Immunosuppressant Vaccine Safety Calculator
Vaccine Safety Assessment Tool
Results will appear here after you complete the assessment.
Getting Vaccinated While on Immunosuppressants Isn’t One-Size-Fits-All
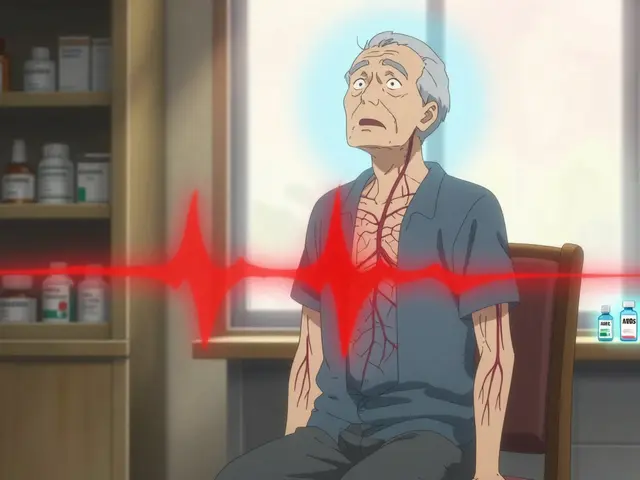
If you’re taking steroids, biologics, or other drugs that weaken your immune system, getting vaccinated isn’t as simple as walking into a pharmacy. The wrong vaccine at the wrong time can put you at risk-not from the disease, but from the vaccine itself. On the flip side, skipping the right vaccines leaves you dangerously exposed to infections that could land you in the hospital. The difference between safety and danger often comes down to one thing: whether the vaccine is live or inactivated.
Live Vaccines Are a No-Go for Most People on Immunosuppressants
Live vaccines contain a weakened version of the actual virus. In healthy people, that’s enough to trigger a strong immune response without causing illness. But if your immune system is turned down by drugs like prednisone, rituximab, or methotrexate, that weakened virus can still grow and make you sick. That’s why live vaccines are generally off-limits.
Examples of live vaccines you should avoid include:
- MMR (measles, mumps, rubella)
- Varicella (chickenpox)
- Zostavax (shingles vaccine-older version)
- Live attenuated influenza vaccine (LAIV-the nasal spray flu shot)
The BC Centre for Disease Control’s 2025 guidelines are clear: if you’re on moderate to high-dose immunosuppressants, these vaccines are contraindicated. Even low doses of steroids over two weeks can make you ineligible. One patient in Brisbane reported being scheduled for the nasal flu spray while on rituximab. Her infectious disease specialist had to step in to cancel it. That kind of mix-up still happens-and it’s avoidable.
Inactivated Vaccines Are Safe, But Timing Matters
Inactivated vaccines don’t contain live viruses. They use dead virus parts, proteins, or mRNA to teach your immune system what to fight. These are safe for people on immunosuppressants. But here’s the catch: your immune system may not respond as well. That’s why timing and extra doses are critical.
Safe inactivated vaccines include:
- Inactivated influenza vaccine (flu shot, not nasal spray)
- COVID-19 mRNA vaccines (Pfizer-BioNTech, Moderna)
- Novavax protein-based COVID-19 vaccine
- Hepatitis B (Engerix-B, Recombivax HB, Heplisav-B)
- Pneumococcal vaccines (PCV20, PPSV23)
But getting them at the wrong time can mean they don’t work. If you’re on rituximab or ocrelizumab, your B-cells are wiped out. Vaccines need B-cells to build lasting immunity. The IDSA 2025 guidelines say you should wait at least six months after your last dose before getting vaccinated. If you can’t wait, get the vaccine four weeks before your next infusion. That’s the sweet spot.
COVID-19 Vaccines for the Immunocompromised: It’s Not Just One Shot
For most people, one updated COVID-19 shot a year is enough. Not for you. If you’re immunocompromised, you need two doses of the 2025-2026 vaccine, regardless of your previous history. Some people need even more-depending on your condition and treatment.
Studies show antibody responses in immunocompromised patients range from 15% to 85%. That’s a huge gap compared to 90%+ in healthy people. That’s why extra doses aren’t optional-they’re lifesaving. One patient with rheumatoid arthritis skipped her methotrexate for a week after each dose and finally developed detectable antibodies. That’s the kind of fine-tuning that works.
Don’t assume your local pharmacy knows this. Many still give only one dose. Always bring your IDSA or CDC guidelines with you. And if the updated vaccine is out of stock? Push back. Delays cost lives. A kidney transplant patient in Queensland missed his booster during a winter surge because the pharmacy ran out. He got sick. He didn’t need to.
Timing Your Vaccines Around Your Medication Cycle
It’s not enough to know which vaccine to get. You need to know when.
