Understanding the Connection between Diabetes and Fever
As a diabetic patient, it's essential to understand how fever can impact your glucose levels and overall health. In this section, we'll dive into the connection between diabetes and fever, exploring how infections can cause high blood sugar levels and the potential complications that can arise from this combination. Knowing this information can help you stay prepared and take necessary precautions to maintain good health.
Common Infections that Cause Fever in Diabetic Patients
Diabetic patients are more susceptible to infections due to their weakened immune system, which might lead to fever. Let's take a look at some common infections that can cause fever in diabetic patients:
1. Urinary tract infections (UTIs)
2. Skin infections, such as cellulitis, fungal infections, or diabetic foot infections
3. Respiratory infections, including the common cold, flu, or pneumonia
4. Gastrointestinal infections, like food poisoning or gastroenteritis
5. Dental infections or gum disease
It's crucial to be aware of these common infections as they might require prompt medical attention to prevent complications and ensure proper diabetes management.
How to Manage Blood Sugar Levels During Fever
When you have a fever, your body is working overtime to fight off infection, which can cause your blood sugar levels to rise. Here are some tips on managing your blood sugar levels during fever:
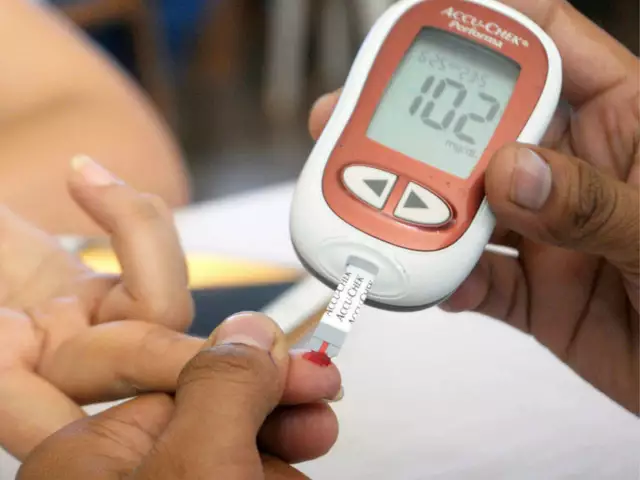
1. Monitor your blood sugar levels more frequently than usual, ideally every 2 to 4 hours.
2. Stay well-hydrated by drinking water, sugar-free beverages, or clear broths to help flush out toxins and maintain your blood sugar levels.
3. Continue taking your diabetes medications as prescribed, unless your healthcare provider advises otherwise.
4. Adjust your insulin dosage as needed based on your blood sugar levels and consult your healthcare provider if you're unsure of how to do this.
5. Keep a supply of sugar-free electrolyte drinks or glucose gel on hand to help treat low blood sugar if it occurs.
Remember, managing your blood sugar levels during fever is crucial to avoid complications and ensure a swift recovery.
When to Seek Medical Attention
It's essential to know when to seek medical attention if you're a diabetic patient with a fever. Here are some warning signs that you should not ignore:
1. Persistent high blood sugar levels despite taking your medications and adjusting your insulin dosage
2. Severe dehydration symptoms, such as dark urine, extreme thirst, dizziness, or confusion
3. Fever lasting more than a few days or not improving with over-the-counter medications
4. Signs of complications, such as breathing difficulties, chest pain, or severe abdominal pain
5. Any new or worsening symptoms that concern you or make you feel unwell
Don't hesitate to reach out to your healthcare provider if you're experiencing any of these symptoms, as they might indicate a more severe infection or complication that requires immediate medical attention.
Preventing Infections and Fever in Diabetic Patients
Prevention is always better than cure, especially for diabetic patients who are more prone to infections and fever. Here are some tips to help prevent infections and maintain good health:
1. Practice good personal hygiene by washing your hands regularly, especially before handling food or after using the bathroom.
2. Get vaccinated for preventable diseases, such as the flu, pneumonia, and COVID-19, as recommended by your healthcare provider.
3. Take care of your skin and feet by keeping them clean, dry, and moisturized to prevent cuts, cracks, and infections.
4. Keep your blood sugar levels well-controlled through proper diet, exercise, and medication management.
5. Maintain regular dental check-ups and practice good oral hygiene to prevent gum disease and dental infections.
By following these preventive measures, you can reduce your risk of infections and fever, ensuring a healthier and more comfortable life as a diabetic patient.






