Ovarian Cancer Screening Planner
Personalize Your Screening Schedule
Enter your information below to get personalized recommendations for ovarian cancer screenings.
Enter your details and click "Get My Screening Plan" to see personalized recommendations.
Ovarian cancer often hides until it’s too late, but a simple habit-seeing a doctor regularly-can change that. This article explains how gynecological exams fit into ovarian cancer prevention, what tests are involved, and how you can take charge of your health today.
Key Takeaways
- Ovarian cancer symptoms are vague; routine exams catch changes early.
- Screening tools include Pap smears, transvaginal ultrasound, and CA‑125 blood tests.
- Women with a family history or BRCA mutation should start exams at age 25‑30.
- Annual visits for ages 21‑40, then every six months after 40, meet most guidelines.
- After an abnormal result, timely follow‑up with a gynecologic oncologist is essential.
Ovarian Cancer: The Silent Threat
In 2024, the Australian Institute of Health reported about 1,200 new ovarian cancer cases nationwide, with a five‑year survival rate hovering around 45%. The low survival rate isn’t because the disease is untreatable; it’s because it’s usually discovered at an advanced stage. Early‑stage ovarian cancer may present as a slight increase in abdominal bloating, mild pelvic discomfort, or subtle changes in menstrual patterns-signs many women dismiss as normal.
How Regular Gynecological Exams are comprehensive health checks that assess the reproductive system, including the uterus, cervix, vagina, and ovaries Spot Early Warning Signs
A routine exam goes beyond a quick visual check. Your clinician performs a pelvic examination, inspects the cervix, and may order imaging or blood tests based on risk factors. By creating a baseline of what’s normal for you, doctors can notice even minor deviations that could signal early disease.

Recommended Screening Schedule
The Australian Cancer Society suggests the following timetable:
- Age 21‑40: Annual exam, even if you’re not sexually active.
- Age 41‑50: Every 12months, with the option to add an ultrasound if you have risk factors.
- Age 51+: Every 6‑12months, especially if you have a family history of ovarian or breast cancer.
Women who carry a BRCA mutation a genetic alteration that significantly increases the risk of breast and ovarian cancers or have a strong family history should begin screening at 25‑30 years and may need more frequent monitoring.
Core Tools Used During the Exam
Three main tests help clinicians evaluate ovarian health:
- Pap smear a sample of cervical cells examined for abnormalities
- Transvaginal ultrasound an imaging technique that visualizes the ovaries and uterus from inside the vagina
- CA‑125 blood test measures a protein that’s often elevated in ovarian cancer patients
| Test | Primary Use | When It’s Recommended | Pros | Cons |
|---|---|---|---|---|
| Pap smear | Cervical cell abnormalities | Every 3years (21‑65) or as part of routine exam | Simple, low cost, catches precancerous lesions | Doesn’t directly screen ovaries |
| Transvaginal ultrasound | Visualize ovarian size, cysts, masses | High‑risk women or abnormal pelvic findings | Detects structural changes early | Operator‑dependent, may find benign cysts |
| CA‑125 blood test | Biomarker for ovarian cancer | Women with family history or after menopause | Non‑invasive, useful for monitoring | Elevated in many benign conditions |
Understanding Personal Risk Factors
Not every woman faces the same risk. Key factors that push your odds higher include:
- First‑degree relative with ovarian or breast cancer.
- Known BRCA1 or BRCA2 gene mutation.
- Long menstrual cycle history (early menarche, late menopause).
- Endometriosis or previous pelvic inflammatory disease.
- Obesity and a sedentary lifestyle.
If you tick any of these boxes, discuss them openly with your doctor. They’ll tailor the screening interval and may suggest preventive measures such as risk‑reducing surgery or chemoprevention.

Preparing for Your Appointment
Feeling nervous is normal, but a little preparation can make the visit smoother:
- Write down any pelvic or abdominal symptoms, no matter how mild.
- Bring a list of medications, supplements, and past surgeries.
- Know your family cancer history-names, ages at diagnosis, and type of cancer.
