When you’re pregnant or planning to breastfeed, taking any medication - even something as simple as an allergy pill or pain reliever - becomes a bigger decision. It’s not just about whether it works. It’s about whether it’s safe for you and your baby. Yet too many people leave their doctor’s office unsure, confused, or worse - scared into stopping a medication they actually need. This isn’t about fear. It’s about clarity. And it starts with how you talk to your provider.
Start Before You’re Pregnant
You don’t have to wait until you miss your period to talk about medications. If you’re trying to get pregnant, or even just thinking about it, this is the best time to review what you’re taking. Many common drugs - like certain acne treatments, seizure meds, or even some antidepressants - carry risks if taken early in pregnancy, often before a woman even knows she’s pregnant. The FDA stopped using the old A, B, C, D, X labels in 2015 because they were too vague. Now, drug labels include clear summaries of known risks, data from human studies, and what’s still unknown. Ask your provider: "Is this medication still right for me if I get pregnant?" Don’t assume it’s fine because you’ve taken it for years. Your body changes. Your needs change. Your risk profile changes.Use Trusted Resources - Not Google
Google searches about medication safety during pregnancy are dangerously unreliable. One study found that only 43% of top Google results matched expert guidelines. Meanwhile, MotherToBaby - a free, science-backed service run by experts - has 98% accuracy. They’ve been answering questions for over 35 years, with over 150,000 calls a year. Their database covers more than 1,800 medications and includes real-world data from thousands of pregnancies. If you’re worried about your antidepressant, your blood pressure pill, or your thyroid med, call them. Or visit their website. Print out the fact sheet. Bring it to your appointment. It gives you a common language to talk with your provider. No more guessing. No more "I heard on TikTok..."Ask for the Numbers - Not Just "It’s Safe"
When your provider says, "It’s safe," ask: "What does that mean?" A risk of "rare" doesn’t tell you anything. Ask for numbers. "Is it 1 in 100? 1 in 1,000?" For example, paracetamol (acetaminophen) is currently the only recommended pain reliever during all three trimesters, despite some recent studies raising questions. But the FDA reviewed 28 studies involving over 7 million pregnancies and still says the benefits outweigh the potential risks - as long as you use the lowest dose for the shortest time. That’s the kind of detail you need. If your provider can’t give you numbers, ask for a referral to a specialist. Many hospitals have teratology consultants - experts trained in how drugs affect fetal development. They’re not just for high-risk cases. They’re for anyone who wants clear answers.Don’t Stop Medication Without Talking
This is one of the biggest dangers. A 2021 study found that 40% of pregnant people stop taking necessary medications - like insulin for diabetes, antihypertensives, or psychiatric drugs - because they’re afraid. But untreated conditions can be far more dangerous than the meds. Uncontrolled diabetes increases the risk of birth defects. Untreated depression raises the chance of preterm birth and low birth weight. Stopping your seizure medication could lead to a seizure during pregnancy - which puts both you and your baby at risk. Your provider should help you weigh the risk of the drug versus the risk of the disease. Sometimes, the safest choice is to keep taking the medicine - just at the right dose.
