Medication Side Effect Risk Estimator
How Risky Is Your Medication?
This tool estimates the risk of serious side effects for common medications used by rural patients without proper monitoring. Select medications to assess risk and get telehealth solutions.
Why Rural Patients Need Better Side Effect Monitoring
When you live miles from the nearest clinic, a bad reaction to medication can turn dangerous fast. For rural and remote patients, side effects from drugs like blood thinners, antidepressants, or high blood pressure pills don’t just cause discomfort-they can lead to hospital trips, emergency transfers, or worse. The problem isn’t just distance. It’s timing. In urban areas, a patient might notice dizziness after starting a new drug and walk into their doctor’s office the next day. In rural areas, that same patient might wait three days just to get a ride to the clinic-and by then, their INR could be dangerously high, or their heart rate could be erratic.
According to the National Rural Health Association, 60 million Americans in rural areas face real barriers to care. Over 120 rural hospitals have closed since 2010. That means fewer local providers, fewer pharmacists, and fewer options when something goes wrong. And it’s not just about access-it’s about risk. Rural patients experience 23% more preventable adverse drug events than those in cities, per a 2020 Health Affairs study. Why? Because monitoring is patchy, delayed, or nonexistent.
How Telehealth Is Changing the Game
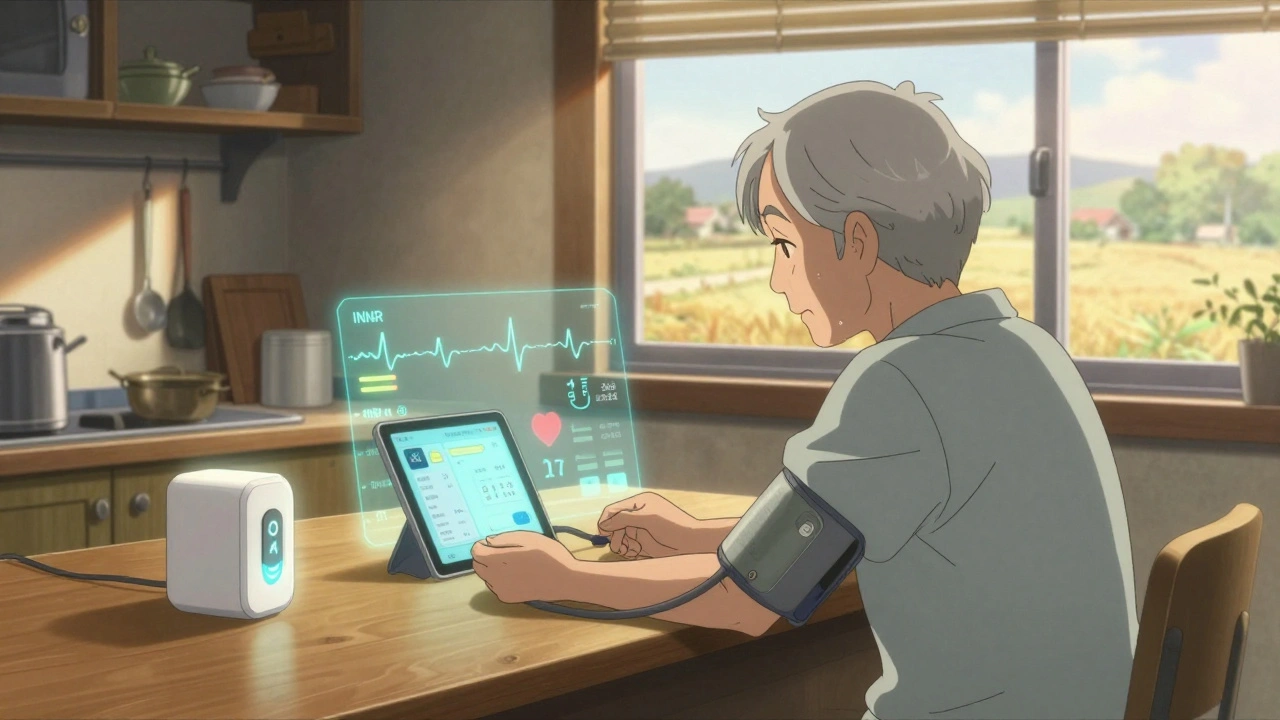
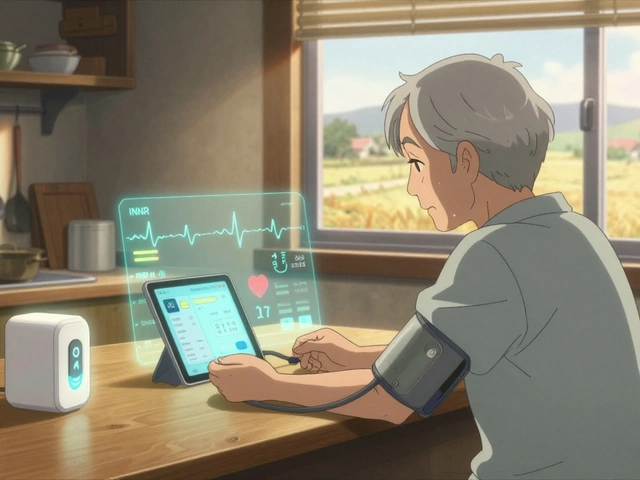
Telehealth isn’t just video calls anymore. It’s a system. A network of tools working together to catch side effects before they become emergencies. Remote patient monitoring (RPM) platforms now let patients track their own vital signs at home. A blood pressure cuff synced to an app can send readings directly to a nurse. A smart pill dispenser alerts providers if a dose is missed. These aren’t futuristic ideas-they’re in use right now in clinics across Montana, Mississippi, and Maine.
