Ulcerative colitis is more than just a complex term; it's a condition that weaves itself into the fabric of daily life for many individuals. Most notably, it casts its shadow over the colon, leading to inflammation and ulcers along the digestive tract. But its reach is neither short nor contained. The ripples of this chronic disease frequently extend beyond, influencing multiple facets of an individual's health and well-being.
While the digestive system may bear the brunt of its assault, ulcerative colitis can trigger a cascade of effects across various bodily systems. Understanding these impacts forms a crucial part of managing the condition effectively. For those living with ulcerative colitis, knowing what to expect and how to tackle the challenges head-on is key to fostering a more comfortable and healthier life.
Recognizing the condition's broader implications, from nutritional deficiencies to the increased risk of complications like colorectal cancer, allows for informed decision-making and proactive care. Whether you're recently diagnosed or have been walking this path for years, exploring the comprehensive effects and strategies for management can empower you to lead a fulfilling life despite the hurdles ulcerative colitis may present.
- What is Ulcerative Colitis?
- Impact on Digestive Health
- Systemic Effects and Complications
- Nutritional Considerations
- Management and Lifestyle Tips
What is Ulcerative Colitis?
Ulcerative colitis (UC) is much more than a medical label; it is a chronic disease that intricately impacts those it touches. Imagine a world inside your body where inflammation becomes a relentless artist, painting ulcers along the innermost lining of your large intestine and rectum. This condition doesn't announce itself subtly; it comes with a symphony of symptoms that are hard to ignore. For many, it begins with a persistent abdominal discomfort and an urgency to run to the restroom. This restless dance with inflammation often leads to bloody stools, fatigue, and an unwelcome weight loss that's not from a new workout plan.
This inflammatory bowel disease (IBD) has a penchant for unpredictably flaring up and then retreating into periods of remission, only to raise its challenging head again. Unlike its relative Crohn's disease, which can affect any part of the gastrointestinal tract, ulcerative colitis restricts its boundaries to the colon and rectum. The inflammation it causes starts at the rectum and may extend continuously through the colon. While the exact cause remains a puzzle, experts speculate a combination of genetic factors, an overactive immune response, and environmental triggers play a significant role in its manifestation.
Delve deeper, and you'll find that ulcerative colitis doesn't discriminate against age or gender. It's a condition often diagnosed in young adults but can onset at any age. Dr. Bruce Sands, a well-respected gastroenterologist, once noted,
"Living with UC is akin to walking on a tightrope with unpredictability on one side and lifestyle adjustments on the other." This succinctly captures the essence of adapting to life with UC, where individuals must balance awareness with adaptation.
The journey to diagnosis involves a detailed exploration of symptoms, family history, and a series of medical tests. Blood tests may reveal anemia or infection, while stool samples can eliminate other vilified culprits. The most telling sign comes from the visual evidence obtained through a colonoscopy, where the internal landscape of your colon presents the true tale. As knowledge and awareness of UC grow, researchers strive to piece together this enigmatic puzzle. Knowledge, after all, is power, and with it, those living with UC can navigate their journey with understanding and resilience.
Impact on Digestive Health
Ulcerative colitis primarily takes its toll on the digestive system, an intricate network where the havoc it wreaks is multi-fold. The lining of the colon is where this condition makes its aggressive mark, leading to chronic inflammation and ulcers. Individuals living with this affliction often experience a spectrum of symptoms that include persistent diarrhea, abdominal pain, and rectal bleeding, all of which can fluctuate in intensity. The inflammation can extend from the rectum continuously through to the colon, resulting in a variety of health challenges and complications over time. One significant point to note is that the degree of inflammation and the specific sections of the colon involved can vary widely among sufferers, adding to the complexity of diagnosis and treatment.
An essential aspect of understanding ulcerative colitis is recognizing its pattern of flare-ups and remissions. These flare-ups can be unpredictable, sometimes occurring without clear triggers, although stress and dietary choices often play a part. During a flare, the inflammation is at its peak, and so too are the symptoms. This cycle can cause significant disruption, making daily life difficult for those affected. The chronic nature of this condition means that even when symptoms subside, the underlying issues within the colon remain. As a result, long-term management becomes a critical focus for those diagnosed with this chronic disease.