Document Everything - And Make Sure It Follows You
If you’re taking multiple medications, especially for chronic conditions, your care team needs to know. This isn’t just about your OB/GYN. It’s about your pharmacist, your primary care doctor, and any specialist you see. Make sure your medication list is in your electronic health record - and that it’s updated every time something changes. Look for ICD-10 codes like Z33.1 (pregnant state incidental) or Z34.00 (supervision of normal pregnancy) being used in your chart. If they’re not, ask why. Also, make sure your pharmacist is aware. Pharmacists are trained in pregnancy and breastfeeding safety. They can flag interactions your doctor might miss. In top-performing clinics, pharmacists review every medication at three key moments: when pregnancy is confirmed, when a new drug is added, and when you start breastfeeding. That’s not a luxury - it’s standard care.Plan for Breastfeeding - Not Just Pregnancy
Many people think once the baby is born, the medication risk is over. It’s not. Drugs can pass into breast milk. Some are harmless. Others aren’t. LactMed, a free database from the National Library of Medicine, tells you exactly how much of a drug enters breast milk and whether it could affect your baby. For example, most SSRIs (like sertraline) are considered compatible with breastfeeding. But some migraine meds, like ergotamine, are not. Don’t wait until you’re nursing to ask. Talk about it during your third trimester. Ask: "Which of my meds are safe for breastfeeding?" and "Are there alternatives if one isn’t?" If your provider says, "You’ll be fine," ask for the evidence. If they can’t point to LactMed or MotherToBaby, it’s a red flag.Speak Up If You Feel Dismissed
Reddit threads and patient reviews tell a clear story: too many people feel ignored. One common complaint: "My doctor laughed when I asked about my anxiety meds." Another: "I was told ibuprofen was fine at 32 weeks - but I later found out it’s not recommended after 20 weeks." Emergency rooms are especially risky - 43% of pregnant patients report being given contraindicated drugs because no one asked about pregnancy status. If you feel rushed, dismissed, or talked down to, say so. You have the right to clear, respectful communication. Ask for more time. Ask for a second opinion. Ask for a medication review appointment. Some clinics now offer 15-20 minute dedicated slots just for this. If yours doesn’t, request it. Your safety matters more than the clock.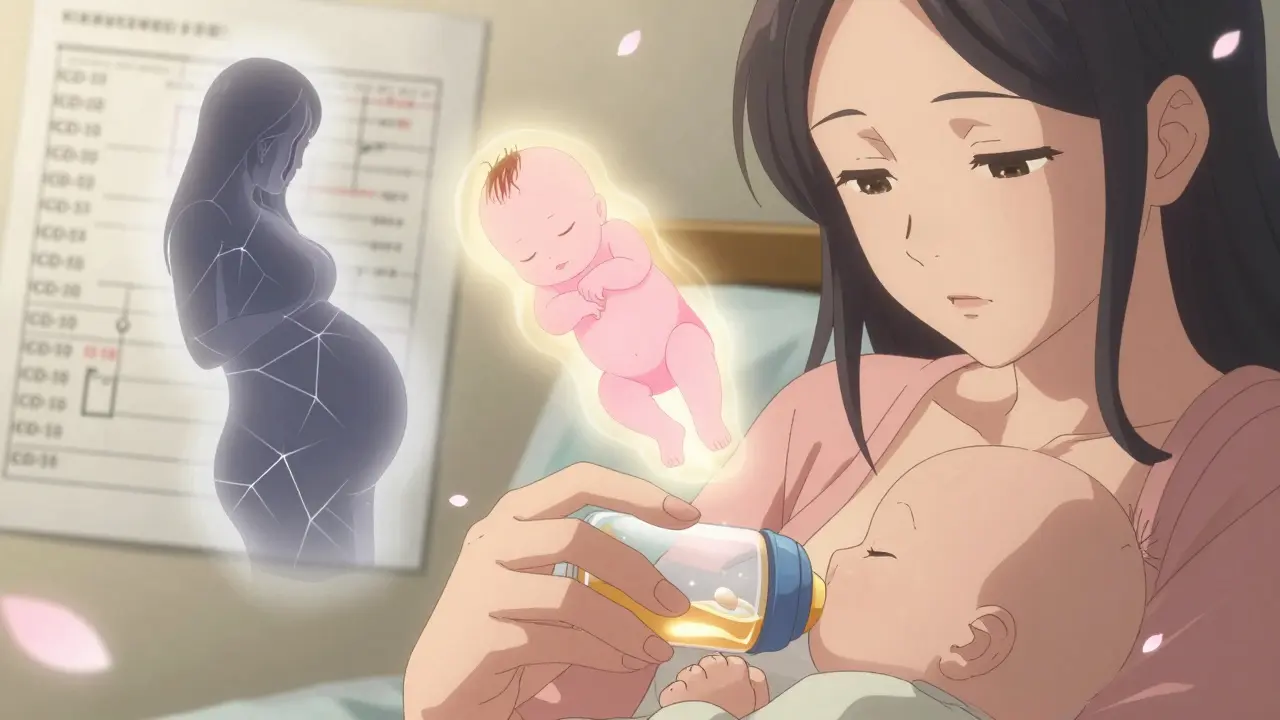
What to Bring to Your Appointment
Be prepared. Bring:- A complete list of all medications - including vitamins, supplements, and over-the-counter drugs
- Any recent lab results or specialist notes
- Printouts from MotherToBaby or LactMed about your meds
- A list of your questions - don’t rely on memory
- A notebook or phone to write down answers
What to Do If You’re in a Rural Area
Only 35% of rural clinics have access to teratology specialists. That’s a real gap. But you’re not out of options. Call MotherToBaby directly - they’re free and available 24/7. Use the LactMed app on your phone. Ask your pharmacist to help you check drug interactions. Many pharmacies now offer free consultations. If you’re on Medicaid or have limited access, know this: you still deserve the same level of care. Push for referrals. Ask your OB if they can connect you with a telehealth teratology service. Some hospitals now offer virtual consults - even if you’re 200 miles away.What’s Changing - And Why It Matters
