Heart disease kills more women every year than breast cancer, stroke, and lung cancer combined. Yet, most women still don’t see it as their biggest health threat. In the U.S., about 1 in 5 female deaths is caused by heart disease - and many of those deaths could have been prevented. The problem isn’t just lack of awareness. It’s that women’s heart attacks don’t look like the ones you see in movies. No dramatic clutching of the chest. No collapsing on the sidewalk. Instead, symptoms are quieter, weirder, and easier to ignore - until it’s too late.
What Heart Disease Looks Like in Women
When men have a heart attack, they often feel a crushing pain in the center of their chest. That’s the classic image. But for women, that’s only part of the story. About 65% of women experience chest discomfort during a heart attack - meaning nearly 4 in 10 don’t feel it at all. Instead, they get symptoms that seem unrelated: sudden exhaustion, nausea, jaw pain, or shortness of breath while walking to the mailbox. A 2023 study from the National Heart, Lung, and Blood Institute found that women are more likely than men to report:- Unexplained fatigue - so bad it stops you from making your bed or taking the stairs (71% of women who had heart attacks reported this)
- Shortness of breath - even when resting
- Pain in the back, neck, jaw, or one or both arms
- Nausea, vomiting, or indigestion
- Dizziness or sudden lightheadedness
Why Women’s Hearts Are Different
Women’s hearts aren’t just smaller versions of men’s. They’re built differently. Arteries are narrower. Hormones like estrogen play a protective role - until menopause. After that, the risk jumps sharply. And then there are conditions that mostly affect women:- Microvascular disease: This affects the tiny arteries in the heart, not the big ones. It doesn’t show up on standard tests. Symptoms? Constant fatigue, breathlessness, and chest tightness - especially under stress.
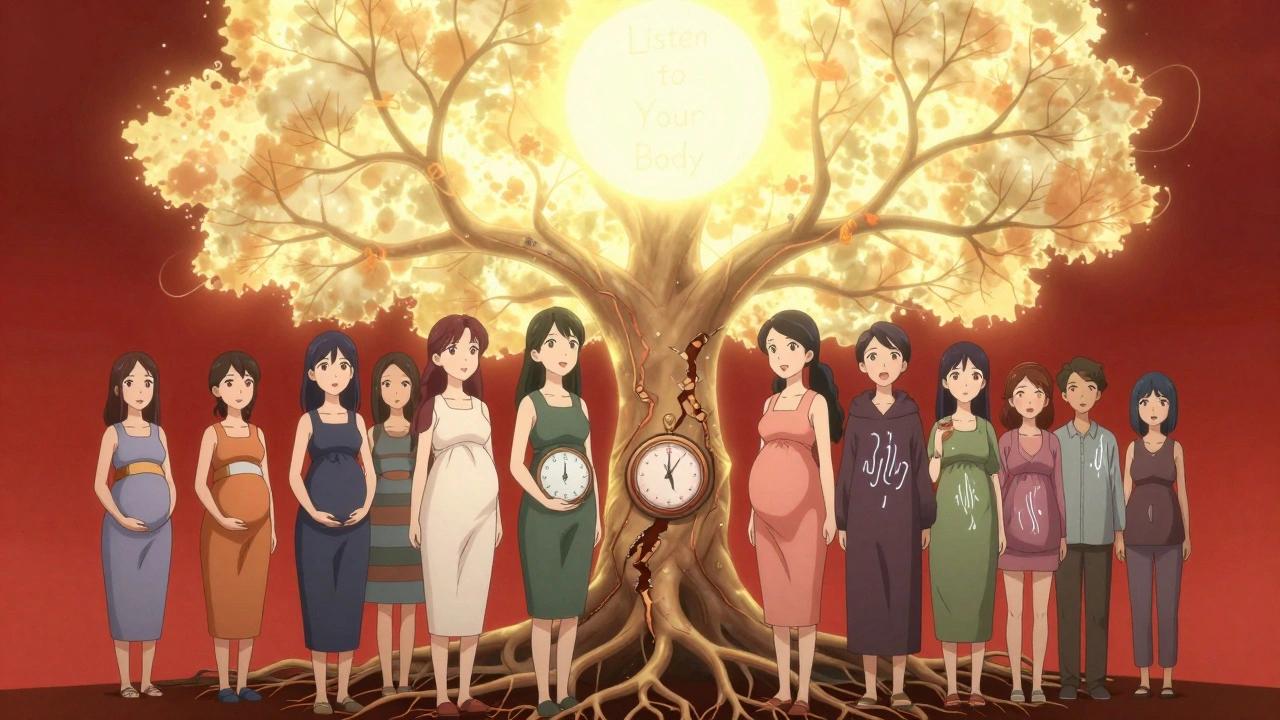
- SCAD (Spontaneous Coronary Artery Dissection): A tear in a heart artery with no warning. It happens mostly in women under 50, often during pregnancy or after childbirth. It’s rare, but it’s the leading cause of heart attacks in younger women.