The impact of ulcerative colitis on digestive health is not limited to the colon. Over time, such chronic inflammation can alter the functionality of the digestive tract, affecting nutrient absorption and leading to a variety of deficiencies. This is not just a theoretical concern; evidence suggests that compromised nutrient absorption is a real issue for many individuals living with ulcerative colitis. Gradual reduction in the efficiency of digestive processes can leave individuals feeling fatigued and malnourished, even if their diet appears balanced and adequate. Thus, careful monitoring and possible dietary adjustments become integral to managing the ailment and its cascading effects on health.
"Ulcerative colitis significantly impacts the quality of life due to its persistent symptoms and need for ongoing management," says Dr. Jane Smith, a renowned gastroenterologist. "It's crucial to adopt a comprehensive approach to care, including diet, medication, and sometimes surgery."
Another significant consideration is the potential for more severe complications such as perforated colon or increased risk of colorectal cancer, especially in those with extensive colitis lasting for many years. This makes regular screening and vigilant management strategies indispensable. Treating ulcerative colitis often involves an integrated approach that addresses inflammation and symptom control, sometimes requiring the use of medications like aminosalicylates, corticosteroids, or biologics. For some, surgical intervention may eventually be necessary to alleviate persistent, severe symptoms or complications that don't respond to medical therapies. Regular consultation with healthcare providers and staying informed about the latest treatment options is key to navigating the challenges posed by this condition.

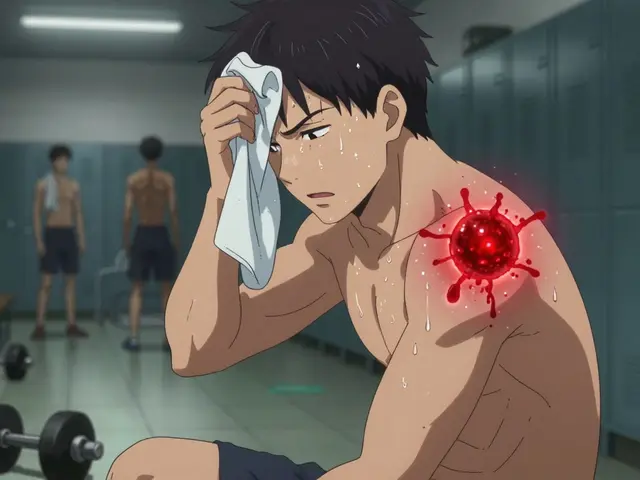
Systemic Effects and Complications
Living with ulcerative colitis goes beyond managing digestive health; it encompasses a range of systemic effects that ripple throughout the body. While the primary battle is fought in the colon, it's important to understand that this chronic ailment can disrupt multiple body systems. One of the intricate ways it does so is by affecting the body's ability to absorb essential nutrients, potentially leading to deficiencies over time. This impact on nutritional absorption can usher in a variety of symptoms. Among these are fatigue, weakness, and an increased susceptibility to infections, as the immune system often undergoes its own challenges.
Moreover, individuals with ulcerative colitis may experience joint pain and inflammation, a condition known as enteropathic arthritis. This occurs because the same inflammatory response that targets the intestine can sometimes affect joints, causing discomfort and contributing to reduced quality of life. The skin isn’t exempted either; skin conditions such as erythema nodosum and pyoderma gangrenosum may arise, further indicating the disease's potential to affect beyond the digestive tract. These conditions serve as a reminder that ulcerative colitis isn't just a localized disease but a systemic challenge.
Hormonal imbalances also come into play, often influenced by prolonged use of medications like steroids commonly prescribed to manage flare-ups. Steroids can lead to complications like weak bones or osteoporosis and might even affect the adrenal glands. Additionally, patients often find themselves at a higher risk for conditions such as liver disease. Specifically, primary sclerosing cholangitis—a progressive disease of the bile ducts—has connections to ulcerative colitis, illustrating the depth of its systemic reach. In fact, while discussing these extensive connections, the consensus echoes, as a study from the National Institute of Diabetes and Digestive and Kidney Diseases noted, "The systemic nature of ulcerative colitis requires comprehensive care strategies beyond typical gastrointestinal treatments."
The cardiovascular system isn’t immune from the indirect assault of ulcerative colitis either. Some studies suggest an increased risk of blood clots and cardiovascular issues, potentially due to the chronic inflammation that is part and parcel of the disease. This underscores the importance of routine check-ups and a heart-healthy lifestyle, even in the face of a predominantly gastrointestinal disorder. From an emotional perspective, the chronic nature of ulcerative colitis often brings about psychological stress and anxiety, further influencing the course of the disease. It's not uncommon for individuals to experience these challenges, highlighting the importance of mental health care as a crucial component of managing systemic complications.
