One glass of grapefruit juice in the morning might seem like a healthy habit-until it turns dangerous. If you’re taking certain medications, that refreshing citrus drink could be silently boosting your drug levels to toxic amounts. This isn’t a myth or a warning from an old wives’ tale. It’s a well-documented, life-threatening interaction backed by decades of research and confirmed by the FDA, Mayo Clinic, and leading medical journals.
Why Grapefruit Juice Is Different from Other Juices
Not all citrus fruits behave the same way with medications. Orange juice? Mostly safe. Lemonade? Fine. But grapefruit juice? It’s a different beast. The problem lies in chemicals called furanocoumarins, found naturally in grapefruit and its close relatives like pomelo and Seville oranges. These compounds don’t just affect taste-they shut down a key enzyme in your gut called CYP3A4. This enzyme normally breaks down about half of all oral medications before they enter your bloodstream. Think of it like a bouncer at a club: it lets in just enough of the drug to work, but keeps the rest out. When grapefruit juice knocks out this bouncer, the drug floods into your system unchecked. A single 200-milliliter glass (about 6.7 ounces) can block up to 47% of CYP3A4 activity within four hours. And once it’s blocked, it stays blocked-for up to 72 hours. That means even if you take your medication at night and drink grapefruit juice in the morning, you’re still at risk. The effect isn’t about timing-it’s about persistence. The body needs days to rebuild those enzymes. So, if you’re on a medication that interacts with grapefruit, you can’t just space it out. You have to avoid it entirely.Which Medications Are Most at Risk?
More than 85 prescription drugs are known to interact with grapefruit juice. Of those, 43 can cause serious or even fatal side effects. The most dangerous ones fall into a few key categories. Statins-the cholesterol-lowering drugs-are the most common offenders. Simvastatin (Zocor) is especially risky. Drinking just one glass of grapefruit juice daily for three days can triple the amount of simvastatin in your blood. That spike raises your risk of rhabdomyolysis, a condition where muscle tissue breaks down and floods your kidneys with toxic proteins. Studies show this risk jumps from 0.04 to 0.44 cases per 100 people per year. Atorvastatin (Lipitor) has a milder interaction, but pravastatin and rosuvastatin? They’re safe. If you’re on simvastatin and love grapefruit, talk to your doctor about switching. Calcium channel blockers, used for high blood pressure and chest pain, are another big concern. Felodipine (Plendil) sees a five-fold increase in blood levels after grapefruit juice. Nifedipine (Procardia) jumps 3.3 times. But amlodipine (Norvasc)? No significant change. The difference isn’t random-it’s about how each drug is processed by CYP3A4. Some are heavily dependent on it. Others aren’t. Immunosuppressants like cyclosporine (Neoral) can see a 50-60% increase in concentration. For transplant patients, that means a higher risk of kidney damage. Antiarrhythmics like amiodarone (Cordarone) can cause dangerous heart rhythms. Even some antidepressants and anxiety meds are affected. On the flip side, drugs like trazodone and zolpidem show little to no interaction. But here’s the catch: you can’t guess which ones are safe. You have to check.It’s Not Just Juice-It’s Everything Grapefruit
