Stomach Pain & Blood Sugar Checker
Diabetes Mellitus is a chronic metabolic disorder marked by elevated blood glucose due to insufficient insulin production or impaired insulin action. It affects more than 460million adults worldwide and is a leading cause of cardiovascular, renal, and nerve complications.
Abdominal Pain is a symptom that can arise from any organ in the belly cavity, ranging from mild cramping to severe, burning discomfort. When it appears repeatedly in people with or at risk of diabetes, it often points to specific metabolic disturbances.
Why the Stomach Talks When Blood Sugar is Off‑Balance
Two main pathways connect blood glucose swings to gut discomfort: Gastroparesis, a condition where the stomach empties slower than normal, and Diabetic Autonomic Neuropathy, which impairs the nerves that control intestinal motility. Both are directly linked to chronic hyperglycemia, but they also flare up during sudden spikes or drops.
When glucose climbs above 180mg/dL after a meal, the stomach’s smooth muscle receives mixed signals: high insulin levels should speed up digestion, yet excess sugar triggers inflammation of the gastric wall. This leads to bloating, nausea, and that classic “food‑got‑stuck” feeling.
Conversely, hypoglycemia (below 70mg/dL) triggers the release of adrenaline, which can cause gut spasm and cramp‑like pain. Many patients describe a “knot” in the upper abdomen just before a low‑blood‑sugar episode.
Key Players in the Pain‑Glucose Loop
- Hyperglycemia - persistent blood sugar >125mg/dL fasting; accelerates glycation of proteins in the stomach lining.
- Hypoglycemia - sudden drop in glucose; stimulates catecholamines that contract gut muscles.
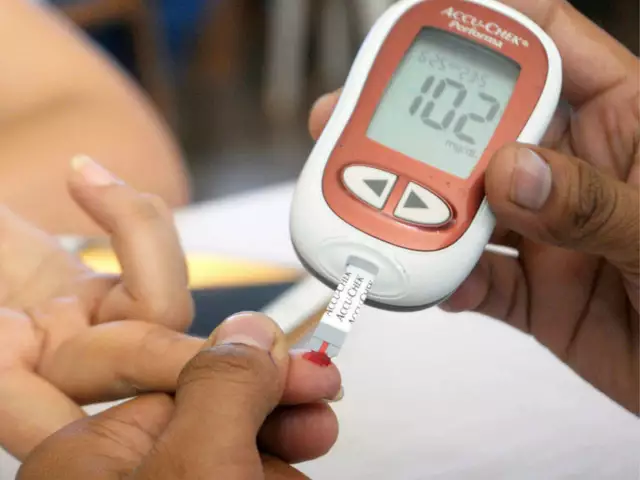
- Blood Glucose Monitoring - the routine of checking capillary glucose levels; provides the data needed to spot patterns that precede pain.
- Carbohydrate‑Rich Meals - meals high in simple sugars that can cause rapid post‑prandial spikes.
- Metformin - first‑line oral diabetes medication; can cause gastrointestinal upset in up to 25% of users.
- Inflammation (Enteritis) - chronic low‑grade inflammation of the gut lining, often driven by advanced glycation end‑products.
Spotting the Signs: When to Suspect Diabetes Behind Stomach‑Aches
Because abdominal pain is a common complaint, clinicians rely on a few red‑flag patterns:
- Persistent nausea or early satiety lasting more than three months.
- Pain that improves when blood sugar is brought into target range.
- Concurrent symptoms like increased thirst, frequent urination, or unexplained weight loss.
- History of “reactive hypoglycemia” after carbohydrate‑heavy meals.
If two or more of these appear, a fasting glucose test or HbA1c measurement is warranted. Early detection can prevent long‑term nerve damage that aggravates gut motility.
Managing Stomach Pain When You Have Diabetes
Effective control hinges on three pillars: glucose stability, gut‑friendly nutrition, and targeted medication adjustments.
1. Stabilize Blood Sugar
Use continuous glucose monitors (CGM) or regular finger‑stick checks to keep fasting glucose between 80‑130mg/dL and post‑meal peaks under 180mg/dL. Small, frequent meals (5-6 per day) reduce the magnitude of spikes.
2. Choose Diabetes‑Safe Foods
- Low‑glycemic carbohydrates (steel‑cut oats, quinoa, legumes).
- High‑fiber vegetables that slow gastric emptying without causing constipation.
- Lean protein sources such as poultry, fish, or tofu.
- Avoid excess fatty foods, which can exacerbate gastroparesis.
3. Medication Review
If metformin triggers nausea, doctors may split the dose, switch to an extended‑release form, or add a gastrointestinal‑protective agent. For confirmed gastroparesis, pro‑kinetic drugs like metoclopramide are used, but they require careful monitoring for side effects.
4. Lifestyle Hacks
Gentle walking after meals, staying upright for at least an hour, and practicing stress‑reduction techniques (deep breathing, meditation) can improve autonomic nerve tone and ease cramping.

