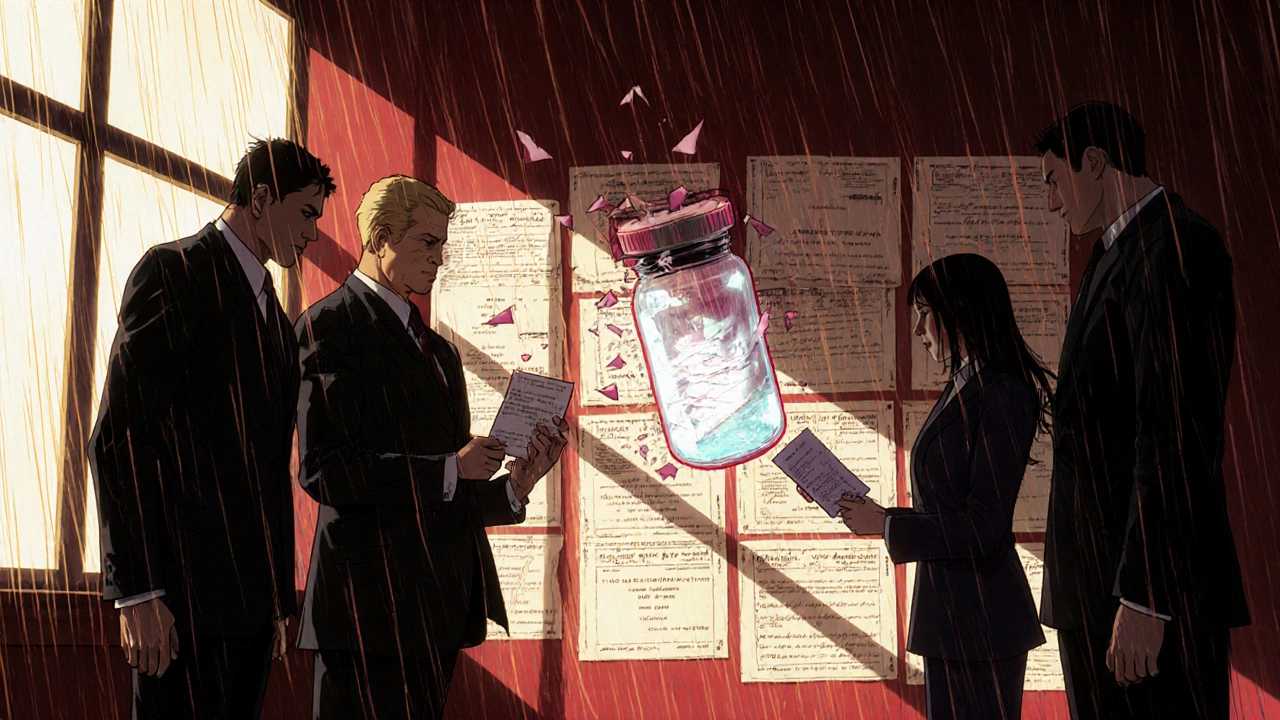
FDA Exclusivity: What It Means for Drug Prices and Access
When you hear FDA exclusivity, a period of market protection granted by the U.S. Food and Drug Administration to drug manufacturers, separate from patents. Also known as drug exclusivity, it’s not about owning an invention—it’s about controlling who can sell a copy after approval. This isn’t a patent. It’s a legal delay, built into the system, that stops generic versions from hitting the market—even if the patent has expired. For patients, that means higher prices. For manufacturers, it’s a reward for investing in clinical trials or studying drugs for new uses.
FDA exclusivity shows up in many places across your prescriptions. If you’ve ever wondered why a new drug costs $1,000 a month and then drops to $50 a year later, exclusivity is why. It’s the reason some drugs stay brand-only for five years, seven years, or even twelve. For example, orphan drugs—those treating rare diseases—get seven years of exclusivity just for being approved for a rare condition. New chemical entities get five years. Pediatric studies can add six more months. And if a drug is the first to treat a specific condition, it might get three years of exclusivity just for that new use. These rules aren’t random. They’re designed to balance innovation with access.
It’s not just about big pharma. This system affects your pharmacist, your insurance, and your wallet. When exclusivity ends, generics flood in. That’s when you see price drops of 80% or more. But until then, you’re stuck paying the brand price—even if the drug’s formula hasn’t changed. That’s why knowing about exclusivity helps you ask better questions: Is there a generic coming? Why is this drug so expensive? Can I wait? The posts below break down real cases where exclusivity shaped treatment options—from switching to biosimilars, to understanding why some medications have no cheap alternatives, to how hidden ingredients in pills can be tied to these same regulatory timelines. You’ll see how exclusivity connects to drug safety, patient choices, and even how travel meds are stored or how vegan-friendly a pill really is. This isn’t just policy. It’s personal.
Biologic drugs in the U.S. enjoy 12 years of exclusivity before biosimilars can enter. Complex patents, high development costs, and legal delays keep prices high. Here’s how the system works-and why patients pay more than in Europe.
Read more