Statin-Antifungal Interaction Checker
Check Your Medication Combination
Results
Select your medications to see the interaction risk level.
Imagine you’re on a statin to lower your cholesterol, and then you get a stubborn fungal infection that needs a strong antifungal pill. Sounds simple, right? But here’s the catch: mixing certain antifungals with statins can turn a routine treatment into a life-threatening situation. This isn’t theoretical. People end up in the hospital every year because of this exact combo. And it’s not just statins-immunosuppressants like cyclosporine or tacrolimus, often taken by transplant patients, can make things even worse.
Why This Interaction Is So Dangerous
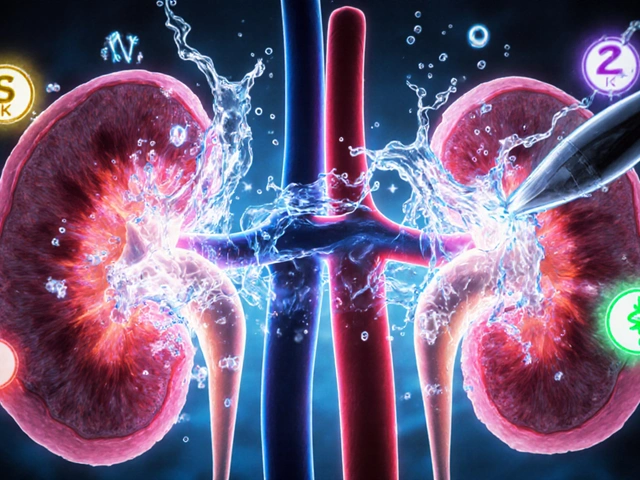
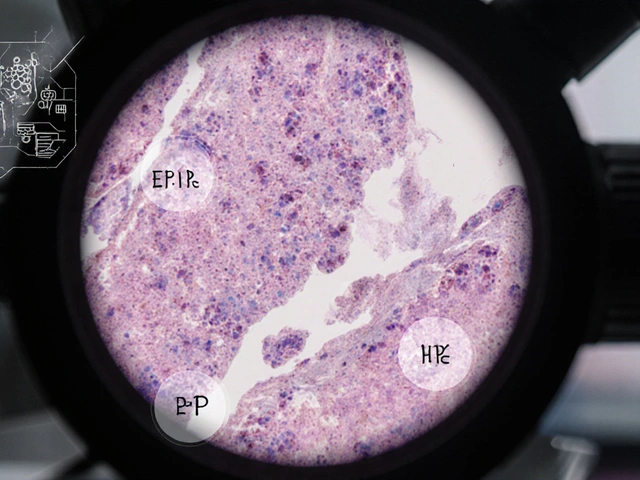
The problem starts with your liver. It uses a group of enzymes called cytochrome P450 to break down drugs so your body can get rid of them. One of the most important of these is CYP3A4. It handles about 30% of all medications you take, including most statins and many immunosuppressants. Now, enter the azole antifungals-drugs like ketoconazole, itraconazole, voriconazole, and posaconazole. These antifungals don’t just kill fungi. They also slam the brakes on CYP3A4. When that happens, your statin doesn’t get cleared from your body like it should. Instead, it builds up to dangerous levels.That buildup doesn’t just mean higher cholesterol control. It means muscle damage. Statins are already linked to muscle pain and weakness in about 5-10% of users. But when you add a strong CYP3A4 inhibitor like ketoconazole or posaconazole, that risk jumps tenfold. In extreme cases, this leads to rhabdomyolysis-a condition where muscle tissue breaks down so badly that it floods your bloodstream with proteins that can shut down your kidneys. Creatine kinase (CK) levels can spike past 10,000 U/L. Normal is under 200. This isn’t rare. It’s documented in case reports across hospitals in the U.S., Europe, and Australia.
Which Statins Are Most at Risk?
Not all statins are created equal. Some are like gasoline near a spark. Others are much safer.- High risk: Simvastatin, lovastatin, atorvastatin. These are broken down almost entirely by CYP3A4. Taking them with ketoconazole or posaconazole can raise their levels by 10 to 20 times. Simvastatin is especially dangerous-some guidelines say it should never be used with even moderate CYP3A4 inhibitors.
