Why the Link Between COPD and Allergies Matters
Most people think of chronic obstructive pulmonary disease (COPD is a progressive lung disease characterized by airflow limitation, chronic inflammation, and irreversible damage) as a smoker’s disease, while allergies are seen as harmless seasonal annoyances. Recent research, however, shows that the two often cross paths, worsening symptoms and complicating treatment. If you live with COPD, ignoring an allergic component may mean more flare‑ups, faster decline in lung function, and a lower quality of life.
Understanding COPD: Core Features
COPD develops over years of exposure to irritants-most commonly cigarette smoke, but also indoor pollutants, occupational dust, and biomass fuels. The disease is defined by three hallmarks:
- Persistent airway narrowing measured by spirometry is a pulmonary function test that quantifies airflow obstruction (FEV1/FVC < 0.70).
- Chronic inflammation that involves neutrophils, macrophages, and, in many patients, eosinophils.
- Irreversible structural changes such as emphysema and airway remodeling.
According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2024 report, about 3.2 million adults in the United States have moderate‑to‑severe COPD, and the disease accounts for roughly 6% of all deaths worldwide.
What Counts as an Allergy?
Allergies are immune‑mediated hypersensitivity reactions to otherwise harmless substances, called allergens, that trigger the release of ImmunoglobulinE (IgE). Common allergens include pollen, pet dander, dust mites, and certain foods. When IgE binds to mast cells, it releases histamine and other mediators, leading to symptoms ranging from sneezing to airway constriction.
While many consider allergies a simple nuisance, around 30% of adults have clinically significant allergic rhinitis, and up to 10% develop allergic asthma, a condition where airway inflammation is driven largely by eosinophils and IgE‑related pathways.
Where COPD and Allergies Overlap
The overlap isn’t a coincidence; several biological pathways converge:
- Eosinophilic inflammation. About 20‑30% of COPD patients show elevated blood eosinophil counts (>300cells/µL). This phenotype responds better to inhaled corticosteroids, the same drugs that control allergic asthma.
- IgE‑mediated pathways. Studies published in the European Respiratory Journal (2023) found that higher serum IgE levels correlate with increased COPD exacerbation rates, suggesting a shared allergic component.
- Airway hyper‑responsiveness. Allergic sensitization can make COPD airways more reactive to irritants, leading to frequent bronchospasm.
In practical terms, a patient with COPD who also has allergic rhinitis may experience worse daytime dyspnea, night‑time coughing, and more frequent hospitalizations.
Clinical Evidence: Numbers That Speak
Several large‑scale studies illustrate the link:
- A 2022 cohort of 4,500 COPD patients in Europe found that 38% reported diagnosed allergic rhinitis. Those with both conditions had a 1.8‑fold higher risk of severe exacerbations.
- The COPDGene study (2021) showed that subjects with high IgE levels (>200IU/mL) had on average a 12% lower FEV1% predicted compared to low‑IgE counterparts.
- In the US, the National Health Interview Survey (2023) reported that 22% of adults with COPD also reported seasonal allergy symptoms, and this subgroup used rescue inhalers 35% more often.
These data reinforce that ignoring the allergic component is a missed opportunity for better disease control.
Diagnosing the Overlap: Tools and Tips
Clinicians need a systematic approach:
- Spirometry. Confirms airflow limitation and helps differentiate COPD from pure asthma.
- Allergy testing. Skin prick or serum-specific IgE testing pinpoints relevant allergens.
- Blood eosinophil count. A simple CBC can flag the eosinophilic COPD phenotype (≥300cells/µL).
- Symptom diary. Tracking triggers-pollen spikes, pet exposure, smoke-can reveal patterns that point to an allergic contribution.
When both spirometry results and allergy tests point to overlapping disease, the diagnosis is often labeled “COPD‑asthma overlap syndrome (CAOS)”.

Managing Both Conditions: Integrated Strategies
Effective treatment hinges on addressing the shared inflammatory pathways while also tackling unique aspects of each disease.
- Inhaled corticosteroids (ICS) are a class of anti‑inflammatory inhalers that reduce eosinophilic activity and suppress IgE‑driven inflammation. For COPD patients with ≥300 eosinophils/µL, adding an ICS to a long‑acting bronchodilator can cut exacerbations by up to 25%.
- Long‑acting bronchodilators. LABA (long‑acting β2‑agonist) and LAMA (long‑acting muscarinic antagonist) remain the backbone of COPD therapy, improving airflow regardless of allergic status.
- Allergen avoidance. Simple measures-HEPA filters, frequent bedding washes, pet‑free bedrooms-lower exposure and reduce symptom burden.
