma and Why Does It Happen?
Melasma, also known as facial hyperpigmentation, shows up as brown‑gray patches mainly on the cheeks, forehead, nose, and upper lip. It’s driven by excess melanin production, usually sparked by a trio of factors:
- Sun exposure - UV rays stimulate melanocytes, the cells that create pigment.
- Hormonal shifts - pregnancy, birth control pills, or thyroid changes can tip the balance.
- Genetic predisposition - families with a history of melasma often see it earlier.
While the physical spots are visible, the unseen side - how you feel about them - often determines whether you seek treatment or retreat from social activities.
Emotional Fallout: From Self‑Consciousness to Anxiety
Research from dermatology clinics in 2023 shows that over 60% of patients with melasma report lowered self‑esteem, and roughly one‑third experience anxiety that interferes with work or school. The emotional chain usually runs like this:
- Seeing the dark patches triggers self‑scrutiny.
- Self‑scrutiny fuels worries about judgment from others.
- Those worries can evolve into social anxiety, avoidance, and even depressive moods.
One 28‑year‑old teacher shared, “I stopped speaking up in class because I feared students would stare at the brown spots on my cheeks.” Stories like this highlight how melasma can shape identity, not just skin tone.
When Skin Concerns Turn Into Mental Strain
It’s easy to dismiss skin issues as “just skin,” but the mind‑body link is real. Anxiety linked to melasma often appears as:
- Constant checking of mirrors.
- Avoidance of photos, video calls, or social events.
- Sleep disturbances caused by worry about the next day’s appearance.
When these patterns persist, they can spiral into clinical depression. That’s why addressing the emotional impact is as important as treating the pigment itself.
Practical Coping Strategies That Work
Below is a quick‑reference table of proven coping tools. Each strategy pairs a mental‑health technique with a skin‑care habit, creating a two‑pronged approach.
| Strategy | Benefit | Tip to Start |
|---|---|---|
| Mindful Journaling | Reduces rumination | Write 5 minutes each night about feelings, not appearance. |
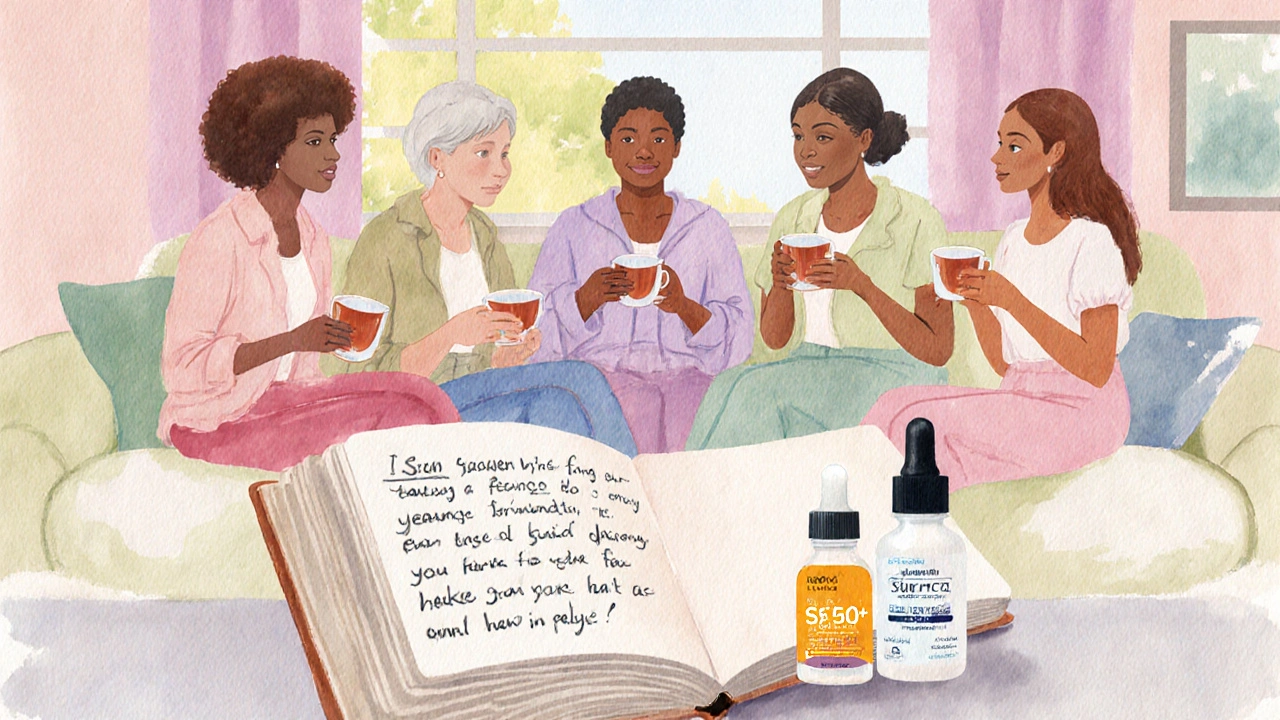
| Support Groups (online or in‑person) | Normalizes experience, builds community | Join a melasma Facebook group or local skin‑health meetup. |
| Sun Protection Routine | Prevents worsening patches | Apply SPF50+ every morning, reapply every 2hours outdoors. |
| Therapeutic Skin‑Care (e.g., gentle brighteners) | Gradual pigment reduction | Start with a 2‑% niacinamide serum, patch test first. |
| Cognitive‑Behavioral Techniques | Challenges negative thoughts | Identify a “melasma‑related” thought, replace with a neutral fact. |
These actions are simple enough to fit into a busy schedule yet robust enough to shift both skin and psyche.