- Prepare questions: "Should I have a transvaginal ultrasound this year?", "When should we check CA‑125?"
- Wear comfortable clothing; you’ll likely be asked to undress from the waist down.
Clinics often have patient portals where you can upload your family history beforehand, saving time and letting the clinician focus on the exam itself.
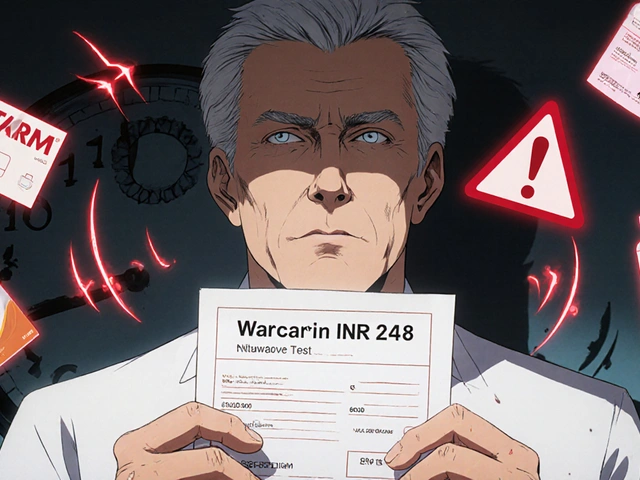
If an Abnormal Result Pops Up
Abnormal doesn’t mean cancer, but it does mean a closer look is needed. Typical next steps:
- Repeat testing after a few weeks to see if the result normalizes.
- Referral to a gynecologic oncologist a specialist trained in diagnosing and treating cancers of the female reproductive system for advanced imaging or biopsy.
- Additional imaging such as MRI or CT if a mass is identified.
- Genetic counseling if a hereditary pattern is suspected.
Early intervention after an abnormality dramatically improves outcomes. The key is staying on top of follow‑up appointments and not delaying further tests.
Lifestyle Habits That Boost Prevention
While exams are the front line, healthy habits reinforce their impact:
- Maintain a healthy weight-studies show obesity can raise ovarian cancer risk by up to 20%.
- Engage in regular physical activity (150minutes of moderate exercise per week).
- Limit alcohol intake to less than two drinks per week.
- Eat a diet rich in fruits, vegetables, and whole grains; antioxidants may protect ovarian cells.
- Consider oral contraceptives if appropriate-they have been linked to a reduced ovarian cancer risk.
Combine these habits with consistent gynecological exams, and you’re building a solid defense against ovarian cancer.
Frequently Asked Questions
How often should I get a transvaginal ultrasound?
For most women with average risk, an ultrasound isn’t routine. High‑risk women (family history, BRCA carriers) usually have it every 1‑2years, but your doctor will set the exact interval based on your personal profile.
Can a Pap smear detect ovarian cancer?
No. A Pap smear screens the cervix, not the ovaries. However, during the same visit the clinician can perform a pelvic exam and decide if additional ovarian screening is needed.
What does an elevated CA‑125 mean?
CA‑125 can rise for many reasons-ovarian cancer, endometriosis, pelvic inflammatory disease, even pregnancy. It’s a flag, not a diagnosis, so doctors follow up with imaging or specialist referral.
Should I start screening earlier if I have a family history?
Yes. Women with a first‑degree relative who had ovarian or breast cancer are advised to begin examinations at age 25‑30, often with yearly ultrasounds and CA‑125 tests.
What if I’m not sexually active-do I still need a gynecological exam?
Absolutely. Exams assess organ health, not sexual activity. Regular pelvic checks help catch conditions like ovarian cysts, fibroids, and early‑stage cancers regardless of activity level.
Staying proactive with regular gynecological exams is one of the smartest moves you can make for ovarian cancer prevention. Pair that habit with awareness of risk factors, the right screening tools, and a healthy lifestyle, and you’ll give yourself the best chance at catching any trouble early.






Comments
Regular check‑ups are the cheapest way to catch problems early. Even if you feel fine, a pelvic exam can spot subtle changes before they turn serious.