- Allergy immunotherapy. Subcutaneous or sublingual immunotherapy has shown promise in reducing COPD exacerbations in patients with documented allergic triggers (2024 meta‑analysis).
- Vaccinations. Influenza and pneumococcal vaccines prevent infections that can amplify both allergic inflammation and COPD flare‑ups.
Creating a personalized action plan that includes rescue inhaler use, a clear trigger‑avoidance checklist, and scheduled follow‑ups can dramatically improve outcomes.
Lifestyle Moves That Benefit Both
Addressing modifiable risk factors offers the biggest win:
- Smoking cessation. Quitting smoking reduces airway inflammation, lowers IgE levels, and improves response to inhaled steroids.
- Air quality. Using portable air purifiers, avoiding heavy‑traffic routes, and monitoring AQI can lessen irritant exposure.
- Exercise. Pulmonary rehabilitation improves lung mechanics and can also reduce systemic inflammation that fuels allergic reactions.
- Nutrition. Diets rich in omega‑3 fatty acids and antioxidants have been linked to lower eosinophil counts and better lung function.
Future Directions: What Researchers Are Exploring
Scientists are digging deeper into the COPD‑allergy nexus:
- Biologic therapies. Monoclonal antibodies targeting IL‑5 (e.g., mepolizumab) are approved for severe eosinophilic asthma and are being trialed in COPD patients with high eosinophils.
- Precision medicine biomarkers. Multi‑omics panels that combine IgE, periostin, and exhaled nitric oxide aim to predict which COPD patients will benefit most from anti‑allergic treatment.
- Microbiome modulation. Early data suggest that altering the airway microbiome may dampen both bacterial‑driven COPD inflammation and allergen‑induced hyper‑responsiveness.
These advances promise a future where therapy is tailored not only to airflow limitation but also to the patient’s allergy profile.
Quick Reference Checklist
- Ask your doctor about allergy testing if you have frequent COPD flare‑ups.
- Know your blood eosinophil count; ≥300cells/µL signals potential benefit from inhaled steroids.
- Keep a symptom‑trigger diary for at least four weeks.
- Implement at least two allergen‑avoidance steps (e.g., air purifier, bedding washing).
- Stay up‑to‑date on vaccinations and consider pulmonary rehab.
Related Concepts and Next Steps
Understanding the COPD‑allergy link opens the door to broader topics in respiratory health. Within our knowledge cluster, you can explore:
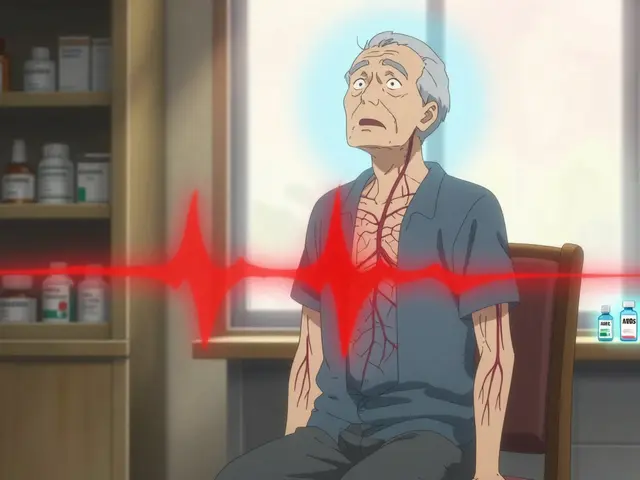
- Heart Health: The impact of chronic hypoxia on cardiovascular risk.
- Senior Health: Managing multimorbidity when COPD, allergies, and arthritis coexist.
- Medication Management: Safe use of bronchodilators alongside antihistamines.
- Guides and Tips: Practical home‑environment modifications for better air quality.
Each of these areas builds on the foundation you’ve just read, helping you create a comprehensive wellness plan.
| Attribute | COPD | Asthma | Allergic Rhinitis |
|---|---|---|---|
| Typical onset age | 40‑65years | Childhood‑adolescence | Any age, peaks 20‑40years |
| Main trigger | Smoking, pollutants | Allergens, exercise | Pollen, dust mites |
| Reversibility (FEV1) | Partial, <12% | Often >12% | Not applicable |
| Inflammatory cells | Neutrophils, eosinophils | Eosinophils, mast cells | Mast cells, IgE |
| Treatment focus | Bronchodilators, steroids (if eosinophilic) | ICS, bronchodilators, biologics | Antihistamines, nasal steroids, avoidance |
Frequently Asked Questions
Can allergies make COPD symptoms worse?
Yes. Allergens can trigger airway inflammation, increase mucus production, and heighten bronchial hyper‑responsiveness, all of which amplify COPD breathlessness and cough.
