Inactivated Vaccines: What They Are, How They Work, and What You Need to Know
When you hear inactivated vaccines, vaccines made from pathogens that have been killed so they can’t cause disease but still trigger an immune response. Also known as killed vaccines, they’re one of the oldest and most reliable types of vaccines still in use today. Unlike live vaccines, which use weakened forms of a virus or bacteria, inactivated vaccines use pathogens that have been destroyed—usually by heat, chemicals, or radiation. This means they can’t replicate or cause illness, making them safer for people with weak immune systems, like older adults or those on chemotherapy.
These vaccines work by showing your immune system a dead version of the germ. Your body learns to recognize it, builds antibodies, and remembers it for next time. That’s why you often need multiple doses—boosters—to keep your protection strong. The polio vaccine, a key example of an inactivated vaccine used globally to eliminate wild poliovirus, is one of the most successful public health tools ever created. So is the hepatitis A vaccine, a shot that prevents liver infection caused by the hepatitis A virus, and the rabies vaccine, given after animal bites to stop the deadly virus from spreading. These aren’t theoretical—they’ve saved millions of lives.
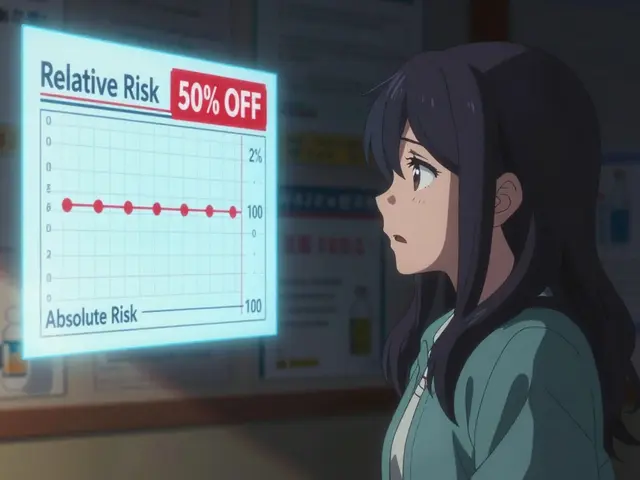
People often wonder if inactivated vaccines are less effective than live ones. They’re not. They just work differently. Live vaccines usually give long-lasting immunity with one or two shots. Inactivated vaccines often need three or four doses to build full protection, and sometimes require boosters every few years. That’s why you see tetanus shots every 10 years—it’s not because the vaccine wore off fast, but because your body needs a reminder. The trade-off? Fewer side effects. You won’t get a mild case of the disease from an inactivated shot, which is why they’re the go-to for people who can’t handle live viruses.
Some of the most common vaccines you’ve probably had are inactivated: flu shots (the injectable kind), whooping cough (part of DTaP and Tdap), polio (IPV), and hepatitis A. Even the newer COVID-19 vaccines from Moderna and Pfizer aren’t inactivated—they’re mRNA. But the older ones, like the ones used in developing countries or for people with certain health conditions, still rely on this tried-and-true method. They’re stable, easy to store, and don’t need ultra-cold freezers. That’s why they’re still used in global health programs.
Side effects? Usually mild: sore arm, low fever, maybe a headache. Serious reactions are rare. And unlike some live vaccines, you don’t have to worry about passing the virus to someone else after getting an inactivated shot. That’s a big deal for parents of newborns, grandparents, or anyone living with someone who’s immunocompromised.
What you’ll find in the posts below isn’t a textbook. It’s real, practical info from people who’ve dealt with these vaccines—whether they’re nursing mothers wondering about safety, caregivers helping older relatives stay protected, or patients managing chronic conditions and needing to avoid live vaccines. You’ll see how inactivated vaccines fit into daily health decisions, what the research says about timing and effectiveness, and how they compare with other options. No fluff. Just what you need to know to make smart choices.
Learn how to safely get vaccinated while on immunosuppressants, including which live and inactivated vaccines are safe, when to get them, and how to coordinate with your treatment plan to protect your health.
Read more