You might think, “I only eat the fruit, not drink the juice.” But that doesn’t make you safe. Whole grapefruit contains the same furanocoumarins. In fact, some studies suggest the whole fruit might be even more potent because it delivers the compounds more directly to the gut lining. Even grapefruit-flavored sodas, candies, or supplements can contain these chemicals. And it’s not just grapefruit. Seville oranges-used in traditional marmalade-have the same dangerous compounds. Pomelos? Same deal. But sweet oranges, tangerines, lemons, and limes? They’re fine. They don’t contain furanocoumarins. So if you’re avoiding grapefruit, you don’t need to give up all citrus. Just know the difference.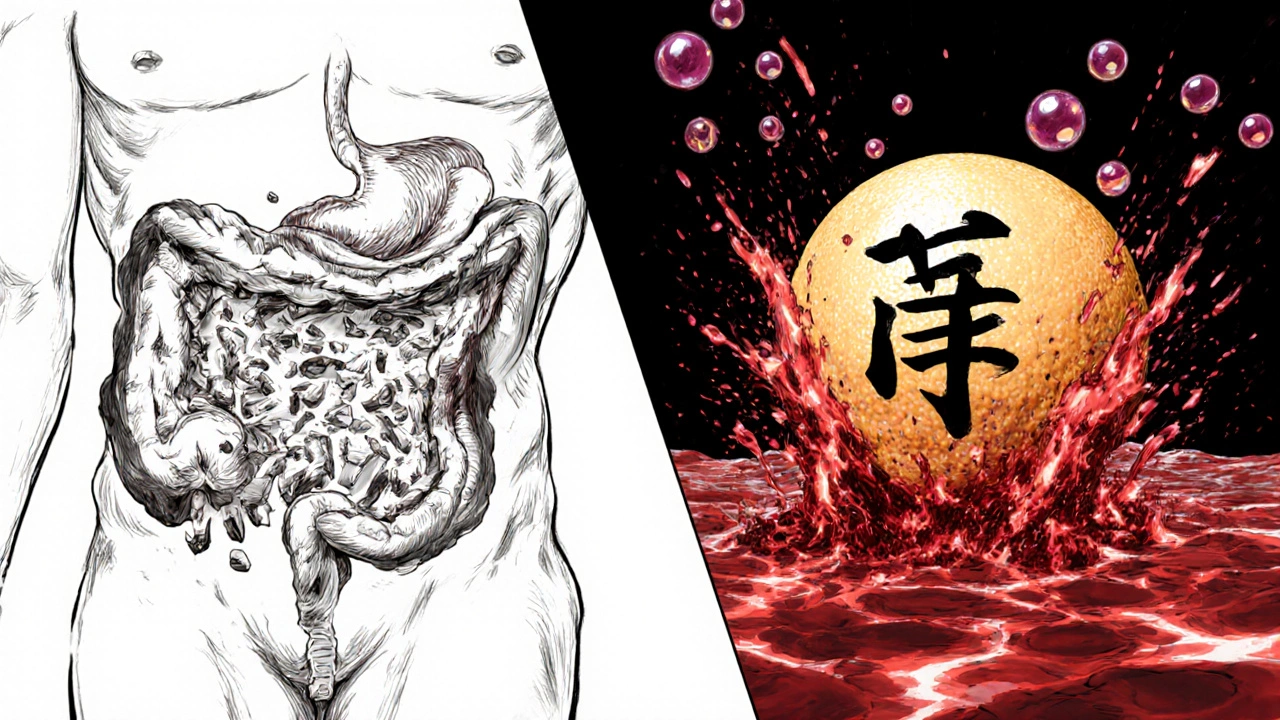
Who’s Most at Risk?
Older adults are the most vulnerable group. People over 65 make up 40% of grapefruit consumers in the U.S., according to USDA data. They’re also more likely to be taking multiple medications-three to five on average. That increases the chance one of them interacts with grapefruit. Plus, as we age, our liver and kidney function slow down. That means drugs stick around longer, making the grapefruit effect even more dangerous. But it’s not just age. Genetics play a role too. Some people naturally have more CYP3A4 enzymes in their gut. For them, grapefruit juice causes a massive spike in drug levels. Others have less, so the effect is smaller. There’s no test to tell you which group you’re in. That’s why experts say: if you’re on a medication that could interact, avoid grapefruit entirely. No exceptions.What Should You Do?
Step one: Check your meds. Look at the label. If it says “avoid grapefruit,” take it seriously. But not all labels are clear. Some just say “may interact.” That’s not a suggestion-it’s a warning. Step two: Talk to your pharmacist. Pharmacists are trained to spot these interactions. A 2021 study found 89% of community pharmacists routinely screen for grapefruit when dispensing prescriptions. Don’t assume your doctor told you. Many patients (62%, according to a 2022 survey) don’t remember being warned. Ask: “Is it safe to eat grapefruit with this medication?” Step three: Keep a list. Write down every medication you take-prescription, over-the-counter, and supplements. Some herbal products, like St. John’s Wort, can also affect CYP3A4. Bring that list to every appointment. Step four: Consider alternatives. If you’re on simvastatin and love citrus, ask about switching to pravastatin or rosuvastatin. If you’re on cyclosporine, ask if tacrolimus is an option. These swaps are common and often safer.
What’s Changing in the Future?