To encapsulate the systemic effects and unexpected complications of ulcerative colitis, the journey involves a multidisciplinary approach. Addressing these diverse impacts requires collaboration among gastroenterologists, rheumatologists, dermatologists, and mental health professionals to tailor a personalized treatment plan. Through understanding these far-reaching implications, one can navigate the complexities of ulcerative colitis with informed decisions and holistic care. Emphasizing the importance of awareness and proactive management, patients and caregivers alike can engage in strategies that mitigate the systemic burdens of this chronic condition.
Nutritional Considerations
Addressing the nutritional needs of individuals living with ulcerative colitis is just as important as managing the physical symptoms of the disease. Since this chronic inflammatory condition affects the colon and disrupts digestion, it often leads to complications such as malnutrition and nutrient deficiencies. Understanding and adjusting one's diet becomes crucial to not only improve digestive comfort but also to ensure that the body receives the necessary nutrients for overall health and well-being. Many patients report that maintaining a balanced diet not only helps alleviate symptoms but also enhances their quality of life. It is beneficial to focus on foods that are easier to digest and less likely to exacerbate symptoms, while avoiding items that trigger inflammation.
Research points to a few general dietary patterns that are often beneficial, though individual needs can vary. Typically, a diet low in fiber is recommended during flare-ups, as high-fiber foods can irritate the already sensitive colon lining. Highly processed foods, sugary treats, and items rich in dairy tend to be problematic for many, making it best to limit their intake. Emphasizing lean proteins, simple carbohydrates, and healthy fats can contribute positively to well-being. Crucially, developing a personalized diet plan should involve discussions with healthcare professionals who understand the intricacies of long-term effects on health when living with ulcerative colitis.
"Diet plays a fundamental role in managing ulcerative colitis. While there's no one-size-fits-all diet, working with a dietitian knowledgeable about inflammatory bowel diseases can tailor a plan that respects individual tolerances and nutrition goals," notes Dr. Jane Andrews, a leading gastroenterologist.
A common complication associated with ulcerative colitis is an increased risk of developing osteoporosis, primarily due to reduced absorption of calcium and vitamin D. It's essential to incorporate food items or supplements rich in these nutrients. Salmon, fortified plant milks, and leafy greens can be good sources to consider. Moreover, since flare-ups can lead to dehydration, maintaining adequate fluid intake is vital. Water, herbal teas, and diluted fruit juices are typically easier on the gut. On the flip side, caffeinated or carbonated beverages may not be as kind, prompting some to avoid them altogether.
Practical Nutritional Tips
For those new to navigating their diet with ulcerative colitis, starting with smaller, more frequent meals might feel more manageable compared to larger meals, which often overwhelm the digestive system. While fresh fruits and vegetables are generally part of a healthy diet, cooking them or choosing canned versions can reduce their fiber content, thus making them more suitable options during the flare-up periods. Reading labels carefully can also prevent accidental consumption of irritating preservatives or additives. While it may seem daunting, adopting a mindful approach to nutrition can significantly contribute to managing both the immediate and long-term effects of ulcerative colitis.

Management and Lifestyle Tips
Living with ulcerative colitis requires a combination of vigilant management and thoughtful lifestyle choices. Given the chronic nature of this condition, establishing a routine centered around health maintenance and proactive care can profoundly affect daily well-being. One fundamental component is medication adherence. Consulting a healthcare provider to tailor a medication regimen individualized to one’s symptoms can help in managing flare-ups and maintaining remission. Routine check-ups are not just precautionary; they provide insights into the current state of the disease and offer opportunities to adjust treatments and prevent complications.
Diet plays a pivotal role in managing ulcerative colitis. While no universal 'ulcerative colitis diet' exists, identifying food triggers and adopting a balanced diet can aid in symptom management. Nutritional adjustments often involve eliminating foods that irritate the intestinal lining, such as nuts and seeds, while incorporating more of those that are soothing like oatmeal and yogurt. Keeping a food diary has proven helpful for many, as it allows one to track correlations between food intake and symptoms. An often-recommended approach is the low FODMAP diet, which minimizes specific carbohydrates linked to digestive distress. Seeking advice from a registered dietitian can further refine dietary choices and ensure nutritional needs are met.
