Standing up from a chair and feeling dizzy? That’s not just aging-it could be orthostatic hypotension, a dangerous side effect of blood pressure meds in older adults. It’s more common than you think. About 1 in 5 seniors on hypertension drugs experience a sudden drop in blood pressure when they stand, leading to falls, fractures, and hospital visits. The scary part? Many doctors still think lowering blood pressure too much causes this. But the truth is the opposite.
What Exactly Is Orthostatic Hypotension?
Orthostatic hypotension happens when your blood pressure drops at least 20 mm Hg systolic or 10 mm Hg diastolic within three minutes of standing. Your body normally adjusts by tightening blood vessels and speeding up your heart to keep blood flowing to the brain. But in older adults, that system slows down. Baroreflexes don’t respond as quickly. Blood vessels lose elasticity. The heart doesn’t pump as forcefully. And if you’re on certain blood pressure medications, it gets worse.This isn’t just a nuisance. Falls from dizziness are the leading cause of injury-related deaths in people over 65. Every year, over 3 million older adults visit the ER because of falls-and many of those are tied to blood pressure meds. Yet, many patients and providers still treat the symptom (low BP on standing) by reducing the medication, not realizing that might make their heart disease risk worse.
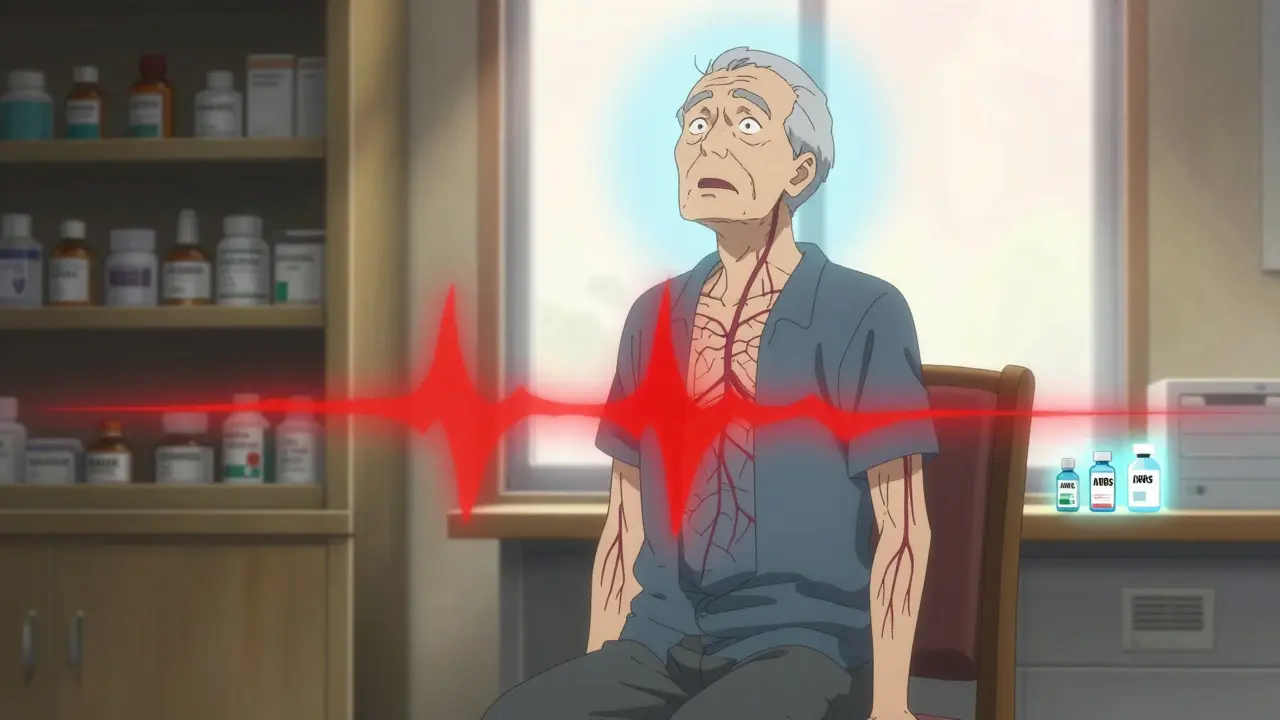
Which Blood Pressure Meds Are Riskiest?
Not all blood pressure drugs are created equal when it comes to orthostatic risk. Some are safer than others, especially for seniors.- Alpha blockers (like doxazosin, terazosin) carry the highest risk-up to 28% of seniors on these drugs develop orthostatic hypotension. They relax blood vessels too much, all at once.
- Beta-blockers (like metoprolol, atenolol) double or even triple the risk, especially sustained-release versions. They slow the heart’s ability to compensate when standing.
- Diuretics (like hydrochlorothiazide) can cause dehydration and low blood volume, making dizziness worse, especially if taken late in the day.