Starting in 2025, all OB/GYN residency programs in the U.S. will be required to include medication safety training. That means future doctors will be better prepared. The FDA now requires new drugs to include clear fetal risk summaries. Insurance companies are starting to tie reimbursement to whether these conversations happen - CMS now requires documentation in 90% of prenatal visits. That’s pushing clinics to get better. But change moves slowly. You can’t wait for the system to catch up. You have to lead the conversation.Final Thought: You’re the Expert on Your Body
Your provider has the knowledge. But you have the lived experience. You know how you feel. You know what you’re willing to risk. You know your priorities. Don’t let anyone make you feel guilty for asking questions. The goal isn’t to avoid all risk - it’s to make informed choices. A healthy mom is the best thing for a healthy baby. That means managing your health - with the right tools, the right info, and the right conversation.Can I keep taking my antidepressants while pregnant or breastfeeding?
Many antidepressants, especially sertraline and citalopram, are considered compatible with pregnancy and breastfeeding based on decades of data. Stopping them suddenly can lead to relapse, which carries greater risks than the medication itself. Always discuss alternatives with your provider, but don’t stop without a plan. MotherToBaby and LactMed both have detailed, evidence-based profiles for each drug.
Is ibuprofen safe during pregnancy?
No - ibuprofen and other NSAIDs are not recommended after 20 weeks of pregnancy. They can affect fetal kidney development and reduce amniotic fluid. Paracetamol (acetaminophen) is the preferred pain reliever during pregnancy. If you’re already taking ibuprofen for a chronic condition, talk to your provider about switching before you conceive or as soon as you find out you’re pregnant.
What if I took a medication before I knew I was pregnant?
Don’t panic. Most medications don’t cause harm during the first few weeks - the embryo is either unaffected or doesn’t survive if there’s major damage. The key is to stop taking it as soon as you know you’re pregnant and consult a specialist. MotherToBaby can help assess your specific exposure. Many women have taken medications unknowingly and gone on to have healthy babies.
Are herbal supplements safe during pregnancy?
No - not without checking. Many herbal products aren’t tested for safety in pregnancy. Some, like black cohosh or dong quai, can trigger contractions. Others, like ginger, are generally considered safe in small amounts for nausea. Always tell your provider about every supplement. Just because it’s "natural" doesn’t mean it’s safe.
How do I know if my provider is qualified to discuss medication safety?
Ask if they use MotherToBaby, LactMed, or TERIS. Ask if they’ve completed CDC’s Medication Safety in Pregnancy training. If they rely on memory or vague statements like "it’s usually fine," they may not be up to date. You can also request a referral to a maternal-fetal medicine specialist or a clinical pharmacist who specializes in obstetrics. There’s no shame in asking for a second opinion - it’s your right.
Can telehealth help with medication safety questions?
Yes - and it’s growing fast. Since 2020, telehealth consultations for pregnancy medication safety have doubled. Services like MotherToBaby offer phone and video consults. Some EHR systems now integrate real-time risk assessments directly into virtual visits. If you live in a rural area or have limited access, telehealth can connect you with specialists who otherwise wouldn’t be available.







