Survivorship Follow-up Schedule Calculator
This tool helps you create a personalized follow-up care schedule based on your treatment type and cancer type. Use it to track your next appointments and monitor late effects.
Your Follow-up Schedule
Important: This timeline is based on general guidelines. Your healthcare team may recommend adjustments based on your individual case.
Finishing cancer treatment feels like crossing a finish line, but the race doesn’t end there. The years that follow bring new routines, lingering side effects, and a whole set of appointments you didn’t expect. Below are proven, easy‑to‑apply tips that help you stay healthy, confident, and in control after a carcinoma diagnosis.
Key Takeaways
- Set a personalized follow‑up schedule with your oncology team and primary doctor.
- Incorporate moderate physical activity most days to boost energy and lower recurrence risk.
- Focus on whole‑food nutrition rich in plant protein, fibre, and antioxidants.
- Prioritize mental health through counseling, peer groups, or mindfulness practices.
- Watch for late effects like fatigue, bone loss, or secondary cancers and act early.
What is cancer survivorship?
Cancer survivorship refers to the phase after primary treatment when you shift from active therapy to living with the long‑term consequences of cancer and its treatment. It covers physical health, emotional wellbeing, and the practical steps needed to prevent recurrence. Understanding this broader picture helps you make informed choices instead of reacting to each symptom as it appears.
Build a Structured Follow‑up Care Plan
Never assume the oncologist disappears once chemo ends. A solid follow‑up plan keeps you ahead of potential issues.
- Schedule a post‑treatment visit with your oncology follow‑up team within three months of finishing therapy. This first meeting establishes baseline lab values and imaging.
- Ask for a surveillance imaging calendar. Depending on cancer type and stage, this might mean a CT scan every six months for the first two years, then annually.
- Introduce a primary care coordination physician into the loop. Your GP can manage routine blood work, vaccinations, and address comorbidities like hypertension.
- Document every appointment, test result, and medication change in a simple spreadsheet or survivorship app. Having a single source of truth makes conversations with specialists smoother.

Stay Active - Even When Fatigue Hits
Many survivors assume rest is the safest route, but gentle movement actually combats fatigue.
Start with physical activity that fits your current stamina. Walking 20 minutes a day, light gardening, or a beginner’s yoga video are excellent entry points. Gradually increase duration or intensity by about 10% each week.
If you feel drained, practice fatigue management techniques:
- Break activities into 10‑minute chunks with short rests in between.
- Stay hydrated; dehydration can mimic or worsen tiredness.
- Prioritize sleep hygiene - dark room, cool temperature, no screens an hour before bed.
Nutrition That Supports Recovery
What you eat directly influences healing, immune function, and weight stability.
Focus on a diet rich in:
- Lean proteins - fish, poultry, legumes - to rebuild tissue.
- Whole grains - oats, quinoa, brown rice - for steady energy.
- Colorful fruits and vegetables - berries, leafy greens, carrots - packed with antioxidants.
- Healthy fats - avocado, nuts, olive oil - to reduce inflammation.
Limit processed meats, excess sugar, and alcohol, as studies link them to higher recurrence risk. If weight loss or gain is a concern, work with a dietitian who understands survivorship nutrition.
Mental and Emotional Wellbeing
Surviving cancer can leave a lingering sense of anxiety, fear of recurrence, or even post‑traumatic stress.
Professional psychological support is a game‑changer. A therapist trained in oncology can teach coping skills, mindfulness, and cognitive restructuring.
Peer connection matters too. Join a local or online support group. Sharing stories reduces isolation and often uncovers practical tips you’d never hear elsewhere.
Consider journaling, gentle meditation, or creative hobbies as daily stress reducers.
Watch for Late Effects
Even years after treatment, some side effects may surface. Awareness allows early intervention.
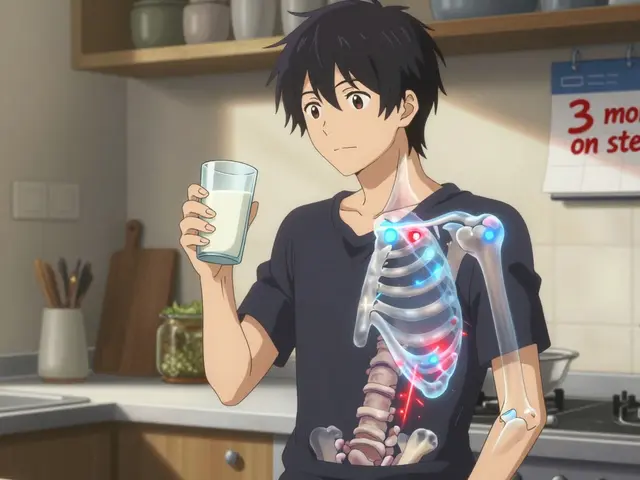
- Bone health: Certain chemotherapy agents and hormonal therapies can thin bones. Get a DEXA scan every 2‑3 years and discuss calcium, vitamin D, or bisphosphonate therapy.