Stress reduction is another vital component. It's now well-recognized that stress can exacerbate symptoms of ulcerative colitis. Techniques such as yoga, meditation, and gentle exercise like walking or swimming can help maintain a calm state of mind. Regular physical activity not only boosts mental health but also enhances the immune system, which is crucial for those with an immune-mediated condition. Mind-body practices such as mindfulness and cognitive-behavioral therapy (CBT) are not just new-age jargon; they provide tangible benefits by reshaping the body's biological response to stress.
As emphasized by Dr. John D. Reveille, a renowned gastroenterologist, "Understanding the balance between medication, lifestyle, and nutrition is crucial for effective management. A multi-pronged approach often yields the best results."
Community support can’t be overlooked. Engaging with support groups offers emotional solace and information exchange that is invaluable. Whether through online forums or in-person meet-ups, connecting with others who understand the challenges of ulcerative colitis can inspire shared coping strategies and provide a sense of belonging. Additionally, educating family members and friends about the condition ensures that social interactions remain supportive and stress-free.
Last but not least, practical adjustments in daily life make a difference. From planning trips with knowledge of restroom locations to organizing workspaces for comfort during flare-ups, these small modifications cater to well-being and minimize stress. Personal planning, combined with healthcare support, dietary mindfulness, and an active lifestyle, crafts a comprehensive blueprint for effectively managing ulcerative colitis. Remember, every step towards management is a step towards a more empowered life.






Comments
Reading through the overview, it becomes clear that ulcerative colitis isn’t just a gut issue. The way it can touch nutrition, joints, and even mood shows how interconnected our bodies are. Managing it means looking beyond the colon and paying attention to the whole system. Small lifestyle tweaks often have outsized effects over time. Staying aware of patterns can turn a reactive stance into a proactive one.
I hear you, Jonathan. It’s tough when a condition spills over into other parts of life. One thing that helped me was keeping a simple log of what I ate and how I felt. Over weeks, I could spot which foods made flare‑ups worse and which ones were safe. Pairing that with regular check‑ups gave my doctor clearer data to adjust meds. Also, gentle walks after meals helped my digestion settle. It’s a slow process but being consistent makes a difference.
Understanding the broader impacts of ulcerative colitis is essential for anyone living with it. Nutrition, joint health, and mental well being all play a part in the overall picture. Simple steps like a balanced diet and regular low‑impact exercise can keep many complications at bay. It’s also valuable to talk openly with a care team about any new symptoms. Staying informed empowers you to make better choices.
Deborah, you nailed the need for a holistic view, but let’s dig deeper into why people ignore the big picture. Most think of ulcerative colitis as merely a bathroom issue, yet it’s a silent puppeteer tugging at the immune system, the bones, and even the heart. When the gut inflames, cytokines spill into the bloodstream like angry ambassadors, prompting joints to ache and the liver to protest. That’s why you’ll see enteropathic arthritis showing up in some patients – the same fire that burns the colon also sparks inflammation elsewhere.
Now, imagine you’re trying to live a normal life while your body is constantly flashing red alerts. The stress response kicks in, cortisol spikes, and you end up with hormonal imbalances that can erode bone density. Long‑term steroid use, while calming the fire, is like using gasoline to put out a grease fire – it can lead to osteoporosis and even mask underlying issues.
But here’s the kicker: the mind isn’t immune to this chaos. Chronic pain and unpredictable flare‑ups breed anxiety, which in turn can worsen inflammation – a vicious feedback loop. Breaking that cycle demands more than just medicine; it requires mindfulness, community support, and a diet that respects the gut’s delicate ecosystem.
So, what’s the actionable takeaway? First, get screened regularly for colon cancer and liver complications; early detection saves lives. Second, collaborate with a multidisciplinary team – gastroenterologists, rheumatologists, dietitians, and mental health professionals. Third, track your symptoms, diet, and mood in a unified journal; data is power. And finally, adopt a heart‑healthy routine: omega‑3 rich foods, moderate exercise, and stress‑reducing hobbies. By treating ulcerative colitis as a system‑wide challenge rather than a localized nuisance, you reclaim agency over your health.
Remember, you’re not alone – support is just a click away 😊.