Comparing the Two Main Diabetes‑Related Digestive Disorders
| Attribute | Gastroparesis | Diabetic Autonomic Neuropathy |
|---|---|---|
| Primary Cause | Delayed gastric emptying due to nerve damage | Broad nerve impairment affecting gut motility |
| Typical Symptoms | Early satiety, bloating, vomiting of undigested food | Abdominal cramping, irregular bowel movements |
| Diagnostic Test | Gastric emptying scintigraphy | Heart rate variability, autonomic reflex testing |
| Treatment Options | Pro‑kinetic agents, dietary modification | Blood‑sugar control, neuromodulators |
| Prevalence in Diabetes | ≈5% of type1, 10% of type2 | ≈30% of long‑standing diabetes |
When to Seek Professional Help
If stomach pain is accompanied by vomiting blood, sudden weight loss, or persistent diarrhea, emergency care is needed. For ongoing discomfort, schedule an appointment with an endocrinologist or a gastroenterologist who understands the metabolic‑digestive interface.
During the visit, bring a log of your glucose readings, medication doses, and meal patterns. This data lets the clinician pinpoint whether the pain aligns with glucose excursions or a separate digestive disorder.
Looking Ahead: Research Trends Linking Gut Health and Diabetes
Emerging studies show the gut microbiome plays a role in insulin sensitivity. Probiotic trials suggest certain bacterial strains can reduce post‑prandial spikes, indirectly easing gastric discomfort. Meanwhile, newer CGM algorithms flag “gastroparesis‑risk” patterns by analyzing the rate of glucose rise after meals.
Staying informed about these advances can empower patients to adopt early interventions-think personalized nutrition plans based on stool‑sample analysis or wearable devices that monitor gastric motility alongside glucose.
Take‑Away Checklist
- Track blood glucose before and after meals to spot pain‑glucose links.
- Prefer low‑glycemic, high‑fiber meals and avoid large fatty portions.
- Review diabetes meds if they cause nausea; discuss alternatives with your doctor.
- Consider pro‑kinetic therapy if gastroparesis is confirmed.
- Stay active after eating and keep upright for 60‑90 minutes.
By treating the stomach as a window into metabolic health, you can catch diabetes‑related issues sooner and keep both your gut and blood sugar in balance.
Frequently Asked Questions
Can occasional stomach aches be a sign of diabetes?
Occasional cramps are usually harmless, but if the pain repeats after meals and you also notice increased thirst, frequent urination, or weight loss, it’s worth checking your blood sugar. Early testing can rule out or confirm diabetes before complications develop.
What is the main difference between gastroparesis and diabetic neuropathy‑related abdominal pain?
Gastroparesis specifically slows stomach emptying, leading to early satiety and vomiting of undigested food. Diabetic autonomic neuropathy affects the entire gut, causing irregular bowel movements and cramping without necessarily slowing gastric emptying.
How quickly can blood‑sugar spikes cause stomach pain?
Symptoms can appear within 30‑60minutes after a high‑glycemic meal. The rapid rise triggers hormonal signals that irritate the stomach lining, producing a bloated, uncomfortable feeling.
Is metformin the only diabetes drug that hurts the stomach?
Metformin is the most common culprit, but sulfonylureas, GLP‑1 agonists, and SGLT2 inhibitors can also cause gastrointestinal side effects. Switching formulation or dosage timing often helps.
Can a low‑glycemic diet cure stomach pain for diabetics?
A low‑glycemic diet won’t cure underlying nerve damage, but it stabilizes glucose swings, which dramatically reduces pain episodes for most patients.






Comments
My stomach feels like a broken alarm that never stops
Honestly, the interplay between hyperglycemia and gastroparesis is nothing short of a textbook case of metabolic dysregulation. While most laypeople dismiss occasional bloating, the literature clearly delineates a cascade of advanced glycation end‑products that irritate the gastric mucosa. I’ve read countless studies that prove a direct correlation, yet the mainstream advice remains shockingly simplistic. The author’s checklist is useful, but it barely scratches the surface of neuro‑hormonal feedback loops. Just saying, if you want real insight, dive into the primary research, not this surface‑level guide.
From a pathophysiological perspective, the article glosses over the intrinsic myenteric plexus degeneration, thereby undermining a comprehensive mechanistic framework. The omission of vagal tone quantification and autonomic neuropathy indices is a glaring methodological oversight. Moreover, the glycemic thresholds presented lack calibration against continuous glucose monitoring variance coefficients. In short, the piece demonstrates a tokenistic approach to diabetic gastroenterology.
Stay on top of those glucose checks and keep moving after meals you got this
Listen, if you’re experiencing that knot feeling after a high‑carb meal, first thing is to log your numbers and food choices meticulously. Small, frequent meals combined with low‑glycemic carbs can dramatically reduce those spikes. Don’t hesitate to talk to your provider about adjusting metformin or adding a pro‑kinetic if symptoms persist. Consistency is key – make the tracking habit and you’ll see the pattern clear up fast.
