Medicine Temperature Control: Keep Your Drugs Safe and Effective
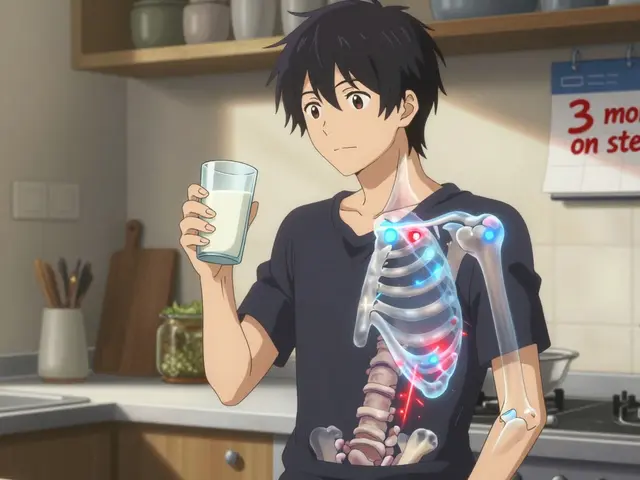
When you buy medicine, you’re not just paying for the chemical inside—you’re paying for medicine temperature control, the system that ensures drugs remain stable, potent, and safe from the factory to your medicine cabinet. Also known as pharmaceutical storage standards, it’s the unseen rule that stops your insulin from breaking down, your vaccines from going useless, and your antibiotics from turning into harmless powder. Most people assume pills are fine sitting on a windowsill or in a hot car, but that’s not true. Many medications, especially biologics, insulin, and certain antibiotics, start losing strength if they go above 77°F (25°C) or freeze. The FDA and WHO both say temperature matters—not as a suggestion, but as a requirement.
It’s not just about the drug itself. drug storage, how you keep your medications at home or on the go, directly affects whether they work when you need them. If you leave your epinephrine auto-injector in a glove box during summer, it could fail when you need it most. If you store your thyroid pills in a humid bathroom, moisture can ruin the coating and change how your body absorbs them. Even your fridge isn’t always safe—some drugs, like certain vaccines, need to stay between 36°F and 46°F. Too cold, and they freeze. Too warm, and they degrade. This is why pharmacies ship insulin with cold packs and why some clinics use temperature-loggers on vaccine fridges.
temperature-sensitive medications, a category that includes everything from biologics to eye drops, require careful handling at every step. You might not realize it, but your travel meds need the same attention. A study from the American Journal of Health-System Pharmacy found that 40% of travelers store insulin improperly during trips. That’s not just risky—it’s dangerous. The same goes for oral chemotherapy drugs, growth hormones, and even some probiotics. If you’re flying, never check your meds. Keep them in your carry-on. If you’re road-tripping, stash them in a cooler with a reusable ice pack—not in the trunk. And if your power goes out, know how long your fridge can keep things cold. Most medications can handle 24 hours at room temp, but not all.
You don’t need a lab to get this right. Start by reading the label. If it says "store at room temperature," that means 68°F to 77°F. If it says "refrigerate," keep it between 36°F and 46°F. If it says "do not freeze," don’t even think about putting it in the freezer. Use a simple thermometer in your medicine cabinet or fridge to double-check. Keep meds in their original bottles—those labels have storage info printed on them for a reason. And if you’re ever unsure, call your pharmacist. They’re trained to tell you exactly what to do, not just what to take.
The posts below cover real-world cases where medicine temperature control made the difference between healing and harm. You’ll find guides on storing insulin during travel, how heat affects your blood pressure pills, why some vaccines need cold chains, and how to handle meds when the power goes out. These aren’t theory pieces—they’re practical fixes from people who’ve been there. Whether you’re managing chronic illness, caring for a loved one, or just trying to avoid wasted prescriptions, this collection gives you what you need to keep your meds working as they should.
Learn how to protect your travel medications from heat, humidity, and freezing temps so they stay effective. Essential tips for insulin, EpiPens, and other sensitive drugs on long trips.
Read more