- Central sympatholytics (like clonidine) and tricyclic antidepressants also show strong links to dizziness and falls.
On the other hand, some medications are actually safer-or even protective:
- ACE inhibitors (like lisinopril) and ARBs (like losartan) have the lowest risk. Studies show they reduce orthostatic hypotension by 14-15% compared to other classes. They work gently on blood vessels without sudden drops.
- Amlodipine and isradipine (calcium channel blockers) are better tolerated than diltiazem or verapamil. Their slow action means less of a sudden drop in pressure.
Here’s the bottom line: If you’re over 65 and taking doxazosin or metoprolol for high blood pressure, talk to your doctor about switching. There’s strong evidence that replacing them with an ARB or amlodipine cuts dizziness and falls by up to 65% in real-world practice.
More Aggressive BP Control? It Might Help
Here’s the counterintuitive part: trying harder to lower your blood pressure doesn’t increase your risk of orthostatic hypotension-it may actually lower it.The SPRINT trial, which followed over 9,000 adults over 50 with high blood pressure, split them into two groups: one aiming for a systolic BP under 120, the other under 140. Many expected the tighter group to have more dizziness. But guess what? Both groups had nearly the same rate of orthostatic hypotension: 14.7% vs. 14.5%. Meanwhile, the tighter group had 25% fewer heart attacks, strokes, and heart failure episodes.
A follow-up analysis of nine trials involving nearly 18,500 people confirmed this: aggressive blood pressure control reduced orthostatic hypotension risk by 17%. Why? Because consistent, steady control prevents the wild swings in pressure that trigger dizziness. When BP is stable, your body adapts. When it’s spiking and crashing, your system gets confused.
So if your doctor says, “We’re lowering your meds because you get dizzy when you stand,” ask: “Is it the medication, or is it the inconsistency?” Often, the fix isn’t less medicine-it’s better timing and smarter choices.

When to Stop or Switch Medications
The American Geriatrics Society Beers Criteria updated in 2023 says clearly: avoid alpha blockers and certain beta-blockers in seniors with a history of falls or orthostatic symptoms. That’s not a suggestion-it’s a clinical red flag.But stopping meds cold is dangerous. If you’ve been on a high-risk drug for years, your body may have adapted to higher baseline pressure. Suddenly removing it can cause rebound hypertension, which is even riskier.
Here’s how to do it right:
- Review all meds-including antidepressants, pain pills, and over-the-counter sleep aids. Many contain hidden antihypertensive effects.
- Switch slowly. Replace an alpha blocker with an ARB over 4-6 weeks. Monitor BP in both lying and standing positions weekly.
- Time your doses. Take diuretics and long-acting meds no earlier than 3 hours before bedtime. This avoids nighttime drops and morning dizziness.
- Check for interactions. Mixing blood pressure meds with erectile dysfunction drugs (like sildenafil) or nitrates can cause dangerous drops.
Don’t wait for a fall to act. If you’ve had one dizzy spell after standing, it’s a warning sign-not just an annoyance.
Non-Medication Fixes That Actually Work
Medication changes are key-but they’re not the whole story. Simple habits can cut your risk of dizziness by half.- Stand up slowly. Sit on the edge of the bed for 30 seconds before standing. Pause again before walking.
- Hydrate before meals. Blood pools in your gut after eating, which can drop BP. Drink 16 oz of water 15 minutes before breakfast or dinner.
- Wear compression stockings. These help push blood back up from your legs. Studies show they reduce dizziness in 60% of seniors with orthostatic hypotension.
- Avoid alcohol and hot showers. Both dilate blood vessels and make dizziness worse.
- Exercise regularly. Walking 30 minutes a day strengthens your cardiovascular system and improves baroreflex sensitivity. You don’t need to run-just move.
These aren’t “nice-to-haves.” They’re essential. Many seniors who stick to these habits see improvement in 2-4 weeks. No new pills. No side effects. Just better control.
What About Medications for OH Itself?
Sometimes, you can’t avoid the dizziness entirely. In those cases, doctors may prescribe drugs to treat orthostatic hypotension directly:- Midodrine (Orvaten): Tightens blood vessels. Works fast but can cause high BP when lying down.
- Droxidopa (Northera): Boosts norepinephrine. Effective but expensive and can cause headaches.
- Fludrocortisone: Retains salt and water. Risk of swelling and heart strain.
- Pyridostigmine (Mestinon): Helps nerves signal better. Lower risk, often used in combination.
These are not first-line treatments. They’re for people who’ve tried everything else and still fall. Most seniors do better with medication switches and lifestyle changes alone.
What You Should Ask Your Doctor
Don’t leave your safety to chance. Bring these questions to your next appointment:- “Which of my blood pressure meds is most likely causing dizziness when I stand?”
- “Can we switch me to an ARB or amlodipine instead?”
- “Should I check my BP lying down and standing up at home?”
- “Am I taking any other meds that could make this worse?”