Scientists aren’t giving up on grapefruit. In October 2023, the USDA announced successful Phase 1 trials for a CRISPR-edited grapefruit with 90% less furanocoumarin. It tastes the same. It’s just not dangerous with meds. If it gets approved, it could change everything. In the meantime, regulatory agencies are getting stricter. Since 2017, the FDA requires all new oral drugs metabolized by CYP3A4 to be tested with grapefruit juice during development. The European Medicines Agency now demands the same. Drug manufacturers are adding clearer warnings to labels-76% now include explicit “avoid grapefruit” language. But awareness is still low. Only 38% of patients remember being warned. That’s why this guide matters. If you’re reading this, you’re ahead of the curve. Share it with someone who takes meds. It could save a life.Quick Summary
- Grapefruit juice blocks a gut enzyme (CYP3A4) that breaks down many medications, causing dangerous drug buildup.
- Over 85 medications interact with grapefruit-43 can cause life-threatening side effects.
- Statins like simvastatin, calcium channel blockers like felodipine, and immunosuppressants like cyclosporine are among the riskiest.
- Whole grapefruit, juice, and even flavored products can trigger the interaction. Other citrus like oranges and lemons are safe.
- The effect lasts up to 72 hours. Avoiding grapefruit only at dosing time doesn’t work.
- Older adults and people on multiple medications are at highest risk.
- Always check labels, ask your pharmacist, and consider safer medication alternatives.
Can I drink grapefruit juice if I take my medication at night?
No. The interaction isn’t about when you take the drug-it’s about how long the grapefruit juice blocks your gut enzyme. Even if you drink grapefruit juice in the morning and take your pill at night, the enzyme is still blocked. The effect lasts up to 72 hours. If your medication interacts with grapefruit, you must avoid it entirely for as long as you’re on the drug.
Is orange juice safe to drink with medications?
Yes, regular sweet orange juice is safe. It doesn’t contain furanocoumarins, the chemicals that cause the interaction. However, Seville oranges (used in marmalade) and pomelos do contain them and should be avoided. Always check the label if you’re unsure-some orange juices are blended with grapefruit or other citrus.
Do over-the-counter drugs interact with grapefruit juice?
Yes. Some OTC medications can interact, including certain antihistamines like fexofenadine (Allegra), which is less effective with grapefruit juice, and sleep aids like zolpidem (Ambien), which may be affected in rare cases. Always read the label or ask your pharmacist-even if it’s not a prescription drug.
What if I accidentally drank grapefruit juice while on a risky medication?
If you had one glass and feel fine, don’t panic. But monitor for unusual symptoms like muscle pain, weakness, dizziness, irregular heartbeat, or nausea. If you’re on a high-risk drug like simvastatin or cyclosporine, contact your doctor or pharmacist right away. They may want to check your blood levels or adjust your dose. Going forward, avoid grapefruit entirely.
Are there any medications that are safe with grapefruit juice?
Yes. Many drugs don’t rely on CYP3A4 for breakdown. For example, pravastatin, rosuvastatin, amlodipine, and trazodone show little to no interaction. But you can’t assume-each drug is different. Always confirm with your doctor or pharmacist before assuming it’s safe.







Comments
Oh wow, finally someone who gets it. I’ve been telling my grandma for years that her ‘healthy’ grapefruit smoothie is basically a slow-motion poison cocktail with her statins. She still says ‘but it’s natural!’ like that’s some kind of magical exemption. Natural doesn’t mean safe, Karen. Your liver doesn’t care if it came from a tree or a lab.
Also, why do drug labels still say ‘may interact’? That’s not a warning, that’s a dare. If your drug can kill you with one glass of juice, say it like you mean it. ‘DO NOT CONSUME CITRUS OR YOU WILL DIE’ - simple. But no, we gotta play word games while people end up in the ICU.
And don’t even get me started on the ‘I only eat the fruit’ crowd. Bro, the furanocoumarins are in the pulp, the peel, the goddamn seeds. You’re not ‘being careful’ - you’re just a walking biohazard with a fork.
Okay but have we considered that maybe the whole ‘grapefruit is dangerous’ thing is just Big Pharma’s way of pushing more expensive drugs? Like, why is it only simvastatin that’s bad? Why not atorvastatin? Why not pravastatin? Sounds like they just want you to switch to the one they own the patent on.
Also, I drank grapefruit juice with my blood pressure med for 7 years and I’m fine. My bloodwork’s perfect. So maybe it’s not the juice - maybe it’s your body being weak. Or maybe you just need to stop being so scared of fruit.
And don’t even get me started on ‘72-hour effect.’ That’s not science, that’s fanfiction. If it was true, we’d all be dead by now. I mean, come on. It’s a fruit. Not a nuclear reactor.