- Takotsubo syndrome (broken heart syndrome): Triggered by extreme emotional stress - like losing a loved one or a sudden divorce. The heart muscle temporarily weakens, mimicking a heart attack. It’s almost always reversible, but it can be deadly if not treated.
The Diagnosis Gap
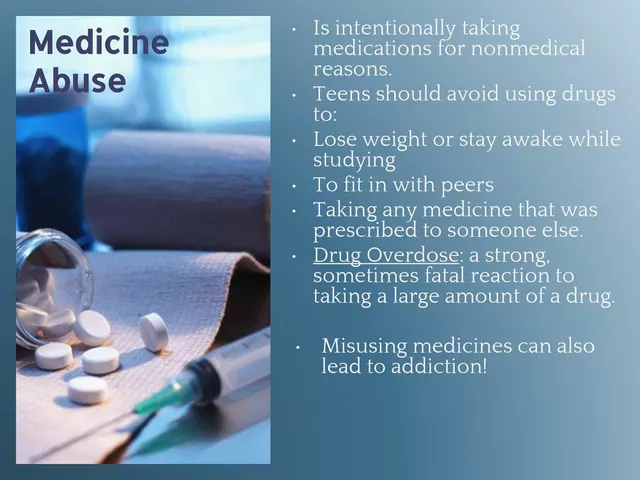
Here’s the scary part: women under 55 are seven times more likely than men to be sent home from the ER with the wrong diagnosis. A 2021 study in the Journal of the American Heart Association found that women with heart attacks are frequently told they’re having anxiety, indigestion, or a panic attack. One woman in her 40s was sent home three times before she finally had a heart attack that couldn’t be ignored. By then, her heart was severely damaged. Why does this happen? Bias. A 2022 study in JAMA Internal Medicine found that 68% of emergency room doctors attributed women’s cardiac symptoms to psychological causes - even when their ECGs showed clear signs of trouble. Women are more likely to be told, "You’re just stressed," or "You’re too young for this." And it’s not just the ER. Standard tests like stress tests and angiograms were developed using mostly male data. They’re less accurate for women. That’s why the FDA approved the Corus CAD test in 2020 - a blood test that looks at gene patterns to detect heart disease in women with 88% accuracy. It’s not widely used yet, but it’s a step in the right direction.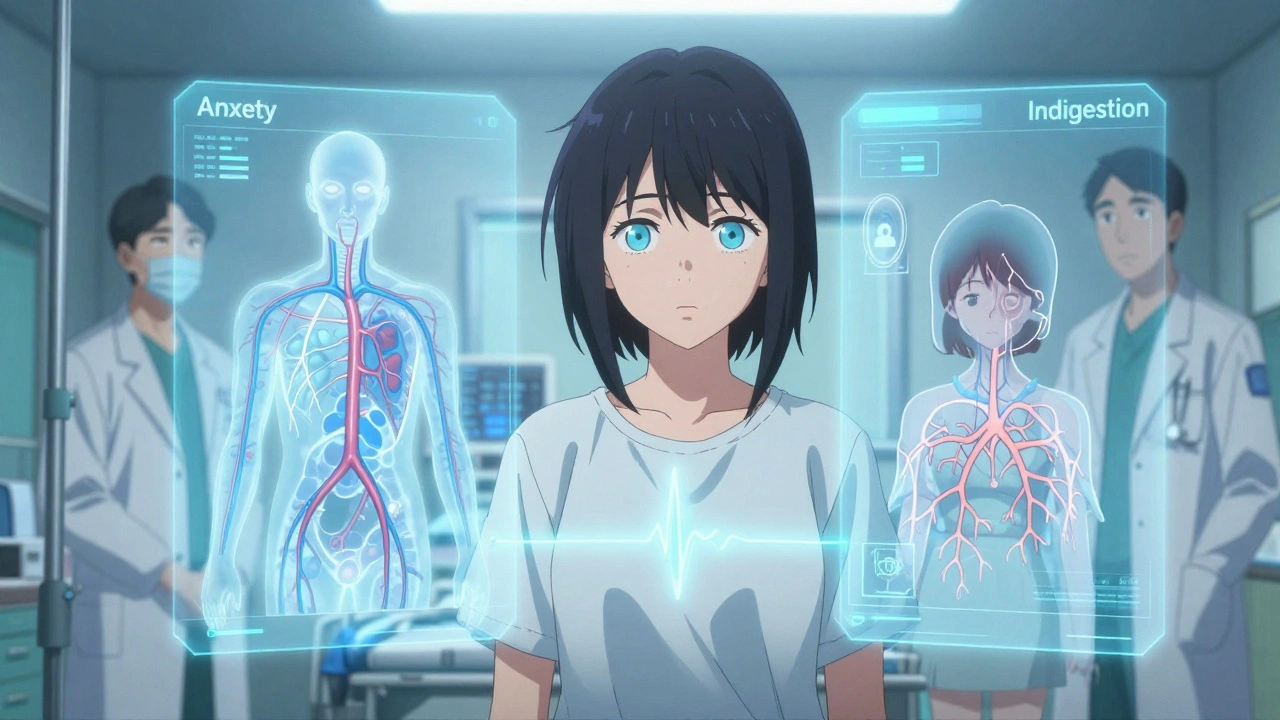
Risk Factors Women Can’t Ignore