- Cardiovascular risk: Radiation to the chest or drugs like anthracyclines raise heart disease risk. Annual blood pressure checks and lipid panels are essential.
- Secondary cancers: Regular surveillance imaging and skin exams help catch new malignancies early.
- Neuropathy: Persistent numbness or tingling may improve with physical therapy and vitamin B12 supplementation.
Keep a symptom diary; note when new issues start and share it with your oncology team.
Survivorship Checklist
| Component | What to Do | Frequency |
|---|---|---|
| Oncology follow‑up visit | Review labs, discuss symptoms, adjust survivorship plan | Every 3-6months (first 2years) |
| Surveillance imaging | CT, MRI, or PET scan as per cancer type | 6months → 1year intervals |
| Primary care check‑up | Blood pressure, cholesterol, vaccinations | Annually |
| Physical activity | Moderate aerobic + strength training | ≥150min/week |
| Nutrition review | Dietitian consult, food diary | Every 6months |
| Mental health screening | Questionnaire, counseling referral if needed | Every 6months |
| Bone health assessment | DEXA scan, calcium/vitaminD review | Every 2-3years |
| Support group participation | Attend meetings, share experiences | Monthly or as desired |
Frequently Asked Questions
How soon after treatment should I see my oncologist?
Most guidelines recommend a first post‑treatment visit within 4-6 weeks. This appointment sets the baseline for labs and imaging and lets you discuss any lingering side effects.
Can I exercise if I still feel weak?
Yes-start low and go slow. Light walking, seated resistance bands, or gentle yoga help rebuild strength without overtaxing your body. Listen to your body and increase gradually.
What foods are best for reducing recurrence risk?
A diet high in fibre, plant‑based protein, and antioxidants-think beans, whole grains, berries, leafy greens, and fatty fish-has been linked to lower recurrence in several studies. Limit processed red meat and sugary drinks.
Do I need a special mental‑health therapist?
A therapist with oncology experience understands the unique fears and identity shifts survivors face. If none are nearby, tele‑health options focused on cancer survivorship are widely available.
How can I spot late‑effect symptoms early?
Keep a simple log of new aches, changes in stamina, or unusual lumps. Bring this log to any appointment. Regular bone density scans, heart checks, and skin exams are also proactive measures.
Life after a carcinoma diagnosis is a new chapter, not a free pass. By staying organized, active, and connected, you give yourself the best shot at a long, thriving future.





Comments
First, it is imperative that survivors maintain a meticulously documented follow‑up schedule; without such rigor, even the most diligent patient may inadvertently miss critical imaging or lab work. Second, the oncology team should be consulted within three months post‑treatment, establishing baseline labs, imaging, and a survivorship care plan; this baseline serves as the reference point for all future assessments. Third, primary care physicians must be incorporated into the care loop, overseeing vaccinations, cardiovascular risk stratification, and management of comorbid conditions. Fourth, patients should employ a centralized log-be it a spreadsheet, a dedicated app, or a paper notebook-to record every appointment, test result, and medication alteration, thereby facilitating clear communication across specialties. Finally, adherence to guideline‑directed surveillance intervals, such as six‑monthly CT scans for the first two years followed by annual imaging, cannot be overstated; deviation from these protocols has been associated with delayed detection of recurrence.
I find that just jotting down the next appointment on my phone calendar and setting a reminder works surprisingly well for me; it takes the mental load off and lets me focus on the day‑to‑day.