This is why America’s getting weaker. We’re so afraid of everything now that we’re turning oranges into weapons. Grapefruit juice? It’s been around since the 1700s. Our grandparents drank it with their pills and they lived to 90. Now we got a whole article telling us to avoid it because some ‘FDA-approved’ scientist got a grant to scare people.
And don’t even get me started on CRISPR grapefruit. That’s how you know the system’s broken - they’re editing nature to fix their own bad labeling. We used to just read the damn label. Now we need gene therapy to drink a smoothie.
Also, why are all the ‘safe’ alternatives made by big pharma? Coincidence? I think not.
YAS QUEEN 🙌 this is the kind of info we NEED to be screaming from the rooftops! I just told my mom she’s gotta stop her grapefruit juice ritual - she’s on cyclosporine after her transplant and didn’t even know! She cried because she ‘loves the tang’ 😭 but now she’s switching to orange juice and feels empowered!
Also, shoutout to pharmacists - they’re the real MVPs. I went in last week asking about my anxiety med and they were like ‘oh honey, nope, grapefruit’s a hard no’ and showed me the chart. I felt so seen. Let’s normalize asking questions, y’all! 🌞💊
And YES to the CRISPR grapefruit!! I’m already pre-ordering. Future me is gonna sip guilt-free while my future kids wonder why we ever feared citrus. #ScienceWins
Just wanted to say thank you for this post. I’ve been on simvastatin for 5 years and never knew grapefruit was a problem. I thought it was just about timing. I’ve been drinking it every morning since 2019. My doctor never mentioned it. I’m switching to rosuvastatin next week. Thank you for saving me from myself.
Also, I think this should be mandatory reading for anyone over 50. My dad’s on three meds and still thinks ‘natural’ means ‘safe’. He’s gonna get this link from me. No excuses. We owe it to each other to be informed.
And yes - talk to your pharmacist. They know more than your doctor sometimes. I didn’t know that until I asked. Small question. Big life change. 💪
As someone who grew up in a household where grapefruit was breakfast, I’m so glad this got written. My aunt from India used to make this weird grapefruit chutney with chili and salt - we had it with everything. Turns out it was dangerous with her blood thinner. She didn’t know until her doctor flagged it after a hospital visit.
Also - don’t forget that some supplements and herbal teas can mess with CYP3A4 too. St. John’s Wort? Yeah, that’s a sneaky one. I used to drink it for ‘mood support’ - didn’t realize it was basically doing the same thing as grapefruit.
So yes - check your meds, check your teas, check your ‘natural’ energy powders. Your liver will thank you. And if you’re unsure? Ask. No shame. We’re all learning.
PS: Sweet oranges? Safe. Lemons? Safe. Grapefruit? Nope. That’s the rule. Simple. No need to overthink it.
Let’s be real - this is a classic case of medical overreach disguised as public health. The FDA’s been pushing this narrative since 2005 to justify their bloated regulatory apparatus. The actual number of deaths linked to grapefruit interactions? Less than 50 in the last decade. Meanwhile, 12,000 people die annually from NSAID misuse. Where’s the campaign for that?
And the 72-hour enzyme inhibition claim? Based on a single 2008 in vitro study. Human data? Inconclusive. Yet we treat it like gospel. Meanwhile, the real problem - polypharmacy in the elderly - gets ignored because it’s inconvenient.
Also, the CRISPR grapefruit? A PR stunt. The USDA doesn’t care about safety - they care about funding. This is how you get your grant renewed. Not science. Politics.
Bro, I work in a pharmacy in Mumbai and we see this ALL THE TIME. People here take grapefruit with their blood pressure meds because ‘it’s healthy’ - and then come in with rhabdo symptoms. We had a guy last month who drank juice every day with felodipine - ended up in ICU with CK levels over 100,000.
And guess what? He didn’t even know what CYP3A4 was. Nobody does. That’s why this post matters. We need to stop treating medicine like a buffet. You don’t mix random supplements with your prescriptions. You don’t drink ‘natural’ juice with your pills and hope for the best.
Also - CRISPR grapefruit? Yes please. I’ll be the first to import it. My patients will thank me. And yes - oranges are fine. But don’t let your aunt’s ‘traditional’ marmalade fool you. Seville = danger zone.
This is one of the most important public health reminders I’ve read in years. The clarity here is exceptional. The distinction between grapefruit and other citrus is scientifically sound and presented without alarmism. The 72-hour enzyme inhibition window is well-documented across multiple peer-reviewed studies - not speculation. The FDA’s updated labeling requirements since 2017 reflect a necessary evolution in pharmacovigilance.