Comments
Had to call MotherToBaby last year when I was on an SSRI and found out I was pregnant. They walked me through the data point by point-no fluff, just facts. Turned out sertraline was fine at my dose, and I kept it through delivery and breastfeeding. Seriously, if you’re even a little unsure, just call them. Free, no judgment, and way better than scrolling through Reddit threads.
google says ibuprofen is fine till 30wks but the article says 20wks. who to belive? also why is paracetamol still ‘recommended’ when studies show it might mess with fetal hormones? someone please explain without using big words.
Wow, this is exactly why America’s healthcare system is crumbling. People are being told to ‘call a hotline’ instead of getting real care. If you’re pregnant and on meds, you need a doctor-not some website that’s funded by Big Pharma. I’ve seen too many women get scared into stopping meds they need because of fearmongering blogs. Real medicine isn’t a podcast.
You got this. Seriously. I know it feels overwhelming-like you’re being asked to become a pharmacologist overnight. But you’re not alone. Every question you ask is valid. Every time you print out a fact sheet from MotherToBaby? That’s power. You’re not being ‘difficult.’ You’re being responsible. And if your provider rolls their eyes? Find someone who lights up when you show up prepared. You’re not just protecting your baby-you’re setting a standard for how care should be done.
And yes, you can still have coffee. And yes, you can still take your anxiety meds. Just don’t do it alone. 💪❤️
I am from India. My doctor said no medicine in pregnancy. But I had high blood pressure. I was scared. Then I found LactMed. I showed to doctor. He changed my medicine. Now baby is 6 months old, I am on safe medicine, and I am breastfeeding. Thank you for this post. It helps many like me.
As someone who’s navigated both pregnancy and postpartum while managing a chronic autoimmune condition, I can’t stress enough how vital it is to treat this like a collaborative project-not a compliance checklist. Your OB isn’t your boss. Your pharmacist? Your ally. MotherToBaby? Your secret weapon. And LactMed? Your bedtime story for when anxiety creeps in at 3 a.m. Bring the printouts. Ask for the numbers. Say ‘I need more time’ even if your appointment is in 7 minutes. You’re not asking for special treatment-you’re asking for the baseline care every human deserves. And if they make you feel small for it? That’s not your failure. That’s their outdated system.
Stop taking antidepressants during pregnancy. It’s just common sense. You don’t need chemicals when you’ve got faith, yoga, and a positive mindset.
I took paracetamol every day when I was pregnant. Baby is 2 now and very smart. My friend took nothing and had a baby with problems. So maybe medicine is not bad. Talk to doctor, not internet.
So proud of how far we’ve come! I remember my mom being told to stop all meds and just ‘pray it through.’ Now we have real science, free resources, and people speaking up. You’re not alone. Keep asking. Keep showing up. The system is slow, but you’re moving it forward-one informed question at a time. You’re doing amazing.
Oh good, another ‘trust the experts’ manifesto. Let me guess-MotherToBaby is funded by the same conglomerate that makes your antidepressants? And LactMed? Probably written by a guy who thinks ‘natural’ means ‘unpatentable.’ Meanwhile, real women are being guilt-tripped into staying on SSRIs because ‘the risk of relapse is higher.’ Funny how the risk of fetal neurodevelopmental disruption never gets the same airtime. I’ll take my chances with a little anxiety over a kid who can’t process emotions because mom was on Zoloft for 9 months.
It’s funny how the same people who scream ‘trust science’ when it’s about vaccines suddenly turn into conspiracy theorists when it’s about pregnancy meds. You don’t need to be a toxic analyst to see that dismissing decades of human data because you read one ‘concerning’ mouse study is… well, it’s not science. It’s fear with a thesaurus. MotherToBaby’s database is built on 150k+ actual pregnancies-not TikTok anecdotes or pharmaceutical brochures. If you’re gonna question it, bring peer-reviewed studies. Otherwise, maybe just… breathe?
It’s 2025. The FDA updated labeling. Residency programs are mandated. CMS is auditing documentation. And yet we’re still having this conversation? The infrastructure is there. The evidence is robust. The tools are free. The only thing missing is the cultural will to treat pregnant people as autonomous agents rather than incubators with liability concerns. If your provider still says ‘it’s usually fine,’ they’re not just outdated-they’re negligent. And frankly, if you’re still Googling, you’re doing the system’s job for it.