One of the biggest wins? Early detection. A patient in Montana using a blood thinner monitoring app reported an unusual spike in their INR levels. The system flagged it automatically. Within hours, their pharmacist called and adjusted their dose. They avoided a dangerous bleed. That’s the power of real-time monitoring. A 2022 review in the Journal of Medical Internet Research found telehealth reduced hospitalizations for medication side effects by 31% in rural populations.
What Tools Are Actually Working?
Not all tech is created equal. The most effective tools share three things: accuracy, simplicity, and integration.
- Bluetooth-enabled devices like INR monitors and smart blood pressure cuffs are FDA-cleared and track vital signs within ±3% accuracy. These connect to apps that auto-send data to care teams.
- Smart pill dispensers like Hero Health track when pills are taken. One study showed 85% accuracy in detecting missed doses-far better than patient self-reporting.
- Symptom check-in apps let patients tap a button to report nausea, dizziness, or confusion. These apps have been validated to match in-person assessments 78% of the time.
- Video platforms must be HIPAA-compliant and encrypted. Most use AES-256 encryption and run on iOS 14+ or Android 10+, which covers 92% of smartphones today.
But the real magic happens when these tools talk to each other. Successful programs integrate with electronic health records like Epic or Cerner. That way, when a patient’s blood pressure spikes, their provider sees it alongside their medication list, allergy history, and lab results-all in one place.
The Human Side: Who’s Behind the Screen?
Technology alone won’t fix this. You need people. The most effective rural telehealth programs don’t just send alerts-they assign care coordinators. These aren’t just nurses. They’re often pharmacists, trained to recognize subtle signs of drug reactions.
A 2023 American Pharmacists Association guideline found pharmacist-led telehealth monitoring boosted medication adherence from 62% to 89%. That’s huge. Pharmacists know how drugs interact. They spot patterns a busy doctor might miss. In one program at the University of Mississippi Medical Center, pharmacists held weekly video check-ins with anticoagulation patients. Patient retention hit 92%.
And it’s not just about clinical care. Many patients feel isolated. A simple video call where someone asks, “How are you really doing?” can make a difference. One Reddit user wrote: “My provider didn’t just check my numbers-they asked if I was sleeping. That’s the first time anyone cared in years.”
Barriers Still Standing in the Way
Let’s be honest: telehealth isn’t a magic fix. It’s got cracks.
- Connectivity: 28% of rural Americans don’t have broadband that meets federal standards. In some areas, 3G is the best you can get. That’s not enough for video calls.
- Age and tech skills: 34% of rural seniors struggle with smartphones. One West Virginia patient complained their video call was too blurry to see tremors. That’s not a tech failure-it’s a design failure.
- Training time: Patients need help. On average, they need two to three sessions just to learn how to use the tools. Older adults need even more-3.2 sessions on average.
- Reimbursement gaps: Medicare pays $51 for 20 minutes of remote monitoring. But only 63% of private insurers follow that rate. If clinics can’t get paid, they can’t keep the service running.
- Health literacy: 36% of rural adults have trouble understanding medical info. If a patient doesn’t know what “dizziness” means in a symptom checklist, they won’t report it.
And here’s the quiet crisis: as urban telehealth companies expand into rural areas, local clinics lose patients-and revenue. A 2022 study found telehealth services from outside providers could cut rural hospital income by 15%. That threatens the very infrastructure needed to support long-term care.