From a clinical epidemiology standpoint, the sensitivity of transvaginal ultrasonography combined with serial CA‑125 quantification yields a higher positive predictive value in BRCA‑positive cohorts, especially when stratified by age‑specific incidence curves.
The exams aren’t just about pap smears; they give a baseline for the ovaries, uterus and cervix, which is essential for early detection.
Think of a regular gyn visit like a car’s oil change – you don’t wait for the engine to sputter before you take it in. Every year, a quick pelvic exam creates a reference point for what’s normal in your body. When you have risk factors like a BRCA mutation or a family history, that reference point becomes critical for spotting tiny changes early. A transvaginal ultrasound can visualize the ovaries in real time, catching cysts or masses that you’d never feel. The CA‑125 blood test adds another layer, flagging biochemical shifts that might precede imaging findings. Together, they form a safety net that catches issues before they become symptomatic. Early‑stage ovarian cancer has a dramatically better five‑year survival rate – often above 70 % – compared to the dismal numbers for late‑stage disease. That improvement isn’t magic; it’s the result of early intervention guided by routine screening. Even if you’re feeling perfectly fine, the exam can uncover things like endometriosis or benign cysts that could cause problems later. Addressing those early can spare you from more aggressive surgeries down the line. For women over 40, the interval tightens to every six to twelve months, because risk climbs with age. If you’re on oral contraceptives, that can actually lower your odds, but you still need the physical exam to monitor other health aspects. Lifestyle tweaks – maintaining a healthy weight, staying active, limiting alcohol – amplify the benefits of screening. Think of it as a partnership: your doctor provides the tools, and you bring the commitment to show up. Skipping appointments is like leaving a window open during a storm – you’re inviting trouble in. So schedule that appointment, write down any vague symptoms, and keep the conversation open. Your future self will thank you.
I cant stress enough how important it is to stay on top of those gyn visits, especially if you got a famiy history or any high‑risk genes. The docs will ask about smal l symptoms that many of us brush off, like slight bloating or a weird change in your cycle. Those tiny clues are often the first red flags. Also, dont forget to bring a list of any meds or supplements – even over‑the‑counter stuff can affect test results. If you’re worried about the transvaginal ultrasound being uncomfortable, just remember it’s quick and the benefits far outweigh the brief discomfort. And yeah, the CA‑125 test can be triggered by non‑cancer things, but that’s why doctors interpret it alongside imaging. So dont panic if you get a borderline result – it’s a cue to dig deeper, not a death sentence. Keep a log of any symptoms, however minor, and share it at your next appointment. That habit alone can make a huge difference in early detection.
Sticking to a regular schedule is the best thing you can do for peace of mind. Even if you’re anxious about exams, think of them as a proactive step toward a healthier future. You’ll feel empowered knowing you’re catching any issues early.
Just get the exam done – it’s worth it.
It’s easy to forget these appointments when life gets busy, but a quick check‑up can prevent a lot of worry later on.
Honestly, the medical industry pushes these screenings to line their pockets more than to save lives. Most women could skip the pricey ultrasounds and still be fine.
Thanks for the clear breakdown! I’ll definitely talk to my doctor about setting up a personalized plan.
The guidelines are straightforward: annual exams until 40, then semi‑annual.
From a clinical perspective, combining physical examination with targeted imaging and biomarkers provides the most comprehensive risk assessment. If you have a known BRCA mutation, start screening at 25 and consider annual ultrasounds and CA‑125 checks. For average‑risk women, annual exams are sufficient until age 40, after which a six‑month interval is advisable. Maintaining a symptom diary can also help your provider identify subtle changes early.
It is evident that the mainstream medical narrative deliberately downplays the potential harms of over‑screening, while subtly urging the populace toward unnecessary procedures. According to independent investigations, a considerable fraction of the funding allocated for ovarian cancer screening is diverted to pharmaceutical lobbying, thereby compromising the integrity of public health recommendations. Consequently, individuals must remain vigilant, question official guidelines, and seek independent counsel when making health decisions.