Professional Help: Dermatologists and Mental‑Health Experts
When self‑managed steps aren’t enough, it’s time to seek specialists. A board‑certified dermatologist can assess the severity of melasma and suggest options such as:
- Hydroquinone creams (2‑4% concentration) to inhibit melanin synthesis.
- Tranexamic acid oral tablets that target pigment pathways.
- Laser or intense pulsed light (IPL) sessions for stubborn patches.
Because some treatments carry risks (e.g., irritation, post‑inflammatory hyperpigmentation), a dermatologist will tailor the plan to your skin type.
Equally vital is a mental‑health professional-psychologist or counselor-who can provide CBT, mindfulness training, or even short‑term medication for anxiety if needed. Integrated care, where skin and mind are treated together, yields the best outcomes.

Lifestyle Tweaks That Ease Both Skin and Mood
Small daily habits can cushion the emotional blow of melasma:
- Sun‑Smart Clothing: Wide‑brim hats and UPF shirts reduce UV exposure without constant re‑application of sunscreen.
- Balanced Diet: Antioxidant‑rich foods-berries, leafy greens, and nuts-support skin repair and improve overall mood.
- Exercise: Regular cardio releases endorphins, which naturally lift self‑esteem.
- Limit Alcohol & Smoking: Both can worsen pigmentation and increase stress levels.
Combining these habits with the coping table above creates a holistic shield against both the physical and emotional aspects of melasma.
Quick Takeaways
- Melasma is a hormone‑ and UV‑triggered hyperpigmentation that often fuels self‑consciousness.
- Emotional fallout can include anxiety, social withdrawal, and lowered self‑esteem.
- Effective coping blends mental‑health tools (journaling, CBT, support groups) with skin‑care practices (sun protection, gentle brighteners).
- Professional guidance from dermatologists and mental‑health clinicians ensures safe treatment and lasting confidence.
- Lifestyle tweaks-sun‑smart clothing, antioxidant diet, regular exercise-support both skin stability and mood.
Frequently Asked Questions
Can melasma disappear on its own?
Melasma rarely clears without intervention. Hormonal changes or reduced sun exposure can soften patches, but most people need targeted skin‑care or medical treatment for noticeable improvement.
Is sunscreen really necessary if I stay indoors most of the day?
Yes. UV rays penetrate windows, and indoor lighting can still trigger melanin production. Applying SPF in the morning creates a protective barrier that works even on cloudy days.
Are there any over‑the‑counter products that actually help?
Products containing niacinamide, azelaic acid, or low‑dose kojic acid can lighten spots gradually. Look for formulas that are fragrance‑free and formulated for sensitive skin to avoid irritation.
How do I find a good support group for melasma?
Search social platforms for “melasma support” or ask your dermatologist for local patient‑meet groups. Online forums often host weekly video chats where members share product experiences and encouragement.
When should I consider prescription‑strength treatment?
If patches cover large facial areas, darken despite sunscreen, or cause significant emotional distress, schedule a dermatologist visit. Prescription‑strength hydroquinone or tranexamic acid can accelerate fading, but they require monitoring.






Comments
Yeah, melasma can be a real confidence buster, but you don’t have to let it run your life. Keep a solid sunscreen routine and the rest will follow.
