Understanding Post-Traumatic Stress Disorder
Before we delve into the role of Carbamazepine in the treatment of Post-Traumatic Stress Disorder (PTSD), it's essential to understand what PTSD is and how it affects individuals. PTSD is a mental health disorder that can develop after a person has experienced or witnessed a traumatic event, such as war, assault, accidents, or natural disasters. The condition can cause intense anxiety, flashbacks, nightmares, and negative thoughts or emotions related to the traumatic event.
As someone who has personally witnessed the devastating effects of PTSD on friends and family, I can attest to the importance of finding effective treatments for this condition. In this article, I'll outline how Carbamazepine has been used to help individuals cope with PTSD symptoms and regain control over their lives.
What is Carbamazepine?
Carbamazepine is an anticonvulsant medication that was initially developed to treat epilepsy. Over time, it has also been found to be effective in treating other conditions, such as bipolar disorder and neuropathic pain. Carbamazepine works by stabilizing the electrical activity in the brain, thereby reducing the occurrence of seizures and mood swings.
Given its ability to regulate brain activity, researchers have begun to explore the potential of Carbamazepine in treating PTSD. In the sections that follow, we'll take a closer look at the evidence supporting its use in this context.
Carbamazepine and PTSD: The Research
The use of Carbamazepine for PTSD treatment has been a topic of interest for researchers in recent years. Several studies have explored its effectiveness in reducing PTSD symptoms, with promising results. For instance, a study conducted by the Department of Psychiatry at the University of California, San Diego, found that Carbamazepine significantly reduced PTSD symptoms in combat veterans.
Another study published in the Journal of Clinical Psychopharmacology showed that Carbamazepine was effective in reducing the intensity and frequency of flashbacks and nightmares in patients with PTSD. These findings suggest that Carbamazepine may be a valuable addition to the arsenal of treatments available for PTSD sufferers.
How Carbamazepine Helps to Manage PTSD Symptoms
Carbamazepine is believed to help manage PTSD symptoms by stabilizing mood and reducing anxiety. By regulating the electrical activity in the brain, Carbamazepine can help to prevent mood swings and reduce the severity of emotional reactions to triggers. This can be particularly helpful for individuals who experience intense anxiety or panic attacks as a result of their PTSD.
Additionally, Carbamazepine has been shown to reduce the occurrence of nightmares and flashbacks, which are common symptoms of PTSD. By reducing the frequency of these distressing experiences, individuals may find it easier to cope with their condition and work towards recovery.
Carbamazepine as an Adjunctive Treatment
It's important to note that Carbamazepine is not typically used as a standalone treatment for PTSD. Instead, it is often prescribed as an adjunctive therapy, meaning it is used alongside other treatments such as psychotherapy, medication, or both. This approach allows healthcare providers to tailor treatment plans to the unique needs of each individual, increasing the likelihood of successful outcomes.
In my own experience, I have seen loved ones benefit from a combination of medications, such as Carbamazepine, and evidence-based psychotherapies like cognitive-behavioral therapy (CBT) or eye movement desensitization and reprocessing (EMDR). This comprehensive approach to treatment can provide the support and tools needed to overcome PTSD.
Potential Side Effects of Carbamazepine
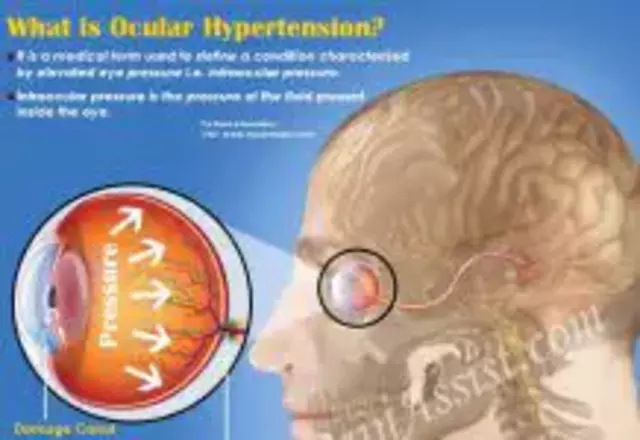
As with any medication, there are potential side effects associated with Carbamazepine use. Some common side effects include dizziness, drowsiness, nausea, and blurred vision. More serious side effects, such as an irregular heartbeat or severe skin reactions, can also occur, although they are less common.
It's essential for individuals to work closely with their healthcare providers when starting Carbamazepine or any other medication. Regular monitoring and communication can help to identify and address any side effects that may arise during treatment.