Some risks are the same for men and women: smoking, high blood pressure, obesity, diabetes. But women have unique ones:- Pregnancy complications: Preeclampsia (high blood pressure during pregnancy) increases future heart disease risk by 80%. Gestational diabetes doubles it.
- Early menopause: Menopause before age 45 raises heart disease risk by 50%.
- Autoimmune diseases: Lupus and rheumatoid arthritis are more common in women and damage blood vessels over time.
- Chronic stress: Women are twice as likely as men to have angina triggered by mental stress - not just physical exertion.
- Silent heart attacks: Women over 65 are 34% more likely than men to have a heart attack with no symptoms at all. They just feel "off" - and never connect it to their heart.
What to Do - Before It’s Too Late
You can’t change your gender or your hormones. But you can change how you respond to your body’s signals.- Track your energy: If you’re constantly exhausted - not just tired from a busy day, but bone-deep worn out - and it lasts more than two weeks, get checked. That’s one of the top warning signs.
- Don’t dismiss unusual pain: Jaw pain that comes and goes. Back pain that doesn’t improve with massage. Nausea that shows up with stress. These aren’t "just a bad day."
- Know your numbers: Blood pressure, cholesterol, and blood sugar matter more for women than you think. Get them checked yearly after 40. If you’re overweight or have a family history, start earlier.
- Ask for the right tests: If you have symptoms but a normal ECG, ask about a coronary calcium scan or the Corus CAD test. Don’t take "nothing’s wrong" as the final answer.
