Hypertension: Practical Ways to Understand and Manage High Blood Pressure
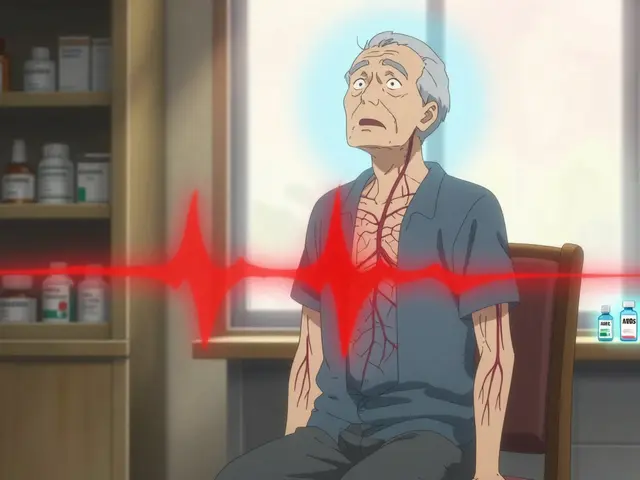
High blood pressure often shows no symptoms but quietly raises your risk of heart attack, stroke, kidney damage, and other problems. If you have hypertension, small practical steps can make a big difference in how you feel and how long you live.
Blood pressure is written as two numbers: systolic over diastolic. Normal is under 120/80 mmHg. Elevated sits between 120–129 over less than 80. Stage 1 hypertension is 130–139 systolic or 80–89 diastolic. Stage 2 is 140/90 or higher. Your doctor will use multiple readings before deciding on treatment.
Quick checks and targets
Home blood pressure monitors are cheap and useful, but accuracy matters. Buy a validated upper-arm cuff, not a wrist model. Sit quietly for five minutes before measuring, feet flat on the floor, arm at heart level. Take two readings one minute apart and record both. Morning and evening checks for a week give a clearer picture than a single clinic reading. Many adults aim for a target below 130/80, but your ideal number depends on age, other health issues, and what your doctor advises.
Medication and lifestyle — how they work together
Lifestyle changes often come first: cut salt to 1.5–2.3 grams daily, move for 30 minutes most days, lose even 5–10% of body weight if you’re overweight, limit alcohol to one drink a day for women and two for men, and follow the DASH-style diet (more vegetables, lean protein, less processed food). When lifestyle isn’t enough, doctors choose medications from well-known classes: ACE inhibitors (like lisinopril), ARBs (losartan), calcium channel blockers (amlodipine), thiazide diuretics (hydrochlorothiazide), and sometimes beta-blockers. Each class has common side effects—cough or elevated potassium with ACE inhibitors, leg swelling with calcium blockers, or increased urination with diuretics—so report new symptoms quickly.
Take meds the same time every day. Missing doses reduces benefit and raises risk. Some drugs interact with over-the-counter medicines—avoid regular NSAIDs for long stretches without checking with your clinician. Tell your provider about all prescriptions, supplements, and herbal products; some can raise blood pressure or blunt medication effects.
Seek urgent care if your blood pressure goes above 180/120 with chest pain, shortness of breath, severe headache, vision changes, or numbness on one side. Otherwise, plan regular follow-ups to review readings, labs (kidney function and electrolytes), and side effects. Keep a simple log of readings and share it at visits.
If you're over 65 or have diabetes or kidney disease, targets and meds change; some drugs need dose adjustment. Pregnant people with high blood pressure need specialist care—avoid ACE inhibitors and ARBs. Use phone apps to track readings and set reminders for meds. Before travel, pack meds and a paper list. Bring one saved chart to your appointments so your clinician sees trends quickly.
High blood pressure is common but manageable. Start with a reliable home monitor, try practical lifestyle moves, and work with your clinician on the right medication plan. Small, consistent actions pay off—check your numbers and act on them. Start small and be consistent. You can do this.
Looking for options beyond Losartan for managing blood pressure? This guide breaks down seven reliable alternatives. You'll get real comparisons, pros and cons, and tips for choosing the right medication. Each alternative is easy to understand, so you can have a better conversation with your doctor. Reading this could help you make a smarter decision for your health.
Read more