- Moderate risk: Fluvastatin and pitavastatin. These use other pathways, so they’re less affected, but still not risk-free.
- Lower risk: Pravastatin and rosuvastatin. These are mostly cleared by the kidneys or through non-CYP pathways. But here’s the twist: ketoconazole can still raise pravastatin levels by blocking the OATP1B1 transporter in your liver. So even these "safer" options need caution.
Bottom line: If you’re on simvastatin or lovastatin and need an azole antifungal, you should stop the statin during treatment. Period. Atorvastatin can sometimes be switched to rosuvastatin as a temporary replacement. But never try to "just lower the dose" and hope for the best. That’s how people end up in intensive care.
Immunosuppressants Make It Worse
If you’ve had a kidney, liver, or heart transplant, you’re probably on cyclosporine, tacrolimus, or sirolimus. These drugs don’t just suppress your immune system-they also block CYP3A4 and P-glycoprotein, just like azole antifungals. So when you add an antifungal to the mix, you’re stacking two powerful inhibitors on top of a statin. The result? Statin levels can jump 3 to 20 times higher than normal.Studies show that up to 25% of transplant patients on statins develop muscle symptoms when they’re also on cyclosporine. And if they get an azole antifungal on top of that? The risk of rhabdomyolysis increases dramatically. One study found that CK levels in these patients often rose above 5,000 U/L within days of starting fluconazole or itraconazole. That’s not a coincidence. It’s a predictable outcome of the chemistry.
Doctors often miss this because transplant patients are already being monitored closely for kidney function and drug levels. But muscle damage doesn’t show up on routine blood tests unless CK is checked. And many clinics don’t routinely check CK unless the patient complains of pain. That’s a dangerous gap.
What to Do If You Need an Antifungal
If you’re on a statin and your doctor prescribes an azole antifungal, here’s what you need to know:- Stop simvastatin and lovastatin immediately. Don’t wait. Don’t try to cut the dose. Just stop. Restart only after the antifungal is completely out of your system-which can take days or even weeks with posaconazole, thanks to its long half-life.
- Switch to pravastatin or rosuvastatin. If you need ongoing cholesterol control, these are your safest bets. Use the lowest effective dose: 10 mg of pravastatin or 5 mg of rosuvastatin daily. Even then, watch for muscle pain.
- Ask about fluconazole. Among azoles, fluconazole is the weakest CYP3A4 inhibitor. It’s still not risk-free, but it’s safer than ketoconazole or posaconazole. For mild fungal infections like oral thrush or vaginal yeast, fluconazole is often enough.
- Get your CK checked. If you start feeling unexplained muscle soreness, weakness, or dark urine, get a blood test for creatine kinase. Don’t wait. Rhabdomyolysis can progress fast.
- Don’t rely on memory. Write down every medication you take-prescription, over-the-counter, supplements. Bring it to every appointment. Many interactions happen because patients forget to mention a topical antifungal cream or a friend’s leftover antifungal pill.
What’s New and What’s Coming
There’s some good news. Newer antifungals are being designed to avoid these interactions. Isavuconazole, approved in 2015, is a moderate CYP3A4 inhibitor-less risky than ketoconazole. And olorofim, currently in phase 3 trials, works by a completely different mechanism. It doesn’t touch CYP enzymes at all. That could be a game-changer for transplant patients who need long-term antifungal therapy.Pharmacists are also stepping up. In 87% of academic medical centers in the U.S., pharmacists now review every azole prescription against a patient’s statin list before dispensing. That’s cut high-risk combinations by 63%. But in community pharmacies and rural clinics, that safety net isn’t always there.
Genetics might also play a role. About 12% of people carry a gene variant called SLCO1B1 that makes their liver less able to take up statins. If you have this variant and take a statin with an azole, your risk of muscle damage is even higher. Genetic testing isn’t routine yet, but it’s becoming more accessible. If you’ve had muscle problems with statins before, ask your doctor about testing.