What Works in Practice: Real Examples
Some programs are getting it right. Here’s how:
- Multi-language support: 87% of successful programs offer materials in Spanish, Navajo, or other local languages.
- Tiered response protocols: Critical symptoms (like chest pain or swelling) trigger an immediate call. Moderate issues (like nausea) get a 24-hour follow-up. Minor complaints (like mild headache) are checked in 72 hours.
- Hybrid models: Some clinics combine video visits with mailed test kits. A patient takes an INR test at home, mails the sample, and gets results back in 48 hours.
- Dedicated staff: Programs with care coordinators see 34% higher patient engagement. These people don’t just answer calls-they proactively check in, troubleshoot tech issues, and even drive to patients’ homes to set up devices.
The University of Arkansas for Medical Sciences launched a pilot using wearable sensors to detect movement changes linked to antipsychotic side effects. It caught early signs of tardive dyskinesia with 91% accuracy. That’s the future-and it’s here.

What’s Next? AI, Policy, and Equity
The next wave is smarter. In 2023, the FDA approved AI tools like IBM Watson Health’s MedSafety system. These can predict side effects before they happen-with 84% accuracy. Imagine getting a warning that your new blood pressure drug might cause low potassium in three days. That’s not sci-fi. It’s happening.
Policy is catching up too. The 2023 CONNECT for Health Act now lets Medicare cover audio-only check-ins. That’s huge for patients without video capability. And the FCC’s $20.4 billion Rural Digital Opportunity Fund is trying to fix broadband gaps by 2025.
But equity remains a problem. Black rural patients are 1.8 times less likely to get telehealth monitoring than white patients. Why? Lack of access, distrust, or just plain oversight. No program can succeed if it leaves people behind.
What Patients and Providers Can Do Today
If you’re a patient in a rural area:
- Ask your provider: “Do you have a telehealth program for checking side effects?”
- Request training. Don’t assume you’ll figure it out alone.
- Use the symptom tracker-even if it’s just a paper form at first.
- If your video call is poor, say so. Ask for audio-only or mailed kits.
If you’re a provider:
- Start small. Pick one high-risk medication (like warfarin or SSRIs) and pilot a monitoring program.
- Partner with a pharmacist. They’re your secret weapon.
- Use free or low-cost tools. Many RPM platforms offer discounted rates for rural clinics.
- Track your outcomes. If hospital visits drop, you’ve got proof to secure funding.
Final Thought: It’s Not About Tech. It’s About Trust.
Telehealth tools are powerful. But they’re only as good as the relationship behind them. A rural patient won’t trust a machine. They’ll trust a person who remembers their name, who calls when they miss a check-in, who shows up-even if it’s just on a screen.
The goal isn’t to replace the clinic. It’s to extend it. To make sure that no matter how far you live from town, your medication won’t hurt you more than it helps.
Can telehealth really catch serious side effects before they become emergencies?
Yes. Real-world examples show it works. Patients using Bluetooth-enabled INR monitors have avoided dangerous bleeding episodes because their readings were flagged before symptoms appeared. A 2022 study found telehealth reduced hospitalizations for medication side effects by 31% in rural areas. Tools like smart pill dispensers and symptom apps catch missed doses and early warning signs-like dizziness or irregular heartbeat-hours or days before a crisis hits.
What if I don’t have good internet in my rural area?
You don’t need high-speed internet for all telehealth monitoring. Many programs now support audio-only calls, which work on basic cell service. Some use mailed test kits-for example, you take a blood sample at home and send it in for INR testing. Others offer low-bandwidth apps that send text-based symptom updates. The key is asking your provider what options exist. Medicare now covers audio-only monitoring, so it’s more accessible than ever.
Are these telehealth tools hard for older adults to use?
They can be-but they don’t have to be. Many patients over 65 need extra help. Successful programs offer in-person setup visits, step-by-step printed guides, and family training sessions. On average, older adults need about 3.2 training sessions to feel comfortable. Some clinics even assign a “tech buddy”-a volunteer or staff member who calls weekly to help troubleshoot. The tools are getting simpler too: one-button devices and voice-activated prompts are becoming more common.
Why do some rural clinics say telehealth is hurting their revenue?
When big telehealth companies from cities start offering services to rural patients, those patients may stop traveling to the local clinic. That means fewer in-person visits-and less revenue for the clinic. A 2022 study found this could reduce rural hospital income by up to 15%. The solution? Integrate telehealth into the local system. Train your own staff. Use local pharmacists. Make sure the money from telehealth visits stays in the community. Otherwise, you risk losing the very infrastructure you need to care for patients long-term.