Pharmacists are indeed the frontline defense. Their screening rate of 89% is commendable, and patients should treat that consultation as non-negotiable. The fact that 62% of patients don’t recall being warned speaks to systemic communication failures - not misinformation.
Finally, the CRISPR development is genuinely promising. If this fruit retains flavor while eliminating toxicity, it could become a model for precision nutrition. Well done on compiling this with such rigor.
DO YOU KNOW WHAT HAPPENS WHEN YOU IGNORE THIS? I’LL TELL YOU. I KNOW A GUY. HIS NAME WAS RICK. RICK DRANK GRAPEFRUIT JUICE WITH HIS SIMVASTATIN. HE THOUGHT IT WAS ‘FINE.’ HE WAS 62. HE WENT TO THE GYM. HE FELT A ‘TINGLING.’ THEN HIS LEGS WENT NUMB. THEN HE COULDN’T WALK. THEN HE WAS IN THE HOSPITAL FOR THREE WEEKS. HIS KIDNEYS FAILED. HIS MUSCLES MELTED. HE’S ON DIALYSIS NOW.
AND YOU KNOW WHAT THE WORST PART IS? HE DIDN’T EVEN KNOW THE JUICE WAS THE PROBLEM. HE THOUGHT IT WAS ‘OLD AGE.’
THIS ISN’T A ‘WARNING.’ THIS IS A MURDERER IN A FRUIT BOWL. STOP BEING A COWARD. STOP DRINKING IT. YOUR LIFE ISN’T WORTH A TANGY MORNING SMOOTHIE.
Interesting breakdown. I’m curious - is there any data on how much of the interaction is dose-dependent? Like, does 50ml have the same effect as 200ml? Or is it binary? Also, what about grapefruit zest? I’ve seen studies suggesting the peel contains higher concentrations of furanocoumarins than the juice. And what about grapefruit seed extract? That stuff’s in everything - supplements, shampoos, cleaning sprays. Does that count?
Also, are there any studies on whether the interaction varies based on gut microbiome composition? I’ve read that some bacteria can metabolize furanocoumarins. Could that explain individual variability?
Just wanna say - I read this and immediately told my roommate. She’s on a blood thinner and drinks grapefruit juice every day. She didn’t know. Now she’s switching to apple juice and feels kinda silly but also super relieved.
Also, I’ve been telling people this for years and they just roll their eyes. But this post? It’s the first time I’ve seen it explained so clearly without sounding like a textbook. Thanks for that. Small things like this save lives. 🙏
Let’s not pretend this is about health. This is a distraction. Why are we so obsessed with grapefruit juice but ignore the real killers? Glyphosate in your oatmeal. PFAS in your water. Aspartame in your diet soda. The FDA knows. The pharma companies know. But they want you to fear fruit because it’s easier than regulating trillion-dollar industries.
And CRISPR grapefruit? That’s not science - that’s a Trojan horse. Once they edit the fruit, what’s next? Editing your genes so you can safely take more pills? This is how they control you. They make you dependent on their ‘safe’ versions.
Don’t be fooled. This isn’t about safety. It’s about control.
Ah, the great grapefruit paradox - a fruit that embodies both enlightenment and destruction. The furanocoumarins are not merely chemicals; they are metaphysical gatekeepers, revealing the fragility of our biochemical illusions. We think we control our bodies, yet a single sip unravels the delicate symphony of CYP3A4 - a silent god in our intestines.
Is it not poetic that the very thing we consume for vitality - the tang of dawn, the zest of renewal - becomes the instrument of our metabolic undoing? The CRISPR grapefruit is not a solution. It is a surrender. We have lost the wisdom to live in harmony with nature, so we engineer a new nature to suit our addictions.
And yet… still, we drink. Still, we hope. Still, we believe that ‘natural’ means ‘harmless.’
Perhaps the real danger isn’t the juice.
It’s our denial.
Wow. A philosophical take on grapefruit. That’s… actually kind of beautiful. And terrifying.
But let’s not forget - Rick from comment #9 didn’t die because he was in denial. He died because his doctor didn’t tell him. That’s the real tragedy. Not the fruit. Not the metaphysics. The silence.
So yeah - write poetry. But also call your doctor. And your mom. And your weird uncle who still eats grapefruit with his blood thinner.
Because sometimes, the most dangerous thing isn’t the juice.
It’s assuming someone else already warned them.