Carbamazepine and the Importance of Personalized Treatment
While Carbamazepine has shown promise in treating PTSD symptoms, it's essential to remember that each individual's experience with PTSD is unique. What works for one person may not be as effective for another. This is why it is crucial to work with a healthcare provider who can develop a personalized treatment plan based on an individual's specific needs and circumstances.
In my own journey to support loved ones with PTSD, I've learned that finding the right treatment can be a process of trial and error. Patience, persistence, and open communication with healthcare providers are key to finding the most effective treatment plan.
Conclusion
Carbamazepine has shown promise as an effective treatment option for individuals living with PTSD. Its potential to stabilize mood, reduce anxiety, and decrease the frequency of flashbacks and nightmares can offer much-needed relief for those struggling with this debilitating condition.
However, it's crucial to remember that each person's journey with PTSD is unique, and the most effective treatment plan will vary from individual to individual. By working closely with healthcare providers and exploring various treatment options, individuals with PTSD can find the support and tools they need to regain control over their lives.






Comments
Carbamazepine offers a unique angle on PTSD treatment by modulating neuronal firing patterns, which can ease hyperarousal. Its mood‑stabilizing properties echo some of the benefits we see with classic anxiolytics, yet it brings a different pharmacologic profile. For veterans who have tried multiple regimens, this drug sometimes fills a missing gap. While not a first‑line option, the evidence points to its potential as an adjunct. Overall, the creative repurposing of an epilepsy medication reflects the evolving landscape of psychiatric care.
Wow, who knew an epilepsy drug could double as a nightmare‑killer?
From a mechanistic standpoint, carbamazepine attenuates voltage‑gated sodium channel activity, which theoretically dampens the hyperexcitability underlying flashback circuitry. However, one must scrutinize the heterogeneity of study designs-small sample sizes, open‑label formats, and inconsistent dosing regimens raise validity concerns. Moreover, the drug’s pharmacokinetic interactions, especially with concurrent SSRIs, could confound observed outcomes. While some clinicians champion its off‑label use, the data still lack the robustness required for widespread endorsement. In short, the pharmacological rationale is intriguing, but the empirical foundation remains shaky.
Carbamazepine can be a useful adjunct, but it’s essential to monitor patients closely, especially regarding blood levels, and to watch for dermatologic reactions; the collaboration between psychiatrist and primary care is vital, and clear communication with the patient about possible side effects should never be overlooked.
When we examine the literature on carbamazepine for PTSD, it becomes evident that the methodology often varies dramatically, leading to a mosaic of outcomes that can be difficult to synthesize into a coherent narrative; in many of the trials, the dosing strategies were adjusted on an ad‑hoc basis, which may have introduced confounding variables that obscure the true efficacy of the compound, and while some participants reported a notable reduction in flashback frequency, others experienced only marginal improvements that did not reach statistical significance, thereby underscoring the necessity for larger, double‑blind, place‑controlled studies that can definitively ascertain the drug’s therapeutic potential within a rigorously defined cohort.
Listen, the mainstream media won’t tell you this, but every time a new drug gets pushed for PTSD, there’s a hidden agenda to pharma profit you down the line. Carbamazepine isn’t a miracle cure; it’s just another way for big corporations to keep us dependent on prescriptions. The side‑effects are downplayed, but you’ll hear rumors about heart issues and severe skin reactions that never make the headlines. They want us to think it’s safe because they’ve bought the research labs. Wake up and demand transparency before you let another pill dictate your life.
Okay, let’s talk about the drama of typo‑fighting these meds! Carbamazepine can actually quiet those night‑time terrors, which feels like a plot twist in a bad movie 🎬. But don’t forget, you still need therapy – it’s not a solo hero. I’ve seen people celebrate the “miracle pill” like it’s a winning lottery ticket 🎟️, then get hit with drowsiness the next day. So, enjoy the win, but keep the script realistic.
One might suggest that the integration of carbamazepine into PTSD protocols is nothing more than a fashionable fad, yet the empirical evidence, though modest, does present a certain allure for clinicians seeking a diversified pharmacopeia. It is, of course, entirely unsurprising that such a proposal would elicit a chorus of cautious optimism from those who revel in the novelty of repurposing established medications. Nevertheless, the hallmark of sound practice remains a diligent appraisal of risk‑benefit ratios, especially in a terrain as sensitive as trauma‑related pathology. In closing, one can only hope that future investigations will either substantiate or gracefully retire this therapeutic curiosity.
