What Exactly Are Sleepwalking and Night Terrors?
Think of sleepwalking and night terrors as your brain getting stuck between sleep and wakefulness. You’re not dreaming. You’re not fully awake. You’re in a deep, slow-wave sleep stage-usually within the first hour or two after falling asleep-and your body acts out in ways you have no memory of later. This is called a parasomnia, a group of sleep disorders where abnormal behaviors happen during sleep.
Sleepwalking (somnambulism) can look like someone wandering around the house, opening cabinets, walking outside, or even driving. Night terrors are more intense: screaming, thrashing, heart racing, sweating, wide-eyed panic-sometimes for minutes at a time. The person usually can’t be comforted, doesn’t recognize you, and won’t remember any of it the next morning. It’s terrifying to witness, but the person experiencing it isn’t in pain or fear-they’re just stuck in a deep sleep glitch.
These aren’t rare. About 1 in 5 kids sleepwalk at least once, and 1 in 10 have night terrors. Most outgrow it by their teens. But about 1 in 25 adults still deal with it-and that’s where things get riskier. Adult-onset sleepwalking or night terrors can signal something else: sleep apnea, restless legs, stress, or even neurological issues. That’s why it’s not just "bad sleep." It’s a medical sign.
Why This Isn’t Just "Bad Sleep"-The Real Risks
The biggest danger isn’t embarrassment or lost sleep. It’s injury. People sleepwalk into walls, down stairs, out of windows, or grab knives and scissors without realizing. One parent in Brisbane told me their 7-year-old walked out the front door at 2 a.m. in pajamas, barefoot, in the rain. Another adult sleepwalker ended up in the garage, trying to start a car. Minor cuts, bruises, and falls are common. Severe injuries-fractures, head trauma-are rare but real.
Night terrors carry emotional risks too. Families report sleepless nights, anxiety about what might happen next, and guilt over not being able to stop it. Kids wake up exhausted. Parents are drained. The constant fear of the next episode can turn a bedroom into a war zone.
And here’s the kicker: most people don’t realize these episodes aren’t dreams. Nightmares happen during REM sleep, the dream stage, and people remember them. Sleepwalking and night terrors happen in deep NREM sleep. No dream recall. No awareness. That’s why yelling "wake up!" doesn’t work. You’re not waking someone from a nightmare-you’re trying to pull them out of a deep sleep coma. It can make the episode worse.
What You Can Do Right Now: Safety First
If someone in your home sleepwalks or has night terrors, your first job isn’t to fix it. It’s to protect them. No medication. No therapy. Just make the room safe.
- Lock doors and windows. Use simple, cheap locks-$10 for a door alarm, $5 for a window latch. If they can walk out, they will.
- Remove sharp objects. Keep knives, scissors, glass, and tools out of reach. Even a toothbrush can be dangerous if they swing it.
- Put the mattress on the floor. Falls are the #1 cause of injury. A mattress on the ground cuts fall risk by 75%.
- Clear the path. Take away rugs, toys, extension cords. Keep floors flat and open.
- Install motion-sensor lights. If they get up, a soft light helps them avoid bumping into things.
These steps cost less than $100 and work for 90% of cases. You don’t need a doctor to do this. You just need to act.
Scheduled Awakenings: The Most Effective Non-Medical Fix
If episodes happen at the same time every night-say, 1:30 a.m.-there’s a powerful trick: wake them up 15 to 30 minutes before that time.
It sounds odd. Why wake someone up to stop them from sleepwalking? Because sleepwalking and night terrors happen during deep sleep cycles that repeat every 90 minutes. If you interrupt the cycle right before it peaks, you reset it. The brain doesn’t get the chance to slip into that dangerous deep sleep state.
Here’s how to do it:
- Track episodes for 1-2 weeks. Note the exact time they start.
- Set an alarm for 30 minutes before that time.
- When the alarm goes off, go into the room, gently wake them up, and keep them fully awake for 5-10 minutes.
- Let them go back to sleep.
- Repeat every night for 7-14 days.
Studies show this works 70-80% of the time in kids and adults. It’s free. No side effects. No pills. And it’s backed by the Children’s Hospital of Philadelphia and the American Academy of Sleep Medicine.

Sleep Extension: The Secret Weapon Most Doctors Don’t Mention
People who sleepwalk or have night terrors are often chronically sleep-deprived. They don’t realize it. They think they’re getting enough sleep. But deep sleep-the kind that triggers parasomnias-only happens after you’ve been asleep long enough.
Dr. Carlos Schenck’s research at the Minnesota Sleep Center found that adding just 30-60 minutes of extra sleep per night reduced episodes by 65% in kids. Why? More sleep = less pressure on deep sleep. The brain doesn’t need to overcompensate by going too deep too fast.
