Ovarian Cancer Screening: What You Need to Know About Early Detection
When it comes to ovarian cancer screening, a process used to find ovarian cancer before symptoms appear, often using blood tests and imaging. Also known as ovarian cancer detection, it's not a simple checkup like a mammogram—it's complex, controversial, and only recommended for certain high-risk groups. Most women don't need regular screening because current methods aren't accurate enough to catch early-stage cancer without causing more harm than good through false alarms.
There are two main tools used in ovarian cancer screening, a process used to find ovarian cancer before symptoms appear, often using blood tests and imaging. Also known as ovarian cancer detection, it's not a simple checkup like a mammogram—it's complex, controversial, and only recommended for certain high-risk groups. Most women don't need regular screening because current methods aren't accurate enough to catch early-stage cancer without causing more harm than good through false alarms.
There are two main tools used in CA-125 blood test, a measure of a protein often elevated in ovarian cancer, but also raised by many non-cancer conditions like endometriosis or even menstruation and transvaginal ultrasound, an imaging test where a probe is placed in the vagina to look at the ovaries for abnormal growths. Neither is perfect. CA-125 can be high for reasons that have nothing to do with cancer, and ultrasounds often pick up harmless cysts that lead to unnecessary biopsies and stress. Together, they’re sometimes used for women with strong family histories or known genetic risks like BRCA mutations.
Women with Lynch syndrome, BRCA1 or BRCA2 gene changes, or a close relative who had ovarian cancer are the only ones for whom screening is seriously considered. Even then, studies show it doesn’t significantly reduce deaths from ovarian cancer. The biggest risk? Delaying real treatment because a false positive makes someone think they’re safe when they’re not—or rushing into surgery for something that isn’t cancer.
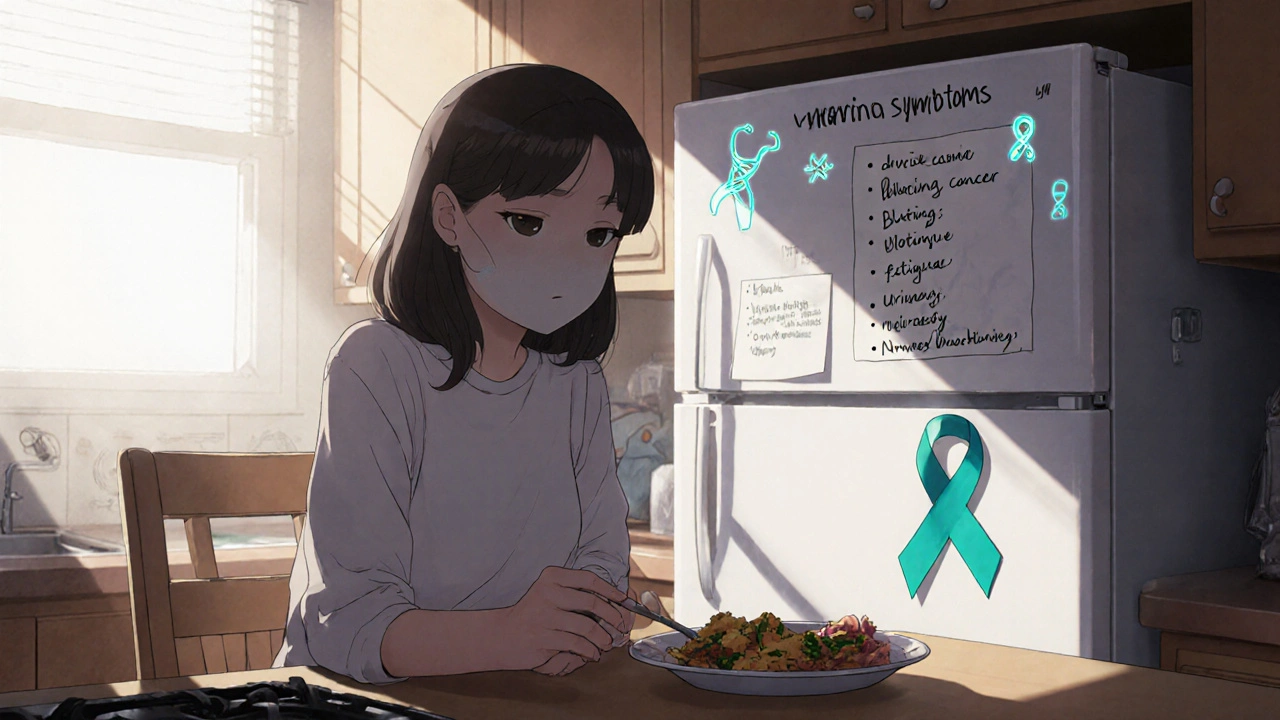
That’s why doctors focus more on ovarian cancer risk, factors like age, genetics, reproductive history, and hormone use that increase the chance of developing the disease than on screening. Knowing your family history, tracking symptoms like bloating, pelvic pain, or feeling full fast, and talking to a genetic counselor if you have a history of breast or ovarian cancer in your family are far more useful than routine screening for most people.
The posts below cover real-world stories and medical insights from women who’ve faced ovarian cancer, its treatments, and how genetics, medications, and lifestyle play into risk. You’ll find guides on genetic testing, how chemotherapy affects the body, what to ask your doctor if you’re high-risk, and how to interpret lab results like CA-125. This isn’t about pushing screening on everyone—it’s about giving you the facts so you can make smarter choices for your health, whether you’re at risk or just want to understand what’s out there.
Ovarian cancer is often silent until it's advanced. Learn the real symptoms, how to support someone diagnosed, and simple ways to help raise awareness and fund better early detection research.
Read more