Look, if you’re a true patriot you’ll question why we keep shoving pills on our vets instead of fixing the system. Carbamazepine might help a few, but it’s a Band‑Aid on a bullet wound. We need real solutions, not just another “new” drug. Get the government to stop the pharmaceutical circus.
From a grammatical standpoint, the prescription guidelines for carbamazepine ought to be articulated with precision, ensuring that each clause adheres to syntactic correctness; any deviation could foster misinterpretation among clinicians. Moreover, the dosage titration schedule must be presented in a manner that reflects both clarity and conciseness, thereby minimizing the risk of prescribing errors. While the therapeutic promise is noteworthy, the discourse surrounding its usage should remain anchored in linguistic rigor. 🧠📚
Honestly, the whole carbamazepine hype feels like a pretentious attempt to sound cutting‑edge. It’s as if the author wanted to sprinkle buzzwords just to impress us. While there are some legit points, the drama around it is overblown. The drug isn’t a silver bullet, just another tool in the kit.
I’ve always thought the focus on carbamazepine is a bit misguided; the core issue lies in the lack of comprehensive care. Sure, it might dampen some symptoms, but without addressing underlying trauma through psychotherapy, the benefits are fleeting. The data isn’t conclusive enough to warrant a wholesale shift in treatment protocols. It’s worth considering alternative mechanisms before championing this drug.
From my perspective, carbamazepine can be part of the toolkit, but it shouldn’t dominate the conversation. I’ve seen patients who responded well, and others who didn’t notice much difference. The key is individualized assessment, and keeping expectations realistic.
I’ve been chatting with a few folks who have tried carbamazepine for PTSD, and the stories are surprisingly diverse.
Some say the medication helped tame the relentless flashbacks that used to hijack their evenings.
Others mention a subtle fog that settles over their thoughts, making concentration a bit of a slog.
What’s interesting is how the side‑effects, like occasional dizziness, seemed to fade once the dose was stabilized.
A lot of the success stories also highlight that the drug was never prescribed in isolation but paired with therapy, which seems to be a key factor.
I’ve noticed that patients who engaged in CBT alongside carbamazepine reported faster improvements than those who relied on pills alone.
There’s also the matter of monitoring blood levels, something that clinicians stress to avoid rare but serious skin reactions.
From a practical standpoint, the medication can be pricey, so insurance coverage becomes a real hurdle for many.
Nevertheless, the overall sentiment among the community I’ve observed feels cautiously optimistic.
Even the skeptics admit that, for a subset of veterans, carbamazepine opened a door that other treatments kept closed.
It’s also worth noting that lifestyle adjustments, like regular sleep patterns and low‑stress environments, amplify the benefits.
When I asked about long‑term outcomes, many reported that after a year the need for the drug either plateaued or tapered off safely.
On the flip side, there are anecdotes about withdrawal challenges if the medication is stopped abruptly, which underscores the need for physician guidance.
All in all, the dialogue I’ve been part of suggests that carbamazepine isn’t a silver bullet, but a valuable piece in a larger puzzle.
So whether you’re a patient, a caregiver, or a clinician, keeping an open mind and sharing experiences seems to be the best path forward.
Thanks for sharing such an in‑depth overview, Bobby. It’s encouraging to see the emphasis on combined therapy, as we know the synergy often yields better outcomes. I’d add that regular follow‑ups can help catch side‑effects early, keeping the treatment on track. Keep the conversation going – it helps everyone stay informed.
While the enthusiasm for carbamazepine is understandable, it’s crucial to remember the ethical responsibility of prescribing. The drug’s side‑effect profile, though manageable, includes rare but severe reactions that demand vigilant monitoring. Moreover, the narrative that a single medication can resolve complex trauma oversimplifies the human psyche. Patients deserve holistic care that integrates pharmacology, psychotherapy, and social support. Let’s not allow excitement to eclipse cautious, evidence‑based practice.
The discourse surrounding carbamazepine typifies the current trend of seeking pharmacological panaceas without sufficient scrutiny. The lexicon employed in many papers veers toward hyperbolic jargon, obscuring the modest efficacy signals present. While there is merit in exploring adjunctive agents, the prevailing hype risks relegating nuanced clinical judgment to the background. It’s imperative that we, as a community, maintain a critical lens and prioritize patient‑centered outcomes over industry‑driven narratives.