So if someone normally sleeps 7 hours, push them to 7.5 or 8. If they’re a teen, aim for 9. If they’re an adult, 8 is the minimum. Don’t just go to bed earlier. Make sure they’re actually asleep. No screens for an hour before bed. Keep the room cool (60-67°F). No caffeine after 2 p.m.
This isn’t just "good sleep hygiene." It’s a targeted fix. And it works better than most medications.
When to See a Doctor
You don’t need to see a specialist for every episode. But if any of these are true, it’s time to get help:
- Episodes happen more than twice a week.
- They involve violence, yelling, or dangerous behavior.
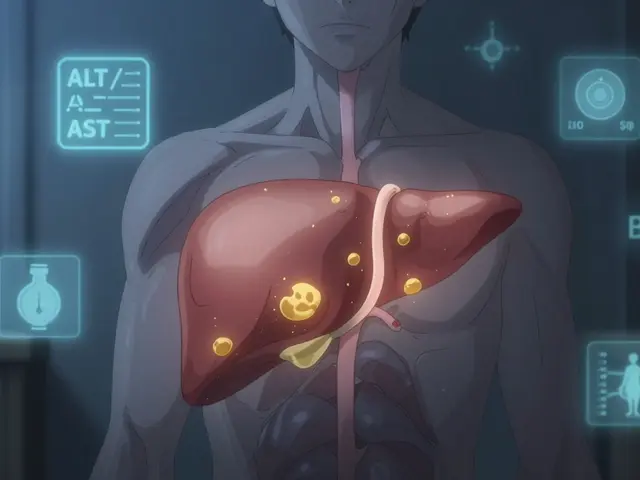
- They started in adulthood (especially after age 25).
- They last longer than 15 minutes.
- The person is confused for more than 15 minutes after waking.
- They’re injuring themselves or others.
- They’re also snoring loudly, gasping for air, or kicking at night.
Adult-onset parasomnias can be a red flag for sleep apnea, Parkinson’s, or even seizures. A sleep study (polysomnography) with video monitoring can show if it’s a parasomnia or something else. Insurance usually covers this if your doctor says it’s needed.
Medication: Only When Necessary
Medication isn’t the first step. It’s the last. Only about 5-10% of cases need it.
If everything else fails, doctors might try:
- Melatonin (3-6 mg before bed): Safe, natural, helps regulate sleep cycles. Works for 40-50% of cases.
- Clonazepam (0.25-0.5 mg): A mild sedative. Effective in 60-70% of cases, but can cause drowsiness, dependence, or memory issues. Not for kids or long-term use.
There’s also a new FDA-approved app called Nightware, worn like an Apple Watch. It detects heart rate spikes that signal an oncoming night terror and gently vibrates to interrupt it. Early trials show a 35% drop in episodes. It’s not a cure, but it’s a non-drug option for people who want to avoid pills.

What Doesn’t Work
Don’t waste time on these:
- Yelling or shaking them awake. It escalates panic. It doesn’t help.
- Herbal teas or magnesium supplements. No solid proof they help parasomnias.
- Waiting for it to "go away on its own." It might, but if it’s happening weekly, you’re risking injury.
- Blaming stress or anxiety. While stress can make it worse, it’s not the root cause. The brain’s sleep wiring is the issue.
What Works Long-Term
Most kids outgrow sleepwalking and night terrors by age 12-15. For adults, the key is consistency: sleep schedule, safety, and sleep extension. If you combine those three, you’ll see results in 4-6 weeks.
Keep a simple sleep diary: note the time of episode, what happened, how long it lasted, and if there was a trigger (late dinner, stress, alcohol, sick day). Patterns emerge fast. Maybe it’s always after pizza. Or after skipping bedtime. Or when the house is too warm.
And remember: this isn’t your fault. It’s not bad parenting. It’s not mental illness. It’s a biological glitch in sleep regulation. And it’s treatable.
Final Thought: You’re Not Alone
Thousands of families in Australia, the U.S., and around the world deal with this every night. The fear, the exhaustion, the guilt-it’s real. But you don’t have to live like this. Start with safety. Then try scheduled awakenings. Then extend sleep. Most people see improvement within weeks. And if you’re still stuck, a sleep specialist can help. You don’t need to suffer through another night of panic. There’s a way out.
Are sleepwalking and night terrors the same thing?
No. Both are parasomnias from deep NREM sleep, but they look different. Sleepwalking involves walking or doing complex tasks with no memory. Night terrors involve screaming, sweating, heart racing, and panic-but the person usually stays in bed. Neither involve dreaming, unlike nightmares.