Comments
Honestly, the whole “common infections” list feels like a lazy rehash of textbook bullet points; anyone who’s been managing diabetes knows the real issue isn’t the pathogens but the inevitable neglect of proper glycemic control that invites them in.
Picture this: a blazing fever ignites a wildfire inside your bloodstream, and every rogue microbe becomes a mischievous spark threatening the fragile equilibrium of your sugar levels. The drama of a diabetic body waging war against an invisible army is nothing short of a cinematic showdown, complete with the sweaty anguish of dehydration and the relentless surge of glucose that feels like a rogue tide crashing against a fragile dam.
From a philosophical standpoint, fever in the diabetic condition can be viewed as an embodiment of the tension between homeostatic order and pathological chaos. The immune response, in its fervent quest to eradicate invading agents, inadvertently perturbs the delicate balance of glucose metabolism, thereby illustrating the paradoxical nature of physiological self‑regulation. It is incumbent upon the patient to cultivate a mindful awareness of this interplay, lest the transient elevation of temperature cascade into a prolonged dysregulation of metabolic homeostasis.
I hear your frustration and it’s true that diet plays a huge role but battling a fever isn’t just about food it’s also about staying hydrated and checking sugars more often because your body is working overtime
Let us be precise: during febrile episodes the endogenous catecholamine surge precipitates hepatic gluconeogenesis and glycogenolysis, which can elevate plasma glucose concentrations to hyperglycemic thresholds. Moreover, the inflammatory cytokine cascade (IL‑6, TNF‑α) exacerbates insulin resistance at the peripheral level. It is essential that clinicians employ evidence‑based algorithms-such as the ADA’s fever‑adjusted insulin correction factor-to mitigate iatrogenic complications. As a proponent of rigorous standards, I must stress that any deviation from protocol jeopardizes both individual health outcomes and, by extension, our national public‑health preparedness.
One must not be lulled into complacency by the veneer of “evidence‑based” guidelines; the moral imperative is to recognize that each patient’s circumstance may defy generic algorithms, demanding a personalized approach that transcends bureaucratic dogma.
First and foremost, let us address the glaring omission in the original treatise: the absolute necessity of a rapid response team for diabetic patients who develop a fever. In my experience, the delay between symptom onset and medical intervention is often indefinately prolonged, resulting in a cascade of preventable complications. It is not enough to merely advise hydration; one must also ensure that electrolyte imbalances are corrected with timely intravenous therapy. Furthermore, the recommendation to monitor blood sugar “every 2 to 4 hours” is far too vaguer than the reality demands; a rigorous schedule of hourly checks is mandatory during the acute phase. The article also fails to acknowledge the particular vulnerability of elderly diabetics, who are predisposed to atypical presentations and therefore require heightened vigilance. It is absolutely critical to educate patients on the signs of ketoacidosis, which can masquerade as a simple fever and be easily missed. Moreover, the assertion that “continue taking your medications as prescribed” overlooks the fact that certain oral hypoglycemics may need to be suspended in the presence of infection to avoid hypoglycemic episodes. The role of family members cannot be understated – they must be trained to recognize subtle shifts in mental status that could herald a serious metabolic derangement. I cannot stress enough that the healthcare system must allocate resources for home‑based monitoring kits, lest we continue to see unnecessary hospitalizations. Additionally, the piece neglects to mention the impact of seasonal influenza vaccinations, which have repeatedly demonstrated efficacy in reducing febrile incidents among diabetics. The underlying theme here is one of complacency, and complacency is a luxury we cannot afford. In summation, a comprehensive, proactive, and aggressively preventative strategy is the only defensible approach to managing fever in diabetic patients. The current guidelines are merely a starting point; they must be expanded, refined, and enforced with uncompromising rigor. Failure to do so will inevitably result in avoidable morbidity and, ultimately, loss of life. Therefore, let us champion a paradigm shift that places immediate, decisive action at the forefront of diabetic fever management.
Oh great, another “must‑do‑everything” checklist-because apparently we’ve all got spare hours to run hourly glucose checks while battling a fever, right?
Good points overall