What medications are most dangerous for rural patients without monitoring?
Anticoagulants (like warfarin), antihypertensives (like beta-blockers), and psychotropic drugs (like SSRIs and antipsychotics) are the top three. These drugs have narrow safety margins-small changes in dose or body response can cause serious side effects. For example, warfarin can cause internal bleeding if not monitored. Antidepressants can trigger serotonin syndrome. Blood pressure meds can cause dangerous drops in heart rate or kidney stress. All of these require regular check-ins. Without monitoring, rural patients are at much higher risk.
Is telehealth monitoring covered by insurance?
Medicare covers remote patient monitoring at $51 for every 20 minutes of clinical time. Medicaid coverage varies by state. Private insurers are slower to follow-only 63% pay the same rate. Some states have passed laws requiring parity. Always ask your provider if they bill for RPM codes (like 99453, 99454, 99457). If they don’t, it may be because they’re unaware-or because they can’t get paid. Advocacy matters: if enough patients ask, providers will make it happen.
Can AI really predict side effects before they happen?
Yes, and it’s already being used. In 2023, the FDA approved AI tools like IBM Watson Health’s MedSafety system, which analyzes medication history, lab results, and patient-reported symptoms to predict adverse reactions with 84% accuracy. These systems don’t replace doctors-they flag risks early. For example, if a patient on a new antidepressant starts reporting fatigue and headaches, the AI might warn that serotonin syndrome is possible. This gives the care team time to adjust the dose before the patient gets sicker.
How can I help a rural loved one start telehealth monitoring?
Start by talking to their provider. Ask if they offer remote monitoring for their medications. If not, suggest they look into programs from organizations like the National Rural Health Association. Offer to help set up the app or device. Go with them to the first training session. Make sure they have a backup plan-like a printed symptom log-if tech fails. And most importantly, check in regularly. A simple phone call saying, “How’s the monitoring going?” can make all the difference.






Comments
this is actually life changing for folks out here in the sticks. i got my dad on one of those smart pill dispensers last year after he nearly passed from warfarin messup. now he gets a call if he misses a dose. simple stuff, but it works. thanks for writing this.
Oh please. You’re glorifying tech like it’s some divine intervention. My cousin in West Virginia tried one of these ‘smart’ blood pressure cuffs-got a false reading because the battery was low, and the nurse ignored it for 3 days. Then he had a stroke. Tech doesn’t save lives. People do. And most rural clinics are too broke to even afford the damn devices.
Wow. So we’re supposed to be impressed that someone *finally* noticed that old people struggle with smartphones? Groundbreaking. I’m sure the 2023 FDA approval of AI that predicts side effects was also the first time anyone ever thought to… monitor patients? 🙄
In India too, many elders use medicine without monitoring. One cousin took blood pressure pill wrong and ended up in hospital. Simple app with voice reminder would help. No need fancy tech. Just clear voice. People understand sound better than screens.
The systemic failure here is not technological-it’s epistemological. You’re deploying siloed IoT modalities without integrating them into a holistic pharmacovigilance framework. The absence of real-time data harmonization across EHRs creates latent risk vectors that negate the purported efficacy of RPM. Also, reimbursement parity is a red herring; the real issue is the commodification of care under neoliberal health economics.
I read this entire thing and I’m just… stunned by how little anyone is talking about the emotional labor involved. The nurses, the pharmacists, the care coordinators-they’re not just pushing alerts. They’re holding space for people who haven’t been seen in years. Someone asks if you’re sleeping? That’s not a question-it’s a lifeline. And yet we treat this like a cost-center to optimize, not a human connection to protect. We’re building systems to catch side effects, but ignoring the side effects of isolation. That’s the real crisis. And no AI will ever fix that.
You people act like this is a miracle. Meanwhile, my uncle’s clinic got shut down because ‘telehealth was taking too many patients.’ So now he drives 90 miles for a 10-minute visit. And you’re patting yourselves on the back for sending a text reminder? 🤡
I’ve worked in rural clinics for 18 years. I’ve seen people die because they couldn’t get a ride. I’ve seen them skip doses because they were scared of the side effects and didn’t know who to ask. This post isn’t just about tools-it’s about dignity. The fact that someone in Montana can get a call from their pharmacist because their INR spiked? That’s not tech. That’s someone choosing to care. And that’s the thing we’ve lost in all this talk about efficiency and data. It’s not about how fast we respond. It’s about whether we show up at all. And for too long, we didn’t.