Real-World Reality
Despite decades of warnings, these dangerous combinations are still being prescribed. A 2012 study found that nearly 1 in 5 patients on statins were also getting a CYP3A4 inhibitor-antifungals included. And that was over a decade ago. Today, fluconazole alone is prescribed over 5 million times a year in the U.S. Many of those patients are also on statins. Electronic health records now have alerts, but they’re often ignored. Why? Because doctors are rushed. Because patients don’t know to ask. Because the risk feels distant until it’s too late.This isn’t about blaming anyone. It’s about awareness. You don’t need to be a doctor to understand this: systemic antifungals and statins don’t play well together. If you’re on either, and you’re prescribed the other, pause. Ask. Double-check. Bring your list of meds. Ask if there’s a safer alternative. Your muscles-and your kidneys-will thank you.
What About Over-the-Counter Antifungals?
Topical creams, sprays, and shampoos (like clotrimazole or terbinafine) are generally safe. They don’t get into your bloodstream enough to cause interactions. But oral antifungals-even ones sold without a prescription in some countries-are a different story. If it’s a pill you swallow, assume it can interact. Always check with your pharmacist or doctor.When to Seek Help Immediately
If you’re taking a systemic antifungal and a statin, watch for these red flags:- Unexplained muscle pain, tenderness, or weakness, especially in the thighs or shoulders
- Dark, tea-colored urine
- Fatigue beyond normal
- Nausea or vomiting with muscle symptoms
Call your doctor or go to urgent care. Don’t wait until morning. Rhabdomyolysis can cause kidney failure within hours.
Can I take fluconazole with my statin?
Fluconazole is a weaker inhibitor of CYP3A4 than other azoles, so it’s often safer. But it still increases statin levels. If you’re on simvastatin or lovastatin, avoid fluconazole entirely. For atorvastatin, use the lowest dose and monitor for muscle pain. Pravastatin or rosuvastatin are better choices. Always check with your pharmacist before combining them.
How long should I wait after stopping an antifungal before restarting my statin?
It depends on the antifungal. For fluconazole, wait 2-3 days. For itraconazole or voriconazole, wait 5-7 days. But for posaconazole, wait at least 10-14 days-it stays in your system much longer. Never restart your statin without checking with your doctor. Even if you feel fine, the drug can still be lingering in your liver.
Are there statins that are completely safe with antifungals?
No statin is 100% safe with all antifungals. But pravastatin and rosuvastatin are the safest options because they don’t rely heavily on CYP3A4. Even then, ketoconazole can still raise their levels by blocking the OATP1B1 transporter. So while they’re your best bet, they still need caution-especially at higher doses.
Can I take a natural antifungal instead, like garlic or oregano oil?
Natural doesn’t mean safe. Garlic and oregano oil can also inhibit CYP3A4 and interfere with statins. There’s no clinical proof they work as well as prescription antifungals for systemic infections. If you have a serious fungal infection, you need a proven treatment. Don’t risk your health with unregulated supplements.
Why don’t doctors catch this more often?
Many doctors aren’t aware of the full scope of the interaction, especially if they’re not specialists. Patients often don’t mention all their meds. Electronic alerts exist but can be overridden. And with statins and antifungals both being so common, the risk gets overlooked. That’s why it’s critical for you to speak up-bring your full med list, ask questions, and don’t assume your doctor knows every interaction.







Comments
This is why people die from simple prescriptions. You take a statin like it's candy, then some doctor throws ketoconazole at you like it's a lollipop-and boom, your muscles turn to mush. No one tells you this stuff until you're in the ICU with CK levels higher than your Netflix binge count. I've seen it. I've nursed people through it. And no, lowering the dose doesn't work. You don't get to cheat biochemistry. Stop being lazy and read the damn label.
I appreciate how thorough this is. I’m a transplant recipient on tacrolimus and rosuvastatin, and I’ve been terrified to even take a fluconazole for a yeast infection. I’m glad someone laid out the risks clearly-especially the part about OATP1B1. I’ll definitely ask my pharmacist next time. Thanks for not just scaring people, but giving real alternatives.
