Breastfeeding Medication Safety Checker
Check Antidepressant Safety During Breastfeeding
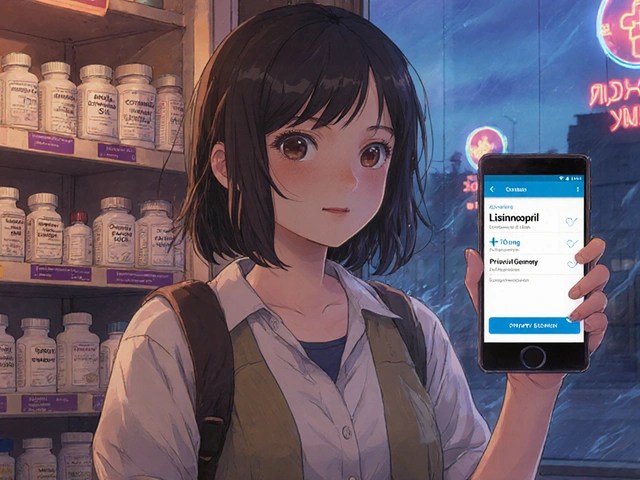
Select your antidepressant to see its Relative Infant Dose (RID) and safety profile while breastfeeding.
Postpartum depression is a mood disorder that hits about one in eight new mothers, causing deep sadness, anxiety, and trouble functioning beyond the usual "baby blues". It can start within the first weeks after delivery and may linger for months if left untreated. For many families, the big question isn’t just "how do I feel better?" but also "can I keep nursing my baby safely while taking medication?" This guide breaks down the science, the safest drug choices, and the practical steps you can take to protect both mom and infant.
Understanding Postpartum Depression
The Edinburgh Postpartum Depression Scale (EPDS) is the go‑to screening tool. A score of 13 or higher suggests a need for further evaluation. Health‑care providers usually administer it during well‑baby visits at 1, 2, 4, and 6 months, according to the American Academy of Pediatrics (AAP). Early detection lets you start treatment before symptoms worsen and before they interfere with bonding or breastfeeding.
Why Treating PPD Matters for Mom and Baby
Untreated depression isn’t just a mood issue; it raises the risk of poor infant weight gain, disrupted sleep, and even long‑term developmental challenges. The CDC emphasizes that the danger of leaving a mother untreated outweighs the theoretical risks of medication exposure through breast milk. In other words, getting mom back to feeling like herself is a critical part of keeping the whole family healthy.
Antidepressant Options While Breastfeeding
Not all antidepressants are created equal when it comes to milk transfer. The key metric is the Relative Infant Dose (RID), which compares the infant’s daily exposure to the mother’s weight‑adjusted dose. An RID below 10 % is generally considered compatible with nursing.
Below is a quick snapshot of the most commonly prescribed agents and their typical RID ranges:
| Medication | Class | Typical RID | Notes |
|---|---|---|---|
| Sertraline | SSRI | 0.5‑3.2 % | First‑line; infant serum often undetectable |
| Paroxetine | SSRI | 0.9‑8.6 % | Low transfer, good tolerability |
| Citalopram | SSRI | 3.5‑8.9 % | Watch QT interval at high doses |
| Fluoxetine | SSRI | 5.9‑15.2 % | Long half‑life; metabolites can accumulate |
| Amitriptyline | TCA | <2 % | High protein binding; good safety record |
| Venlafaxine | SNRI | 1.4‑5.9 % | Case reports of infant irritability at high maternal doses |
| Mirtazapine | NaSSA | ~4 % | Limited data; monitor feeding patterns |
| Bupropion | NEU | 6‑10 % | Potential seizure risk in infants; use cautiously |
| Zuranolone | Neurosteroid | 0.5‑1.5 % | First oral PPD‑specific drug; data limited, advise pumping & discarding for 1 week post‑treatment |
What does this mean in plain language? Sertraline and paroxetine consistently show the lowest infant exposure and the strongest safety record, so they’re the go‑to choices for most nursing moms. Fluoxetine and doxepin sit at the risky end, mainly because their metabolites linger in the baby’s system.

How to Assess Safety: RID and Monitoring
When you start an antidepressant, calculate the RID (you can find calculators online or ask your pharmacist). If the RID is under 10 %, you’re in the safe zone according to LactMed.
- First two weeks: watch for excessive sleepiness, poor feeding, or unusual fussiness. These are the red flags Dr. Thomas Hale highlights for infants under two months.
- Four‑week check‑in: reassess the mother’s EPDS score and ask how the baby is doing. If there’s any concern, you can order a single infant serum level-though it’s rarely needed.
- Timing doses: many clinicians suggest taking the medication right after a feeding session, then waiting 2‑3 hours before the next bout. This creates the largest gap between peak milk concentration and the baby’s next suck.
Practical Steps for Clinicians and Moms
- Screen early. Use the EPDS at 1‑month well‑visit.
- Choose the safest drug first. Start sertraline 25 mg daily; if not effective after 4‑6 weeks, consider increasing to 50 mg.
- Educate about RID. Show moms how to read the LactMed entry for their chosen medication.
- Set a monitoring plan: daily log of infant’s sleep, feeding, and mood for the first month.
- If side effects appear, adjust dose or switch to an alternative with a lower RID (e.g., from fluoxetine to sertraline).
- Document everything in the electronic health record, including the mother’s consent to breastfeed while on medication.
Remember, abrupt discontinuation can cause a relapse that’s three times more likely, according to the Cleveland Clinic. Taper slowly if you need to stop.