- Find a women’s heart specialist: Hospitals with Women’s Cardiovascular Centers of Excellence have 25% fewer diagnostic delays for women. If you’re in Australia, ask your GP for a referral to a cardiologist who specializes in women’s heart health.
What Works - Real Results
The American Heart Association’s "Go Red for Women" campaign has helped. Since 2004, women’s ability to recognize heart attack symptoms has increased by 27%. But we’re still far from where we need to be. Only 44% of women know heart disease is their top killer - and that number hasn’t budged much since 2019. The good news? Women who get treated at specialized heart centers have a 22% higher chance of surviving a heart attack. That’s huge. It means the right care makes all the difference. And prevention? It works. Quitting smoking cuts your heart disease risk by half in just one year. Walking 30 minutes a day lowers blood pressure and improves circulation. Managing stress through yoga, meditation, or even just talking to a friend reduces your risk more than you think.Final Thought: Your Body Is Talking
Heart disease in women isn’t a mystery. It’s a mismatch - between how we expect symptoms to look, and how they actually appear. The science is clear. The tools exist. The problem is silence - from women who don’t speak up, and from doctors who don’t listen. If you feel something’s off - even if you can’t explain it - trust that feeling. Write down your symptoms. Note when they happen. Bring them to your doctor. Don’t wait for chest pain. Don’t wait for a crisis. Your heart doesn’t care if you’re "too young" or "too healthy." It only cares if you listen.Do women have heart attacks without chest pain?
Yes. About 43% of women who have heart attacks don’t feel chest pain at all. Instead, they experience extreme fatigue, shortness of breath, nausea, jaw or back pain, or dizziness. These symptoms are often mistaken for the flu, stress, or aging - but they’re warning signs of a heart attack.
Is heart disease more dangerous for women than men?
Yes, in several ways. Women are more likely to die within a year after their first heart attack. They’re also more likely to have complications like heart failure or stroke afterward. Their symptoms are often missed, leading to delayed treatment. And when they do get treated, they’re more likely to have damage to the small arteries - which are harder to fix.
What are the most overlooked symptoms of heart disease in women?
The most overlooked symptoms are unexplained fatigue, nausea, jaw or back pain, and shortness of breath during normal activities. Many women think these are signs of stress, poor sleep, or getting older. But when they happen together - especially if they’re new or worsening - they’re strong indicators of heart trouble.
Can pregnancy affect a woman’s heart health later in life?
Absolutely. Complications like preeclampsia, gestational diabetes, or delivering a baby prematurely increase a woman’s future risk of heart disease by 50-80%. These are not just pregnancy issues - they’re early warning signs. Women who’ve had these complications should get regular heart screenings starting in their 30s or 40s.
Are standard heart tests accurate for women?
Not always. Traditional stress tests and angiograms were designed using mostly male data. They can miss microvascular disease - the most common form of heart disease in women. Newer tools like the Corus CAD blood test and coronary calcium scans are more accurate for women. If you have symptoms but normal test results, ask your doctor about these alternatives.
How can I reduce my risk of heart disease after menopause?
After menopause, estrogen drops, and heart risk rises. To protect yourself: maintain a healthy weight, exercise 150 minutes a week, avoid smoking, manage blood pressure and cholesterol, and limit alcohol. Talk to your doctor about whether hormone therapy is right for you - it’s not for everyone, but it can help some women if started early after menopause.







Comments
Heart disease isn't some abstract threat-it's the quiet killer that outsmarts us because we're trained to look for drama. We want cinematic collapses, not a woman who just can't get out of bed for three days. We romanticize suffering, but real danger is mundane. It's in the silence. And we're too busy scrolling to hear it.