Survivorship is not merely a personal journey; it is a testament to our nation's resilience and the superiority of our healthcare infrastructure. When we emerge from the crucible of cancer treatment, we carry the banner of our country’s scientific advancement. It is essential to recognize that the follow‑up schedule prescribed by oncologists reflects decades of research funded by our patriotic taxpayers. Adhering to these guidelines demonstrates loyalty not just to oneself but to the collective progress of the nation. The first three months after therapy are critical; neglecting this window undermines the very foundations of the system that cured us. Regular imaging, such as CT or MRI scans, should be performed at the intervals recommended, without seeking alternative “holistic” shortcuts that lack empirical support. Our laboratories, equipped with cutting‑edge technology, provide the most accurate blood work, and we must trust their results. Engaging with a primary care physician is not a sign of weakness but an affirmation that we value coordinated care, a hallmark of a strong society. Physical activity, even modest walking, is a civic duty because it reduces recurrence rates, thereby preserving the workforce. Nutrition, rich in whole foods and low in processed meats, aligns with national dietary guidelines that aim to curb chronic disease. Mental health support, whether through counseling or peer groups, fortifies the emotional fortitude that our nation needs from its citizens. Bone health assessments, such as DEXA scans, protect you from fractures that could impede productive participation in society. Cardiovascular monitoring after chest radiation is non‑negotiable; the heart is the engine of the nation’s vitality. Recognizing late effects early, from neuropathy to secondary malignancies, allows for swift intervention and maintains our collective health capital. Keeping a symptom diary is a disciplined practice that reflects the orderliness of our great nation. Finally, by sharing your survivorship experiences in community forums, you inspire fellow patriots to pursue vigilance, thereby reinforcing the cycle of national health excellence.
Keeping a log helps keep things straight.
It is my firm belief that the very entities dictating follow‑up schedules have ulterior motives, possibly aiming to keep survivors dependent on a perpetual cycle of appointments that feed a hidden agenda. The timing of imaging, seemingly calibrated to maximize revenue streams, raises unsettling questions about the true purpose of these guidelines. While the industry presents these protocols as evidence‑based, one cannot ignore the subtle pressures exerted to enroll patients in costly clinical trials without transparent consent. Moreover, the integration of digital survivorship apps may serve as a conduit for data harvesting, allowing unseen parties to monitor our health trajectories in ways we have yet to comprehend. Therefore, a prudent survivor should remain vigilant, questioning each recommendation and seeking second opinions whenever possible.
We have a moral obligation to treat our bodies with reverence after they have endured the onslaught of chemotherapy and radiation; it is not merely a personal preference but a duty to honor the gift of life. This means refusing the temptation to indulge in processed junk foods that sabotage our recovery, and instead embracing a plant‑forward diet that fuels healing. It also entails committing to regular physical activity, even on days when fatigue whispers otherwise, because our perseverance sets an example for those still battling. In addition, seeking out mental health resources reflects a deeper ethical stance: acknowledging that emotional well‑being is inseparable from physical health, and refusing to stigmatize the need for professional support.
I just keep things simple I log my appointments on a notepad and check them off when I go
Walking the path of survivorship often feels like navigating a labyrinth where each corridor represents a new challenge-yet each turn also offers an opportunity for self‑discovery. By reflecting on the interdependence between mind, body, and community, we can cultivate a holistic resilience that transcends mere symptom management. Engaging regularly with supportive peers and compassionate professionals acts as a lantern, illuminating the darker passages of doubt and fear. Ultimately, embracing this integrated approach not only mitigates recurrence risk but also enriches the very meaning of life beyond cancer.
Oh sure, because nothing says "I care about my health" like skipping your DEXA scan and hoping the bones just magicaly stay strong, right?
Obviously, that's the pinnacle of survivorship wisdom.
Follow the schedule, don't skip it.
i cant stress enough how important it is to keep a diary of symptoms it can literally save ur life if a problem shows up early
It is incumbent upon the discerning survivor to recognize that the ostensibly benevolent framework of post‑treatment surveillance may, in fact, be an instrument of systemic oversight, calibrated to monitor and, perhaps, subtly influence patient behavior. Such a perspective necessitates a vigilant appraisal of each recommended modality, ensuring that the adoption of imaging or laboratory assessments aligns unequivocally with one's personal health objectives rather than external imperatives. In this vein, the integration of independent second opinions serves not merely as a precaution but as an affirmation of intellectual autonomy. Moreover, the prudent allocation of one's temporal and financial resources toward interventions substantiated by rigorous peer‑reviewed evidence safeguards against the erosion of personal agency. Ultimately, an enlightened approach to survivorship intertwines empirical rigor with a steadfast commitment to self‑determination.
While many herald the standard follow‑up regimen as flawless, I maintain a skeptical eye toward its universal applicability.