- “Is my BP target too aggressive for my age and balance?”
If your doctor dismisses your dizziness as “just getting older,” get a second opinion. You deserve to live without fear of falling.
The Future Is Personalized
New research is already changing the game. Two drugs in Phase II trials are designed to release medication only when you’re standing-keeping your BP steady no matter your position. That’s not sci-fi-it’s coming by 2028.Right now, the best tool you have is awareness. Know your meds. Know your risks. Know your body. And don’t accept dizziness as normal. With the right changes, you can control your blood pressure without losing your balance.
Can blood pressure meds cause falls in older adults?
Yes. Certain blood pressure medications-especially alpha blockers, beta-blockers, and diuretics-can cause orthostatic hypotension, a sudden drop in blood pressure when standing. This leads to dizziness, lightheadedness, and falls. About 3-26% of older adults on these drugs experience this. Switching to safer options like ARBs or amlodipine can reduce fall risk by up to 65%.
Is it safe to lower blood pressure aggressively in seniors?
Yes, if done correctly. The SPRINT trial and multiple meta-analyses show that targeting a systolic BP under 120 mm Hg does not increase orthostatic hypotension risk and actually reduces it by 17%. Aggressive control prevents dangerous BP swings, which are more harmful than steady, low pressure. The key is choosing the right meds and monitoring carefully.
Which blood pressure meds are safest for seniors with dizziness?
ACE inhibitors (like lisinopril) and ARBs (like losartan) have the lowest risk of causing orthostatic hypotension. Among calcium channel blockers, amlodipine and isradipine are better than diltiazem or verapamil. Avoid alpha blockers (doxazosin), beta-blockers (metoprolol), and diuretics if dizziness is a problem. Always switch under medical supervision.
Should I stop my blood pressure meds if I get dizzy?
No. Stopping suddenly can cause rebound high blood pressure, increasing heart attack or stroke risk. Instead, talk to your doctor about switching to a safer medication. Most dizziness improves within 2-4 weeks after changing drugs and adding lifestyle changes like slow standing and hydration.
Can lifestyle changes help with orthostatic hypotension?
Absolutely. Standing slowly, drinking 16 oz of water before meals, wearing compression stockings, avoiding alcohol and hot showers, and walking 30 minutes daily can reduce dizziness by up to 50%. These changes work better than most medications and have no side effects. Many seniors see improvement in just 2-4 weeks.





Comments
This is just Big Pharma pushing pills to keep people dependent. They don't care if you fall-they care if you keep buying meds. I've seen 70-year-olds on 12 different drugs. One day they're fine, next day they're in a wheelchair. Coincidence? I think not.
The data is statistically significant but methodologically flawed. You're conflating pharmacokinetic profiles with neuroautonomic resilience without accounting for polypharmacy confounders. The SPRINT trial's exclusion criteria invalidated its generalizability to frail elderly populations. This is reductionist medicine at its finest.
I've been standing up slowly for three months now... and I swear, it's changed my life. I used to need a cane. Now I dance with my grandkids. No pills. Just awareness.
Let me be clear: the medical establishment has been systematically ignoring the baroreflex dysfunction in geriatric populations since the 1980s. The fact that you're only now acknowledging this is evidence of institutional stagnation. Alpha-blockers were never meant for seniors-this was a regulatory failure disguised as clinical practice.
Canada's been doing this right for decades. We don't throw beta-blockers at seniors like candy. We assess, we adjust, we respect the body's wisdom. This post? It's what happens when American medicine forgets it's supposed to heal, not monetize.
I love how this doesn't just list drugs but explains why they work-or don't. My mom switched from metoprolol to losartan last year and hasn't stumbled since. It's not magic. It's science. And it's available to anyone who asks the right questions.
i read this and was like... wait so i dont have to be dizzy all the time?? like... wow. my granpa was on doxazosin for 5 years and no one ever said anything. this is wild.
I'm a nurse and I see this every day. Families come in panicked because Grandma fell. They think it's 'just old age.' But when we check meds? 80% of the time it's a drug interaction or timing issue. This post? It's the kind of thing we wish every patient read before their appointment.
My dad’s from Nigeria. He didn’t believe in pills until he started taking amlodipine. Now he walks 5K steps every morning. He says, 'If your body can adapt, let it adapt-with help, not harm.' Simple. Wise. Real.
I’ve spent 20 years working in geriatric care, and this is the most accurate, compassionate, and actionable summary I’ve ever seen. The non-pharmacological interventions-hydration, compression stockings, slow standing-are not 'adjuncts.' They are foundational. We’ve been treating symptoms instead of systems. This changes everything.
The real question isn't which drug to take-it's whether we've forgotten how to listen to the body's signals. Orthostatic dizziness isn't a side effect-it's a message. And we've been silencing it with more pills instead of asking why it's there. The body doesn't lie. We just stopped hearing it.