Angioedema is a sudden swelling of the deeper layers of skin and mucous membranes, often affecting the lips, eyes, throat, or genitals. It can appear without warning and may be triggered by foods, medications, stress, or hereditary factors. Understanding what fuels these episodes is the first step toward keeping them at bay.
Key Takeaways
- Identify and avoid personal triggers such as specific foods, medicines, and extreme temperatures.
- Adopt stress‑reduction habits like regular exercise, mindfulness, and adequate sleep.
- Stay hydrated and maintain a balanced diet rich in anti‑inflammatory foods.
- Know the prescription options: antihistamines, C1‑esterase inhibitor concentrates, and newer bradykinin blockers.
- Seek immediate medical help if swelling involves the throat or causes breathing difficulty.
Understanding Angioedema
There are two main categories: Hereditary Angioedema, a genetic condition caused by a deficiency of C1 Esterase Inhibitor, and acquired forms, which are usually linked to allergies, medications, or idiopathic causes.
In allergic cases, Histamine release drives the swelling, while in hereditary or ACE‑inhibitor‑induced attacks, the peptide bradykinin is the main culprit.
Common Triggers to Watch
Knowing your triggers lets you build a defense plan. Below is a quick reference:
| Trigger | Typical Management |
|---|---|
| Foods (nuts, shellfish, gluten) | Avoidance + antihistamine as needed |
| ACE Inhibitors (e.g., lisinopril) | Switch to alternative antihypertensive |
| NSAIDs (ibuprofen, naproxen) | Use acetaminophen; consider COX‑2 selective agents |
| Stress or anxiety | Mindfulness, regular exercise, adequate sleep |
| Cold exposure | Gradual temperature changes; protective clothing |

Lifestyle Changes That Reduce Risk
While medications are powerful, many people keep episodes at bay with daily habits.
- Mind Your Diet: Emphasize omega‑3 rich fish, leafy greens, and berries. These foods contain antioxidants that can dampen inflammatory pathways linked to swelling.
- Stay Hydrated: Dehydration can thicken plasma proteins, potentially worsening edema. Aim for at least 2 liters of water per day, more if you exercise heavily.
- Manage Stress: Chronic cortisol spikes can increase vascular permeability. Incorporate 10‑minute breathing exercises, yoga, or short walks after stressful tasks.
- Regular Physical Activity: Moderate aerobic exercise improves circulation and supports lymphatic drainage, which helps clear excess fluid.
- Avoid Known Medications: If you’ve reacted to NSAIDs or ACE Inhibitors, discuss alternatives with your doctor.
- Temperature Control: Sudden heat or cold can trigger swelling in some people. Use humidifiers in dry environments and dress in layers when moving between climates.
Medical Treatment Options
When lifestyle tweaks aren’t enough, targeted therapies step in.
- Antihistamines: First‑line for allergic angioedema. Non‑sedating options like cetirizine are preferred for daytime use.
- C1 Esterase Inhibitor Concentrates: For hereditary cases, products such as Berinert or Cinryze can be given intravenously or subcutaneously to restore the missing protein.
- Bradykinin Receptor Antagonists: Icatibant (Firazyr) blocks the B2 receptor, halting swelling quickly-especially useful for ACE‑inhibitor‑related attacks.
- Fresh‑Frozen Plasma: In emergency settings where specific inhibitors aren’t available, plasma can supply functional C1‑esterase temporarily.
- Short‑Course Corticosteroids: Helpful for severe, non‑histamine‑mediated swelling, but not ideal for long‑term use due to side effects.
Always keep a rescue kit (antihistamine tablets, epinephrine auto‑injector if you have anaphylaxis risk) and know how to use it.