OMG I KNEW THIS WAS A TRAP!! My uncle died from this!! He was on simva and got posaconazole for aspergillosis and then POOF!! Muscles gone!! Kidneys gone!! He was 58!! WHY DO DOCTORS STILL DO THIS!! I SWEAR IF I SEE ONE MORE PRESCRIPTION FOR SIMVASTATIN WITH AN AZOLE I'M GOING TO THE NEWS!!
Y’all are acting like this is new info. I’ve been screaming about this since 2019 when I had to go off atorvastatin for a fungal nail thing. My legs felt like lead for a week. My doc didn’t even blink. I had to pull up the FDA warning myself. Like… why is this still a thing? We have alerts in EHRs. Why are people still getting this combo? Someone’s not doing their job.
Great breakdown. I work in a community pharmacy, and we’ve started flagging every azole prescription against statin lists since last year. It’s cut our near-misses by over half. But honestly? The biggest issue isn’t the tech-it’s the patients who don’t tell us about their OTC supplements or that ‘natural antifungal’ cream they’ve been using for months. We need better patient education, not just alerts.
This is one of those topics where the science is crystal clear, but the human system keeps failing. I’ve had patients come in saying, ‘My cousin took this and was fine.’ But biology doesn’t care about cousins. It cares about enzymes. I’m glad someone spelled it out so plainly. I’ll be sharing this with my elderly patients who are on multiple meds.
In India we see this often. Elderly patients take statins for years and then get antifungal pills from local pharmacies without prescription. No lab tests. No monitoring. Many end up with kidney failure. We need public health campaigns. Not just for doctors but for the people who buy medicine off the street. Awareness saves lives.
The fact that this interaction remains under-recognized in primary care is a systemic failure. The pharmacokinetics are well-documented in peer-reviewed literature since the early 2000s. Yet, in community settings, clinicians still default to prescribing simvastatin with fluconazole because it’s ‘convenient.’ We need mandatory CYP3A4 interaction training for all prescribers-not just pharmacists. This isn’t niche knowledge. It’s standard.
Oh wow, another ‘warning’ article. So… we’re supposed to believe that every single drug interaction is a death sentence? What about all the people who take these combos and never have an issue? Maybe your fear is just masking your lack of trust in the body’s ability to adapt? Also, ‘natural’ antifungals aren’t dangerous because they’re ‘unregulated’-they’re dangerous because you’re too lazy to let your immune system do its job. Let your body heal. Stop poisoning it with statins and azoles.
Let me tell you what happened to my neighbor. She was on simvastatin for 8 years. Got a yeast infection. Took itraconazole for 10 days. Woke up one morning and couldn’t lift her coffee cup. Thought it was ‘just tired.’ Went to the ER three days later. CK was 28,000. Kidneys shut down. Dialysis for a month. Now she walks with a cane. And the doctor? Said, ‘We didn’t think it would happen to her.’ That’s not medicine. That’s Russian roulette with a prescription pad. I’m not even mad anymore. I’m just… numb.
This is why America's healthcare system is broken. You have a 10-page article explaining something that should be taught in med school orientation. And yet, doctors still mess this up. Why? Because they're overworked. Because they're paid to prescribe, not to think. And because patients don't read the fine print. We need mandatory CYP450 certification for every prescriber. Or better yet-ban simvastatin outright. It's a relic.
In South Africa, we face a different challenge: access. Many patients cannot afford to switch from simvastatin to rosuvastatin. The cost difference is 10x. So they take the cheaper statin and the antifungal anyway. And when they get sick? They go to a clinic with no CK testing. This is not just a pharmacological issue-it is a social justice issue. We need generic, affordable, safe alternatives. And we need them yesterday.
Thank you for including the part about OATP1B1. Most resources stop at CYP3A4, but the transporter inhibition is just as critical-especially for pravastatin and rosuvastatin. I’m a clinical pharmacist in Canada, and we’ve updated our institutional guidelines to include this nuance. It’s a small but vital detail that can prevent harm. I wish more providers knew this.