For cyclical treatments like cyclophosphamide, the best time is during the “nadir week”-when your white blood cell count is starting to recover. That’s when your immune system is most able to respond.
For corticosteroids: if you’re on 20 mg or more of prednisone daily for two weeks or longer, wait until your dose drops below 20 mg before vaccinating. If you can’t reduce it, vaccinate anyway-but expect a weaker response.
For biologics like adalimumab or etanercept, vaccinate at least two weeks before your next dose. If you’re on monthly infusions, plan your shot for the week after your infusion, not before. That gives your body time to build immunity before the drug suppresses it again.
And here’s a pro tip: keep a log. Write down every drug, dose, and date. Include when you got each vaccine. Your specialist needs this. Your pharmacist needs this. Your future doctor will need this. Don’t rely on memory.
What About Your Family and Close Contacts?
Your vaccine isn’t the only one that matters. The people around you are your first line of defense. If your child gets the live nasal flu vaccine, they could bring the virus home-even if they don’t feel sick. That’s a risk you can’t afford.
All household members and close contacts should be fully vaccinated, including:
- Annual flu shot (inactivated)
- Updated COVID-19 vaccine
- DTaP (diphtheria, tetanus, pertussis)
- Varicella (if not immune)
Studies show this “cocooning” strategy cuts household transmission by 57%. That’s not a small win. It’s the difference between staying home and ending up in ICU.
What to Do If You’re Not Sure
There’s no universal rule. Your risk depends on your condition, your drugs, your dose, and how long you’ve been on them. The IDSA 2025 guidelines give you a framework, but your doctor needs to make the call.
Ask your specialist these questions:
- Am I considered moderately or severely immunocompromised based on my current treatment?
- Which vaccines do I need, and which ones are off-limits?
- When is the best time to get them relative to my next dose?
- Should I pause any of my meds around vaccination? If so, which ones and for how long?
- Can you refer me to a clinic that specializes in immunocompromised vaccination?
Specialized clinics like the Immunocompromised Vaccine Access Network (IVAN) now exist in over 40 U.S. locations and are starting to appear in Australia. They work directly with oncology and rheumatology teams to time vaccines perfectly. If you’re struggling to get coordinated care, ask for a referral.

What’s Changing in 2026?
The field is moving fast. By 2026, you might see point-of-care tests that measure your immune response on the spot-like a blood test that tells your doctor if you need one more dose or if you’re protected. The NIH is already testing adjuvanted vaccines designed specifically for people with weak immune systems. These could be game-changers.
Right now, the system is still catching up. Only 62% of community oncology clinics have standardized vaccination schedules. Most still wing it. That’s why you need to be your own advocate. Print out the IDSA 2025 guidelines. Bring them to your appointments. Don’t let confusion cost you your health.
Key Takeaways
- Live vaccines (MMR, chickenpox, nasal flu) are dangerous if you’re on immunosuppressants-avoid them.
- Inactivated vaccines (flu shot, COVID mRNA, pneumococcal) are safe-but timing and extra doses matter.
- If you’re on rituximab or similar drugs, wait 6 months after your last dose before vaccinating.
- For COVID-19, you need two doses of the 2025-2026 vaccine, not one.
- Coordinate with your care team. Log your meds and vaccines. Don’t guess.
- Make sure your household is fully vaccinated. It’s not just about you-it’s about protection.
Frequently Asked Questions
Can I get the flu shot if I’m on prednisone?
Yes, but only the inactivated flu shot (the injection), not the nasal spray. If you’re on 20 mg or more of prednisone daily for 14 days or longer, it’s best to wait until your dose drops below 20 mg. If you can’t reduce it, get the shot anyway-it’s still better than nothing. Your immune response may be weaker, but it’s safer than risking the flu.
I’m on rituximab. When should I get my COVID-19 booster?
Wait at least six months after your last rituximab dose. If you can’t wait that long, get the booster four weeks before your next infusion. This gives your body a chance to rebuild B-cells before the next round of treatment wipes them out again. Don’t wait until you’re sick to get it-plan ahead. Vaccine shortages are common, and delays can be deadly.
Do I need extra doses of the hepatitis B vaccine?
Yes. The standard three-dose series (at 0, 1, and 6 months) is recommended, but many immunocompromised people need a fourth dose. Ask your doctor to check your antibody levels after the third shot. If your hepatitis B surface antibody level is below 10 mIU/mL, you’ll need another dose. Some patients need up to four or five doses to build protection.
Can I get vaccinated during chemotherapy?
Yes, but timing matters. Avoid vaccination during the nadir-the week when your white blood cell count is lowest. Instead, schedule it during the recovery phase, usually 1-2 weeks after your chemo infusion. This gives your immune system the best shot at responding. Always coordinate with your oncologist before scheduling.
What if my doctor says I don’t need extra doses?