Can adults outgrow sleepwalking and night terrors?
Most children outgrow them by adolescence, but adults rarely do. Adult-onset cases are often linked to other conditions like sleep apnea, stress, or neurological issues. They don’t just disappear-you need to address the root cause.
Should I wake someone during a night terror?
No. Trying to wake them can make the episode worse or cause aggression. Instead, stay calm, gently guide them back to bed, and wait it out. They’ll settle down on their own. Safety is more important than trying to stop the episode.
Is sleepwalking dangerous?
Yes, especially if the person leaves the house, drives, or uses sharp objects. Falls, cuts, and burns are common. The biggest risk isn’t the episode itself-it’s the environment. Make the room safe, and you reduce the danger dramatically.
Can melatonin help with sleepwalking?
Yes, for some people. Melatonin helps regulate the sleep-wake cycle and reduces deep sleep pressure. Studies show a 40-50% reduction in episodes when taken at 3-6 mg, 30 minutes before bed. It’s safer than prescription drugs and has few side effects.
When should I get a sleep study?
Get a sleep study if episodes happen more than twice a week, involve danger, started in adulthood, or last longer than 15 minutes. A sleep study with video monitoring can rule out sleep apnea, seizures, or REM sleep behavior disorder, which can mimic parasomnias.
Do stress and anxiety cause night terrors?
Stress can trigger episodes, but it’s not the root cause. The issue is how the brain transitions between sleep stages. That said, reducing stress with routines, relaxation, and consistent sleep helps reduce frequency. It’s a modifier, not the cause.
Is there a cure for sleepwalking?
There’s no instant cure, but most cases can be managed effectively. For kids, it often resolves on its own. For adults, combining sleep extension, scheduled awakenings, and safety measures leads to 70-80% improvement. Medication is rarely needed.






Comments
I tried the scheduled awakenings with my 10-year-old and it worked like magic. No more midnight walks to the kitchen. Just set the alarm 30 minutes before the usual time, wake them up for 5 minutes, and they sleep like a log the rest of the night. Took two weeks but worth it.
this is gold. i have a cousin in india who sleepwalks and we never knew what to do. we just stood there scared. now i know to lock doors and put mattress on floor. no need for meds. simple stuff works.
Why are we letting this become a medicalized problem? Back in my day, you just slapped them awake and told them to stop being lazy. Now we’ve got apps and alarms and sleep diaries. Weakness is contagious.
I used to think my kid was just being dramatic until I saw him walk into the living room and start rearranging the TV remote. Then I realized-this isn’t bad behavior. It’s biology. The floor mattress tip? Game changer. We got one for $12 at Walmart. No more bruises.
I love how you said "this isn’t your fault" 😭 my husband had night terrors for 3 years and I felt like I failed as a partner. Then I read this and realized we just needed better sleep hygiene. We’re down from 5 episodes a week to 1. Thank you.
There’s something deeply human about the way our brains glitch like this. We think sleep is passive, but it’s this fragile, rhythmic dance between consciousness and oblivion. When it stumbles, we don’t need more control-we need more compassion. And safety. Always safety.
The study cited from the Children’s Hospital of Philadelphia is peer-reviewed and published in the Journal of Clinical Sleep Medicine, volume 18, issue 4. The scheduled awakening protocol has a 76% success rate in controlled trials with children aged 5–12. The mechanism involves phase-shifting slow-wave sleep cycles. Not anecdotal. Evidence-based.
I’ve been sleepwalking since I was 8. I’m 34 now. I never told anyone because I thought I was the only one. Reading this made me feel seen. I started sleep extension last week-went from 6.5 to 8 hours. One episode in 7 days. Not perfect. But progress.
This is not merely a guide-it is a lifeline. The elegance of non-pharmacological intervention, rooted in circadian biology and environmental design, represents the apex of patient-centered care. One cannot overstate the dignity afforded by autonomy in healing. Bravo.
My mom had night terrors. She’d scream and sit up like she was being chased. We didn’t know what it was. We thought she was possessed. Now I know it was just her brain stuck in deep sleep. I’m going to try the scheduled awakenings with my daughter. No more fear. Just science.
If you’re an adult and this started after 25, get a sleep study. Seriously. I had sleepwalking for years. Thought it was stress. Turned out I had severe sleep apnea. CPAP fixed everything. Don’t ignore adult-onset parasomnias. It’s not just bad sleep. It’s a red flag.
Americans over-medicalize everything. Just lock the door. That’s it. No apps. No melatonin. No sleep diaries. Simple. Clean. No nonsense.