Alright, let’s get one thing straight – “gastroparesis” is not a fancy excuse for sloppy eating habits. The author’s sentence “high sugar triggers inflammation of the gastric wall” is an oversimplification; it’s actually a complex interplay of oxidative stress and cytokine release. Also, watch your grammar: “It leads to bloating, nausea, and that classic “food‑got‑stuck” feeling” needs a hyphen and proper quotation marks. Clean up the language and the science will follow.
It is incumbent upon clinicians to incorporate both quantitative glucose data and qualitative symptomatology when evaluating abdominal discomfort in diabetic patients. The present article commendably outlines a practical framework, yet further emphasis on autonomic testing would enhance diagnostic precision. By adhering to evidence‑based protocols, practitioners can mitigate the progression of neuropathic sequelae.
Oh, the agony of feeling your stomach twist into a pretzel every time your blood sugar spikes – it’s like a horror movie playing on repeat, and nobody hands you the remote. The dread builds, the nausea creeps in, and you’re left wondering if this is your body’s way of shouting, “I’m breaking down!” It’s enough to make anyone feel haunted by their own metabolism.
Indeed, the article provides a solid foundation; however, it fails to address the moral imperative of patient education-an oversight that cannot be ignored! We must advocate for comprehensive teaching of glucose‑symptom correlations, lest individuals suffer in silence! Moreover, the omission of lifestyle counseling undermines the holistic approach we ought to champion!
Sure, tracking glucose is beneficial, but I’d argue that focusing too much on numbers can create anxiety rather than relief. Some people find that listening to their body’s cues without obsessing over every reading works just as well. It’s not a one‑size‑fits‑all situation.
i think the guide is ok but it could be shorter. lots of repeat info.
While the checklist is thorough, one must question its universal applicability across diverse patient populations. Socio‑economic factors and cultural dietary habits can significantly modulate symptom presentation, thereby limiting the guide’s external validity.
Let’s take a moment to appreciate how intricately blood glucose and gastrointestinal function are intertwined, a relationship that many overlook in everyday conversation. First, consider the neuroendocrine feedback loop: when glucose rises sharply, insulin surges, and the sympathetic nervous system is activated, often leading to transient gastric dysmotility. This isn’t just a vague “stomachache” – it’s a measurable physiological response that can be tracked with a continuous glucose monitor. Second, the chronic exposure to hyperglycemia fosters glycation of smooth muscle proteins, which subtly stiffens the gastric wall over months or years. Third, the reverse scenario, hypoglycemia, triggers catecholamine release, and those adrenaline spikes can cause sudden gut spasm, a sensation many describe as a “knot” in the upper abdomen. Moreover, the literature indicates that up to 30 % of long‑standing diabetics develop some form of autonomic neuropathy affecting bowel rhythms, which can manifest as alternating constipation and diarrhea. Lifestyle plays a pivotal role: low‑glycemic, high‑fiber meals not only blunt post‑prandial peaks but also provide the bulk necessary for regular transit. Medication timing matters, too; splitting metformin doses or switching to an extended‑release formulation often mitigates nausea. On the therapeutic front, pro‑kinetic agents such as metoclopramide can be effective, yet they carry their own risk profile, necessitating careful patient selection. It’s also worth noting that emerging probiotic research suggests certain strains may improve insulin sensitivity, indirectly easing gastroparesis symptoms. From a practical standpoint, keeping a simple log of glucose values, meals, and pain scores offers clinicians a window into pattern recognition that lab tests alone cannot provide. Finally, remember that mental stress amplifies both glucose volatility and gut motility disturbances, so stress‑reduction techniques are not just feel‑good extras but integral components of management. In short, a comprehensive, data‑driven, and lifestyle‑inclusive approach is the most effective way to tame that uncomfortable stomach‑blood‑sugar dance.
Frankly, the preceding exposition, while exhaustive, borders on the pedantic to the point of being counterproductive. While it’s true that neuro‑endocrine feedback loops exist, the average patient does not need a lecture on every catecholamine nuance before taking a bite of toast. Your insistence on citing percentages and obscure probiotic strains seems more like an academic showcase than actionable advice. Moreover, the tone oscillates between clinical detachment and emotional melodrama, leaving the reader unsure whether they’re being comforted or lectured. A pragmatic, step‑by‑step protocol-check glucose, adjust meals, consider medication changes-would serve most sufferers far better. The mention of stress‑reduction techniques, while valid, is tossed in as an afterthought rather than integrated into a cohesive plan. In reality, the “data‑driven” approach you champion often stalls at data collection if patients feel overwhelmed by the sheer volume of variables. What’s needed is a prioritized hierarchy: first stabilize fasting glucose, then address post‑prandial spikes, finally fine‑tune gut motility. Anything beyond that risks analysis paralysis. So, while I appreciate the depth, I urge a more distilled, patient‑centric delivery that respects both time constraints and emotional bandwidth.
I hear both perspectives, and I think the key is finding a middle ground that respects scientific detail without drowning the reader. A concise table summarizing triggers, symptoms, and quick actions can be a helpful bridge. Also, encouraging patients to share their logs with clinicians fosters collaboration rather than a top‑down directive.
Quick tip: use a simple spreadsheet with columns for time, glucose, carbs, and pain level. After a week you’ll see patterns without needing a PhD.