Get a second opinion. The CDC and IDSA guidelines are clear: immunocompromised patients need more than the standard schedule. If your doctor isn’t familiar with the 2025 updates, bring the guidelines with you. You can also call the CDC’s 24/7 clinical consultation line-they’ll talk directly to your provider. Your life depends on getting this right.
Next Steps
Start today. Make a list of every immunosuppressive drug you’re taking, including doses and how often you take them. Write down the dates of your last vaccine. Then, call your specialist and ask: “Based on my current treatment, which vaccines do I need, and when should I get them?” Don’t wait for an appointment. If you’re on a waiting list, call the pharmacy and ask if they carry the updated 2025-2026 COVID-19 vaccine. If they don’t, ask them to order it. And if you’re traveling, make sure you’re protected against travel-related diseases like hepatitis A and typhoid-both of which are inactivated and safe for you.
You’re not alone. Thousands of people are navigating this same path. The tools, guidelines, and support systems are here. You just need to use them.






Comments
Just got my flu shot yesterday. Inactivated, not the spray. Took the doc's advice and brought the IDSA guidelines. Pharmacy almost gave me the wrong one. Stay sharp.
lol why even bother getting shots if ur on meds anyway. they dont work. just waste of time. my cousin did all this and still got covid 3 times.
Actually, that’s not true. Studies show immunocompromised folks who get the full 2-dose series + boosters have 60-70% lower hospitalization rates than those who skip. It’s not perfect, but it’s the best shield we’ve got. Don’t let cynicism kill you.
The system is rigged. Pharma pushes vaccines to keep people dependent. You think they care if you live? They care if you keep buying meds. Live vaccines? They’re just Trojan horses. I’ve seen the data.
Oh wow. So now the CDC is in bed with Big Pharma and your rheumatologist is a puppet? Let me guess - you also believe the moon landing was real and that 2+2=4? Wake up. They’re sterilizing us with mRNA. It’s not science - it’s control.
The data is statistically insignificant. You're conflating correlation with causation. Also, your 'guidelines' are from 2025 - that's not even published yet. Who even wrote this? Some grad student with a blog? This is pseudoscience dressed as medicine.
There is a profound ethical tension here: the medical imperative to preserve life versus the systemic failure to personalize care. We treat immunocompromised individuals as a monolith - when in truth, each immune response is a unique constellation of biology, timing, and circumstance. The guidelines are a scaffold, not a cathedral. And yet, the architecture of healthcare refuses to bend to individual need. We demand uniformity in a world of chaos. This is not negligence - it is ontology.
I’m a veteran. I’ve seen what happens when you trust the system. They lied about Agent Orange. They lied about the Gulf War syndrome. Now they’re lying about vaccines. You think your ‘inactivated’ shot is safe? That mRNA? It’s not even real biology. It’s nano-tech. It’s designed to alter your DNA. And they’re testing it on people like us - the sick, the vulnerable - so they can say ‘look, it worked!’
To everyone panicking about vaccines: please talk to your specialist. Seriously. Don’t rely on Reddit. Don’t rely on random blog posts. Your rheumatologist or oncologist has access to real-time data, clinical trials, and vaccine response trackers. Bring them this post. Ask them to walk you through it. You’re not alone in this. We’ve got teams now - IVAN, CDC consult lines, specialty clinics. Use them.
I got my third COVID shot last week. They gave me the wrong one - said it was updated. Turned out it was last year’s. I called the CDC. They said ‘we’re out of stock in your county.’ I drove 90 miles. Got it. Then I called my insurance. They denied coverage because ‘it’s not standard.’ I’m not a statistic. I’m not a number. I’m a man who’s been through three transplants. And I will not be ignored.
You people don’t understand the science. The mRNA doesn’t just teach immunity - it reprograms your dendritic cells. It’s epigenetic. It’s designed to persist. And they’re using immunocompromised patients as guinea pigs because they know you won’t fight back. You’re being used. And you’re thanking them for it.
The real issue isn't the vaccine - it's the epistemic collapse of clinical medicine. The IDSA guidelines are written by bureaucrats with corporate funding. The ‘nadir week’ protocol? A myth perpetuated by lazy clinicians. Real science requires single-patient RCTs. We need N=1 protocols. Until then, we’re all just lab rats in a corporate cage.
Rituximab wipes out B-cells. No debate. The 6-month window isn’t arbitrary - it’s the time needed for B-cell reconstitution from hematopoietic stem cells. If you vaccinate before that, you’re triggering a T-cell-dependent response without humoral memory. That’s why antibody titers are flat. This isn’t opinion. It’s immunology.
They’re using vaccines to track us. The microchips are in the syringes. You think the QR codes on the vials are for inventory? No. They’re scanning your DNA. Your immune system is the key. They’re building a bio-digital ID. And you’re lining up for it. Wake up.