When to Seek Immediate Care
Swelling that involves the throat, tongue, or vocal cords can obstruct the airway in minutes. If you notice:
- Difficulty swallowing or speaking
- Stridor (high‑pitched breathing sound)
- Rapidly expanding neck or lip swelling
- Feeling light‑headed or dizzy
Call emergency services right away. Even if you have a known trigger, airway compromise is a medical emergency.
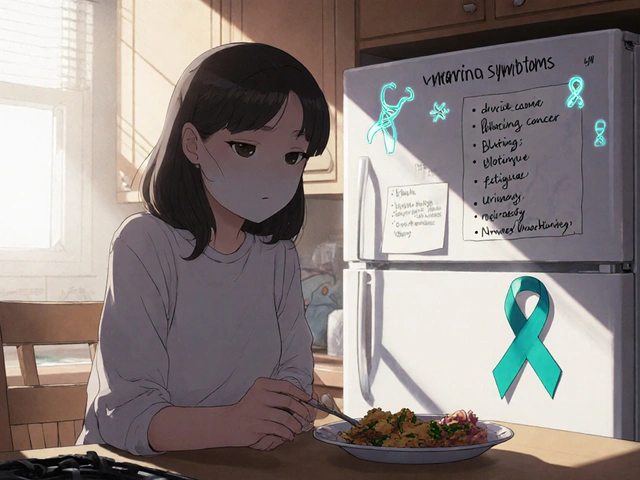
Creating Your Personal Action Plan
Write down a simple checklist you can keep on the fridge or in your phone.
- List known triggers and alternatives.
- Keep an up‑to‑date medication list (including over‑the‑counter drugs).
- Store rescue medication where you’ll see it.
- Schedule routine follow‑ups with a specialist-preferably an allergist or immunologist.
- Review the plan with family or coworkers so they can help if an episode occurs.
Review this plan every six months or after any new reaction.
Frequently Asked Questions
Can stress really cause angioedema?
Yes. Stress releases hormones that increase capillary permeability, making swelling more likely in people with a predisposition.
Are there any foods that universally trigger angioedema?
No single food affects everyone, but common culprits include nuts, shellfish, and certain fruits like strawberries. An elimination diet under a dietitian’s guidance helps pinpoint personal triggers.
What’s the difference between antihistamines and C1‑esterase inhibitor therapy?
Antihistamines block the effects of histamine, useful for allergy‑related swelling. C1‑esterase inhibitors replace a missing protein in hereditary angioedema and work on a completely different pathway involving bradykinin.
Should I stop taking NSAIDs if I’ve never had an episode?
If you have no history of reactions, you don’t need to stop abruptly, but be aware that NSAIDs are a known trigger for some people. Discuss alternatives with your physician if you’re concerned.
Is there a cure for hereditary angioedema?
Current treatments can control attacks and improve quality of life, but they don’t eliminate the genetic deficiency. Ongoing research into gene therapy shows promise for the future.
By blending vigilant trigger avoidance, healthy daily habits, and appropriate medical therapy, most people can keep angioedema episodes rare and mild. Stay informed, stay prepared, and don’t hesitate to reach out to a healthcare professional when in doubt.







Comments
If you think staying hydrated alone prevents angioedema, you’re missing the mechanistic reality; without addressing bradykinin pathways, water won’t stop an attack.
They don’t tell you that big pharma hides the true cure for angioedema behind expensive biologics, while pushing cheap antihistamines that barely scratch the surface.
Our country’s medical system should prioritize rapid access to C1‑esterase inhibitors –‑ no one should wait days for life‑saving meds because of bureaucratic red tape.
Actually, the real bottleneck isn’t the system but patient education; many ignore trigger avoidance, assuming medication alone will save them, which fuels unnecessary ER visits.
Oh great, another list of “lifestyle tips” that sound like a wellness blog, as if a two‑minute meditation can stop a throat‑closing swelling.
Hydration and balanced diet help, but keep a rescue kit handy.
Honestly, the whole “bradykinin blocker” hype is just pharma’s way to rebrand old peptides; the underlying inflammatory cascade stays the same and they sell you another pricey injection.
Sure, Jake, because the only thing missing from your “concise” critique is a citation-maybe a peer‑reviewed study showing plasma levels correlate with water intake.
Life is a series of swellings, both literal and metaphorical; recognizing the pattern is the first step to mastering the unknown.
Managing angioedema starts with a clear understanding of your specific subtype.
If you have hereditary angioedema, C1‑esterase inhibitor replacement is the cornerstone of therapy.
For acquired forms, identifying whether histamine or bradykinin drives the swelling guides drug choice.
Antihistamines are inexpensive and work quickly for histamine‑mediated episodes.
However, they have little effect on bradykinin‑driven attacks, which require targeted agents like icatibant.
Keep a written log of any swelling events, noting the time of day, foods eaten, medications taken, and stress levels.
This log becomes invaluable when you discuss patterns with your allergist or immunologist.
In addition to prescription meds, a daily regimen rich in omega‑3 fatty acids, antioxidants, and adequate protein supports vascular stability.
Avoiding known triggers such as ACE inhibitors, NSAIDs, and extreme temperature swings can reduce baseline risk.
Regular moderate exercise promotes lymphatic drainage, but always have your rescue kit on hand during workouts.
If you ever experience throat involvement, call emergency services immediately; airway compromise can progress in minutes.
For patients on home infusions, a pre‑filled emergency kit containing C1‑esterase inhibitor concentrate can be life‑saving.
Discuss the possibility of prophylactic subcutaneous therapy with your physician if attacks occur more than twice a month.
Finally, educate family members and coworkers on how to administer emergency medication, because timely help matters.
By combining precise medical treatment with diligent lifestyle habits, you can keep angioedema episodes infrequent and manageable.
Congrats on discovering water-you’ve unlocked the secret to everything.
I appreciate your thorough breakdown, Casey; the emphasis on systematic logging really resonates with best practices.
lol, water is magic but only if you remember to breathe 🌊