I get that the patches can feel overwhelming, especially when you’re constantly checking the mirror. Try setting a timer for each skincare step so it doesn’t become a chore. Pair that with a quick gratitude journal each night – it helps shift focus away from the skin. Small habits add up, trust me.
From a dermatological standpoint, consistent photoprotection is paramount; without it, any topical treatment is undermined. Additionally, consider a 2% niacinamide serum as the first line of adjunctive therapy. Ensure you patch‑test before full application.
🙌 Totally feel you on the self‑conscious vibe! The good news is there are tons of online support groups where you can share tips and memes. 🎉 Jump in and you’ll see you’re not alone.
Oh great, another skin “problem” that apparently needs a whole life plan. 🙄 Maybe just put on some SPF and stop overthinking.
Hey, I get the frustration. It’s easy to feel like it’s a mountain, but breaking it down into sunscreen, a gentle cleanser, and a supportive community makes it manageable.
The philosophical angle is interesting: we often project our inner insecurities onto visible traits. Recognizing that the skin is just one facet can reduce the mental load.
Practical tip: wear a wide‑brim hat and UPF clothing when outdoors. It’s a simple barrier that complements your SPF and saves you from constant re‑application.
Honestly, I think most of the hype around melasma “cures” is just marketing fluff. The condition is chronic; setting realistic expectations is key.
😅 True, but having a community that shares real experiences can cut through that fluff and give you honest insights.
Make sure you’re using fragrance‑free products to avoid irritation, especially if your skin is already sensitized from treatments. Consistency is the real hero here.
Melasma is more than a cosmetic issue; it intertwines with psychological well‑being in ways many overlook.
The hyperpigmented patches can act as a persistent reminder of hormonal shifts or sun damage, leading to a subtle but steady erosion of self‑esteem.
Studies from 2022 onward have shown that individuals with visible skin conditions report higher scores on anxiety inventories, even when controlling for other stressors.
This correlation suggests that the visual cue itself becomes a source of social anxiety, prompting behaviors like avoiding mirrors or camera lenses.
Over time, these avoidance tactics can spiral, limiting social interactions and professional opportunities.
Moreover, the nocturnal rumination about the next day’s appearance often disrupts sleep, creating a feedback loop of fatigue and heightened stress.
Stress, in turn, can exacerbate melasma, because cortisol influences melanocyte activity.
Breaking this cycle requires a dual approach: dermatological treatment to address the pigment and psychological strategies to manage the emotional impact.
Simple mindfulness exercises, such as focusing on the breath for five minutes, have been shown to reduce the intensity of intrusive thoughts.
Cognitive‑behavioral techniques, like challenging the automatic belief that “people will judge me,” replace distortion with factual statements.
Support groups add another layer by normalizing the experience and providing practical product recommendations backed by peer trials.
From a skincare perspective, sunscreen with at least SPF 50, broad‑spectrum protection, and re‑application every two hours is non‑negotiable.
Complementary agents, such as niacinamide, azelaic acid, or low‑dose tranexamic acid, can gradually lighten the patches when used consistently.
It is crucial to patch‑test new formulations to avoid irritant contact dermatitis, which would worsen the condition.
Finally, seeking a dermatologist who understands the psychosocial dimension ensures a treatment plan that addresses both skin and mind.
When patients feel heard on both fronts, adherence improves, and the pathway to clearer skin and calmer thoughts becomes far more attainable.
Great summary-treat the skin and the mind together.
If you’re not following the dermatologist’s advice, you’re basically saying you don’t care about your own health. That’s a harsh judgment but accurate.
Hey mates, just a heads‑up: a good hat and consistent SPF are cheap tricks that actually work. No need to over‑complicate it.
Oh sure, because we all have endless hours to meticulously log every tiny spot on our faces 📔. Meanwhile, the world keeps turning and nobody even notices the little brown smudge unless you point it out 🙄. But hey, if journaling about melasma makes you feel like a superhero, go for it 😆. Just don’t forget to actually put on sunscreen, otherwise your diary will be filled with new entries. At the end of the day, a little SPF beats a novel any day.
It’s fascinating how a pigment disorder can spark such a kaleidoscope of emotional colors-frustration, hope, determination. Embracing a balanced routine, like sunscreen plus a supportive community, paints a brighter picture.
Wow, another “miracle” serum? Yeah right-let’s all throw money at the next hype train while ignoring the basics.