Okay but let’s be real-this isn’t just about medicine, it’s about patriarchal medical infrastructure. The entire diagnostic framework was built on male bodies like they’re the default human. Microvascular disease? SCAD? Takotsubo? These aren’t ‘female variants’-they’re legitimate, physiological phenomena that were ignored because ‘men are the norm.’ It’s medical colonialism wrapped in stethoscopes. And now we’re expected to be grateful for a blood test that *finally* acknowledges we’re not just men with smaller chests? 🤡
I’ve had this weird fatigue for months. My doctor said it was ‘burnout.’ I didn’t say anything. Now I’m scared to bring it up again. What if I’m just weak? What if I’m overreacting? I don’t want to be that girl who cries wolf… but what if I’m already too late?
Listen. I’ve been a nurse for 22 years. I’ve seen women sent home with indigestion while their hearts were failing. I’ve held their hands as they coded in the ER three days later. This isn’t theoretical. It’s personal. If you feel off, write it down. Bring it in. Say it again. And if they dismiss you? Find another doctor. Your life is worth more than their bias. I’ve seen it save lives. You can too.
bro why are we even talking about this like its a mystery? women just complain too much. i had a cousin who said she had chest pain and it was just anxiety. now she's fine. stop making everything a crisis. also why are we blaming doctors? maybe women are just dramatizing normal stuff. 😴
Hey, you're not alone. I had the same thing-fatigue, jaw pain, thought it was just stress. Went to three doctors before one actually listened. Got the Corus CAD test. Turned out I had microvascular disease. I'm alive today because I kept pushing. You got this. 💪 And if your doc doesn't get it, find one who does. There are specialists out there. You deserve care that sees you.
USA has the best medicine in the world. If you're having symptoms, go to the ER. End of story. If you're not getting help, you're not trying hard enough. This isn't a gender thing-it's a 'you didn't scream loud enough' thing. Also, why are we letting feminists turn heart disease into a political issue? Just take your vitamins and stop whining. 🇺🇸
obviously this is all a big pharma scam to sell more tests. the real cause? 5g radiation + glyphosate in your kale smoothie. doctors dont know sh*t. theyre just puppets. and why is the article talking about a 'corus cad test'? sounds like a NSA surveillance program. they want to track your heartbeats. wake up sheeple. 🌍👁️
Thank you for sharing this information with such clarity. I believe that early detection and proactive care are not just medical choices-they are acts of self-respect. Every woman deserves to be heard, to be believed, and to have access to tools that recognize her body's unique language. Please, if you are reading this, take one step today. Write down your symptoms. Call your doctor. Your heart is not asking for permission to speak.
Just had my first coronary calcium scan after my doc finally listened (thank god). Score was 187-high risk. Scared the crap outta me but now I'm on a path. Walked 5 miles today. Cut out soda. Started meditating. I'm not fixed but I'm fighting. If you're reading this and feel off-don't wait. Don't wait for a collapse. Don't wait for someone to validate your pain. Your body's already screaming. Just listen. ❤️
lol so women are just too delicate for real heart attacks? i mean come on. my grandpa had a heart attack at 72 and he was out golfing the next day. you're telling me a woman can't handle it? maybe stop eating so much sugar and get off the couch. also, why are we giving out fancy blood tests like they're magic wands? just eat less pizza.
I want to say something real. I lost my mom to this. She was 56. She kept saying her back hurt, she was tired all the time, she felt like she was drowning even when she was sitting still. We thought it was arthritis. Then one morning she didn’t wake up. The autopsy said she’d been having silent heart attacks for over a year. I’m not trying to scare you. I’m trying to save you. If you feel like you’re running on empty, even if you’re ‘just a woman’ or ‘too young’ or ‘no family history’-get checked. Not tomorrow. Today. I’m begging you.
Look, I don’t care if you’re a woman, a man, or a sentient toaster-if you’re not taking responsibility for your health, you’re part of the problem. This isn’t about gender bias, it’s about personal accountability. You think a blood test is going to save you? No. It’s diet. It’s exercise. It’s quitting being a couch potato. Stop blaming the system. Start lifting weights. Stop eating processed crap. Your heart doesn’t care about your trauma-it cares about your LDL levels. Get real.