Triple-Negative Breast Cancer Explained: Causes, Signs & Treatment Options
Learn what causes triple‑negative breast cancer, how to spot its symptoms, and the latest treatment options-from chemo to immunotherapy and PARP inhibitors.
Read moreWhen talking about breast cancer subtypes, the distinct categories of breast cancer classified by molecular and pathological features. Also known as BC subtypes, it helps doctors predict how the disease will behave and which therapies are likely to work.
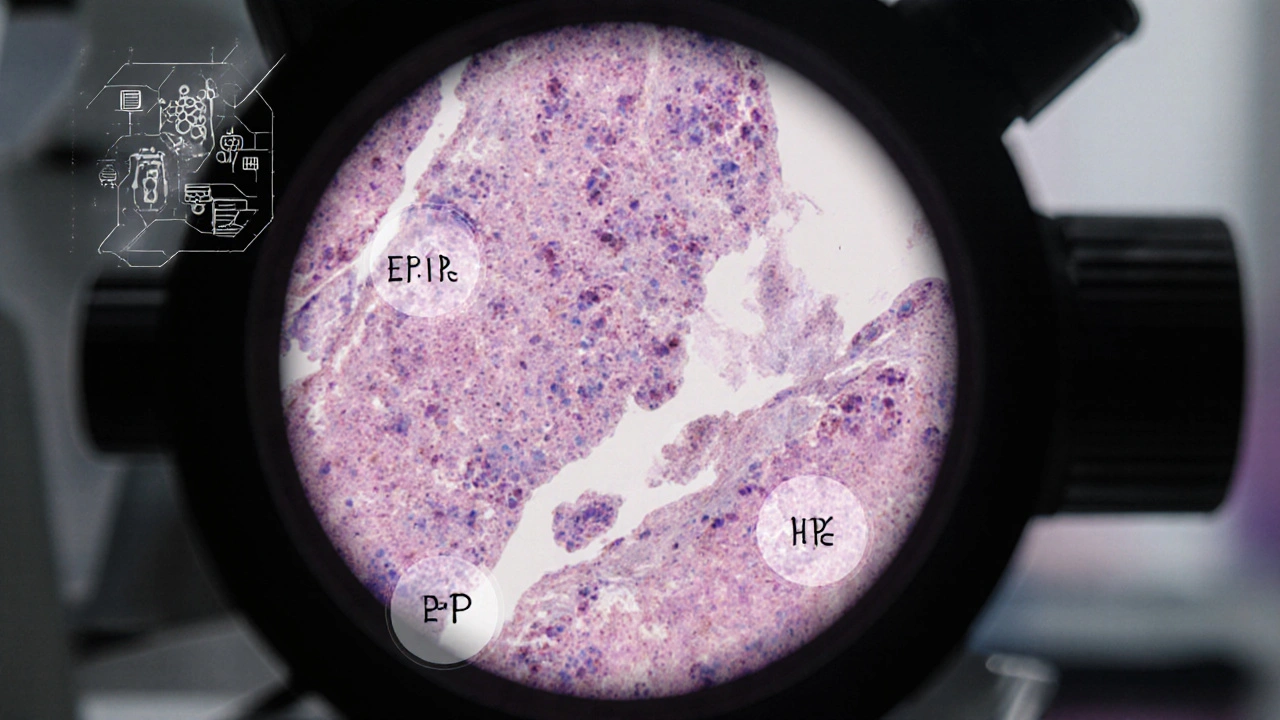
One of the first things you’ll hear is hormone receptor status, whether cancer cells have estrogen (ER) or progesterone (PR) receptors. Tumors that are ER‑positive or PR‑positive usually respond to endocrine treatments, which can lower recurrence risk. Breast cancer subtypes are built around this marker because it directly shapes the treatment plan.
Another pivotal marker is HER2, a protein that drives rapid tumor growth when overexpressed. HER2‑positive cancers often need targeted drugs like trastuzumab, and knowing the HER2 status can mean the difference between a standard chemotherapy regimen and a more effective, less toxic approach.
When a tumor lacks ER, PR, and HER2, it falls into the triple‑negative breast cancer, a form that typically grows faster and has fewer targeted options. Patients with this subtype may be eligible for immunotherapy or clinical trials, making early identification crucial for accessing those options.
Genetic factors also play a big role. Mutations in BRCA genes, DNA repair genes whose loss raises breast cancer risk can predispose someone to specific subtypes, especially triple‑negative disease. Testing for BRCA mutations isn’t just about risk assessment; it can guide the use of PARP inhibitors, a class of drugs that work particularly well in BRCA‑mutated tumors.
Understanding the subtype landscape enables patients to ask the right questions at the doctor’s office. It also lets clinicians match a tumor’s biology with the most appropriate therapy, reducing unnecessary side effects. For researchers, categorizing cancers by subtype fuels the development of new drugs that target the exact pathways driving each form.
The practical side of subtype classification shows up in everyday decisions. For example, a patient with a Luminal A tumor—a subtype defined by strong hormone‑receptor positivity and low proliferation—might safely skip chemotherapy and rely on hormonal therapy alone. Meanwhile, a Luminal B tumor, which shares hormone‑receptor positivity but has higher proliferation, often benefits from a combined chemo‑hormonal approach.
Beyond treatment, subtypes influence follow‑up schedules. HER2‑positive patients typically undergo more frequent imaging in the first two years after treatment because the risk of early recurrence is higher. Triple‑negative patients, on the other hand, may need closer monitoring for distant metastasis, as this subtype tends to spread beyond the breast earlier.
So, whether you’re a patient navigating your care plan, a caregiver supporting a loved one, or a health professional staying current, knowing the details of breast cancer subtypes equips you with the context needed to make informed choices.
Below you’ll find a curated collection of articles that dive deeper into nutrition tips for muscle health, comparisons of various medications, and other health topics that intersect with cancer care. These pieces provide practical guidance and up‑to‑date information to help you apply what you’ve learned about breast cancer subtypes to real‑world situations.
Learn what causes triple‑negative breast cancer, how to spot its symptoms, and the latest treatment options-from chemo to immunotherapy and PARP inhibitors.
Read more