Emerging Treatments and What to Watch
Zuranolone (brand name Zurzuvae) made headlines in August 2023 as the first oral pill specifically approved for PPD. Trials showed about 50 % of participants hit remission within two weeks. However, the label still says there’s no human‑milk data, so the current ACOG recommendation is to pump and discard milk for one week after finishing the course.
Research is moving toward personalized risk assessment. A 2022 JAMA Pediatrics study found infants with a CYP2D6 poor‑metabolizer genotype had 3.2‑fold higher venlafaxine levels after breastfeeding exposure. While routine genetic testing isn’t standard yet, it signals a future where doctors might tailor drug choice based on the baby’s expected metabolism.
Long‑term studies, like the B.R.I.D.G.E. cohort, are tracking neurodevelopment up to two years of age for kids exposed to SSRIs through milk. Early results suggest no major differences, but the final data won’t be out until late 2024, so clinicians continue to rely on short‑term safety data.
Key Takeaways
- Untreated PPD carries greater risk than most antidepressant exposures via breast milk.
- Sertraline and paroxetine are the safest first‑line options (RID < 5 %).
- Calculate RID, monitor the infant for the first month, and time doses after feeds.
- Emerging drugs like zuranolone look promising but require cautious breastfeeding practices.
- Regular EPDS screening and open communication with your health‑care team are essential.
Can I breastfeed while taking sertraline?
Yes. Sertraline has one of the lowest RID values (0.5‑3.2 %). Most studies report undetectable infant serum levels and no noticeable side effects.
What should I do if my baby seems unusually sleepy after I start an antidepressant?
Contact your pediatrician right away. Ask for an infant serum level if advised, and consider switching to a medication with a lower RID.
Is it safe to use fluoxetine while breastfeeding?
Fluoxetine has a higher RID (up to 15 %) and a long half‑life, so it can accumulate in the infant. It’s generally reserved for mothers who can’t tolerate sertraline or paroxetine and who are monitored closely.
How long should I wait after stopping an antidepressant before I can breastfeed freely?
For most SSRIs, wait 24‑48 hours after the last dose to allow the drug to clear from milk. For longer‑acting agents like fluoxetine, a 5‑7‑day washout is safer.
What resources can help me make a decision about medication and breastfeeding?
The LactMed database, the InfantRisk Center hotline, and the CDC’s postpartum‑depression fact sheet are all reliable, up‑to‑date sources. Your OB‑GYN or psychiatrist can also walk you through the RID calculations.







Comments
I’m a mom of two and I can tell you firsthand how terrifying postpartum depression feels – the darkness, the guilt, the endless self‑doubt 😢. When I finally got my diagnosis, the first thing on my mind was “Can I still breastfeed my baby while I’m on meds?” – because I didn’t want to break that precious bond. I started on sertraline after talking to my OB‑GYN, and we monitored the infant’s weight and behavior every week 😊. The RID for sertraline is famously low, usually under 3 %, so the pediatrician said the risk was minimal. My baby didn’t show any signs of sedation or feeding issues, and the mood‑lifting effect on me was noticeable within two weeks. I also kept a feeding log and a mood diary, which helped me see the correlation between stable med levels and calmer evenings. If you’re worried about the half‑life, remember that sertraline clears relatively quickly compared to fluoxetine, which can linger and pile up in milk. I was also told to watch for any rash or jitteriness in the infant, but none appeared. The key was regular follow‑ups – the AAP recommends checking at 1, 2, 4, and 6 months, which gave me reassurance every step of the way. When the anxiety peaked, I used breathing exercises and short walks with the stroller; those moments of fresh air kept my cortisol from spiking. The community support groups on Facebook were lifesavers – hearing other moms say “I’m doing okay on citalopram, the RID is about 5 % and my baby is thriving” made me feel less alone. Even the CDC data backs the idea that untreated PPD poses a bigger risk than the tiny drug exposure through milk. So, my advice is: don’t let fear stop you from getting help, talk openly with your provider, and stay vigilant with your baby’s cues. If you ever feel overwhelmed, reach out to a lactation consultant; they can suggest timing doses right after a feeding to further reduce exposure. Remember, taking care of yourself is the best thing you can do for your child 💪.
Everyone knows pharma pushes meds onto new moms-they’re just selling chemicals, not cures.
The pharmacokinetic profiles cited in peer‑reviewed journals indicate that certain selective serotonin reuptake inhibitors possess relative infant doses well below the ten percent threshold, thereby supporting clinical guidelines that endorse their cautious use during lactation.
lol i get why u’re scared but honestly most of these meds r low risk – just keep an eye on the baby’s feeding pattern and you’ll be fine, definetly worth the mental health boost.
One must resist the tempting allure of oversimplification; the nuanced interplay between maternal neurochemistry and infant development demands a rigorously evidence‑based approach, not the pedestrian reassurance that populates lay forums.
From a psychopharmacological systems‑biology perspective, the modulation of serotonergic transmission via high‑affinity SERT inhibition yields a favorable therapeutic index, especially when juxtaposed against the metabolic clearance rate (MCR) observed in lactational physiology 📈💊.
i think thats pretty cool – it means moms can get the help they need without feeling like they’re betraying their babies, sooo hopeful 😊.
Honestly, most of this info feels like academic fluff 😒.
While the presentation may appear dense, the underlying data substantiate the safety parameters delineated for selective serotonin reuptake inhibitors during nursing periods.
Stay strong, mama! 🚀 You’ve got the science on your side and the right meds can flip that depression script fast – no excuses, just action!
getting help is good.
The truth is clear: our nation’s health policy should champion evidence‑based treatment for postpartum depression, not hide behind outdated myths that threaten our mothers and future generations.