Is it worth getting an allergy test if I already have COPD?
Absolutely. Identifying specific allergens lets you apply targeted avoidance strategies and, in some cases, immunotherapy-both of which can reduce exacerbation frequency.
Do inhaled corticosteroids treat allergies as well as COPD?
Inhaled steroids suppress eosinophilic inflammation common to both conditions, so they can alleviate allergic airway symptoms while also slowing COPD progression in eosinophilic patients.
What lifestyle changes help both COPD and allergies?
Quit smoking, improve indoor air quality with HEPA filters, keep humidity below 50%, use dust‑mite‑proof bedding, stay active with pulmonary rehab, and follow a diet rich in omega‑3s and antioxidants.
Can biologic drugs for asthma help COPD patients?
Biologics that target IL‑5 or IgE have shown promise in COPD patients with high eosinophil counts or strong allergic sensitization, but they’re still under clinical investigation.
How often should I see my doctor for monitoring?
At least twice a year for stable disease, and sooner if you notice new allergy symptoms, increased cough, or more frequent rescue inhaler use.






Comments
Looks like another boring article about COPD and allergies just rehashing old facts
While the article provides a comprehensive overview, it fails to emphasize that eosinophilic COPD represents a distinct therapeutic target requiring precise biomarker-driven interventions. The authors should have cited the latest GOLD 2024 guidelines explicitly, especially the recommendation for inhaled corticosteroids only in patients with blood eosinophils ≥300 cells/µL. Moreover, the discussion of biologics is superficial; recent Phase III trials of mepolizumab in high‑eosinophil COPD cohorts have demonstrated a statistically significant reduction in exacerbation rates. A more rigorous analysis of cost‑effectiveness would also benefit clinicians facing budget constraints. In short, the piece oversimplifies complex management algorithms and thus does a disservice to the informed reader.
From a global health perspective, the interplay between COPD and allergic sensitization cannot be ignored. In low‑ and middle‑income regions, indoor biomass fuel exposure compounds allergic inflammation, leading to a synergistic decline in lung function. The article rightly highlights eosinophils, yet it should also address how cultural practices such as indoor cooking without ventilation exacerbate both conditions. Policy makers must therefore consider culturally tailored interventions, including community education on proper stove use and allergen mitigation. Ignoring these sociocultural dimensions would render any clinical recommendation ineffective.
I understand how overwhelming these overlapping conditions can feel, and it’s encouraging to see such detailed guidance. Taking small steps like improving indoor air quality or keeping a simple symptom diary can make a big difference. Remember, you’re not alone in navigating this journey, and your healthcare team is there to help personalize the plan.
When we stare into the mirror of our own breath, we see reflections of countless tiny battles fought between allergens and damaged airways.
The simple act of washing bedding weekly becomes, in that quiet moment, a ritual of resistance against invisible dust mites.
Similarly, the decision to place a HEPA filter beside the bed is not merely a purchase but a symbolic gesture of reclaiming control.
Each inhaled breath, filtered and purified, whispers a promise that the body can recover, even if the odds seem stacked.
It is strange how a piece of technology can feel like a talisman, protecting the lungs that have endured years of smoke and pollen.
Yet we must also remember that true healing lies in the balance between external aids and internal acceptance.
Accepting that we may never be completely free of triggers does not mean surrender, but rather invites us to adapt gracefully.
In that adaptation, the mind learns to detach from the panic that a sudden cough might trigger.
The heart, meanwhile, steadies as we incorporate gentle exercises, letting the muscles learn new patterns of oxygen use.
Nutrition, too, plays its quiet role; omega‑3s glide through the bloodstream like tiny diplomats negotiating peace between inflammation and repair.
And as we breathe, the microbiome of our airways, a bustling micro‑city, may shift toward a calmer, less hostile community.
Science is still uncovering how these tiny organisms converse with our immune system, but the hope is that they will one day become allies.
Until then, hybrid strategies-medication, avoidance, and lifestyle-form a mosaic that is uniquely ours.
Do not underestimate the power of consistency; a daily habit of opening windows when pollen counts drop can shave minutes off a wheeze.
In the end, living with COPD and allergies is a marathon, not a sprint, and every modest improvement is a victory worth celebrating 😊.
For patients unsure about whether to pursue allergy testing, a practical approach is to start with a detailed exposure diary for two to three weeks, then discuss the patterns with the pulmonologist. If the diary shows consistent symptom spikes correlated with specific triggers, targeted skin‑prick testing or serum IgE panels are justified. This stepwise strategy avoids unnecessary tests while ensuring that relevant allergens are identified.