When your liver starts storing too much fat-not from drinking alcohol, but from how you eat and live-it’s not just a minor glitch. It’s nonalcoholic fatty liver disease, or NAFLD, now more accurately called MAFLD. This isn’t a rare condition. One in four people worldwide has it. In the U.S., it’s the most common liver disease you’ve never heard of. And here’s the scary part: it can quietly turn into scarring, cirrhosis, or even liver cancer if left unchecked. But the good news? In its early stages, it’s completely reversible.
What Exactly Is NAFLD/MAFLD?
NAFLD means fat builds up in your liver cells-more than 5% of the liver’s weight-without any heavy drinking or viral hepatitis causing it. It’s not just about being overweight. Even people with normal weight can have it if their metabolism is off. The name changed to MAFLD (Metabolic Associated Fatty Liver Disease) in 2020 because it’s not about what you’re not doing (drinking), it’s about what you are doing: having insulin resistance, high blood sugar, excess belly fat, or high triglycerides. These are the real drivers.
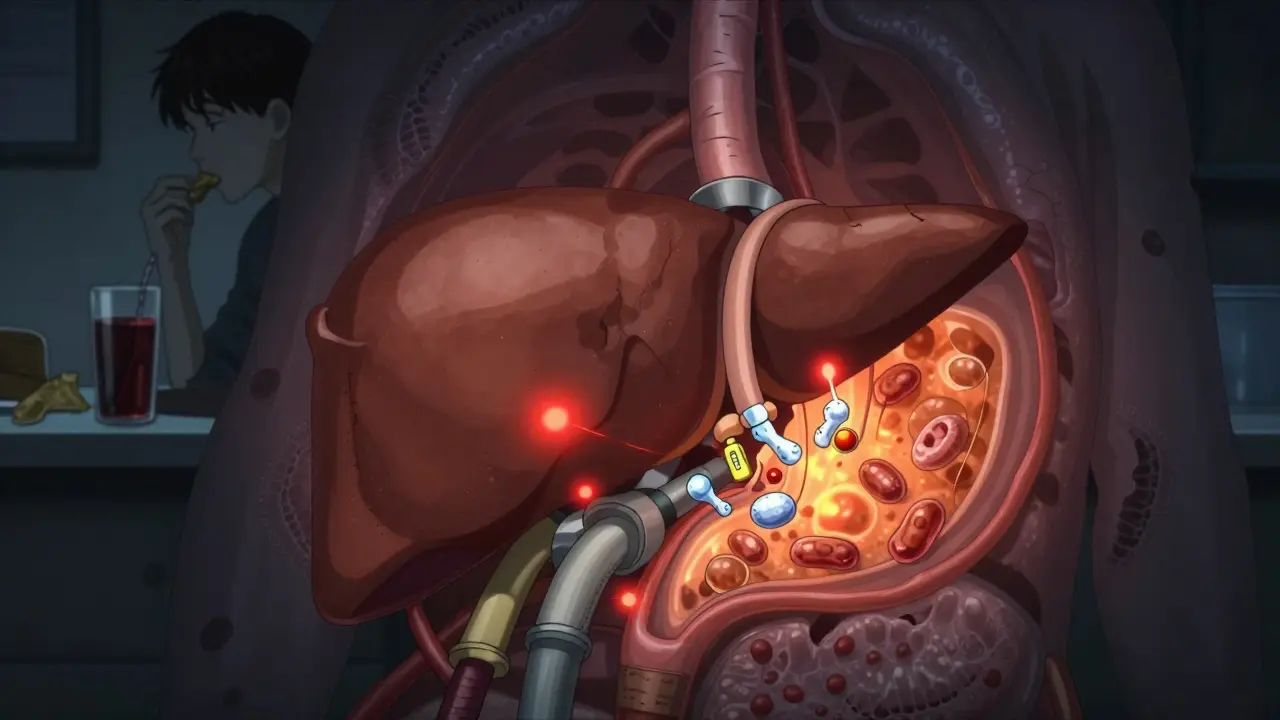
The liver doesn’t just sit there. It’s a chemical factory. When insulin resistance kicks in, your fat cells start leaking fatty acids into your bloodstream. Your liver, confused by all this energy flood, starts turning those fats into triglycerides and storing them. On top of that, your liver begins making its own fat from sugar-especially fructose from soda, fruit juice, and processed snacks. That’s right: sugar turns into liver fat. Studies show that in people with MAFLD, up to 26% of liver fat comes from this internal sugar-to-fat conversion. In healthy people, it’s only 5%.
How Does It Get Worse?
Having fat in the liver isn’t the end of the story. That fat isn’t harmless. It’s like having a leaky pipe in your basement-eventually, it causes damage. When fat builds up, it triggers inflammation. Your liver cells get stressed. Mitochondria (the powerhouses of your cells) start malfunctioning. Toxic fat molecules like ceramides and diacylglycerols pile up, damaging cell membranes and triggering cell death.
This is when simple fatty liver (NAFL) turns into NASH-nonalcoholic steatohepatitis. That’s the dangerous stage. Inflammation attracts immune cells. Liver scarring (fibrosis) begins. The liver tries to repair itself, but over time, it just builds more scar tissue. Think of it like a wound that won’t heal properly-it keeps forming tough, inflexible patches. Left unchecked, this can lead to cirrhosis, where the liver becomes lumpy and can’t function right. About 20% of people with NASH develop cirrhosis within 15 years.
And here’s what many doctors don’t tell you: not everyone’s liver gets worse. Some people stay stuck in the fat stage for life without progression. But others-often those with type 2 diabetes, high blood pressure, or obesity-see rapid decline. That’s why checking your liver isn’t optional if you have metabolic issues.
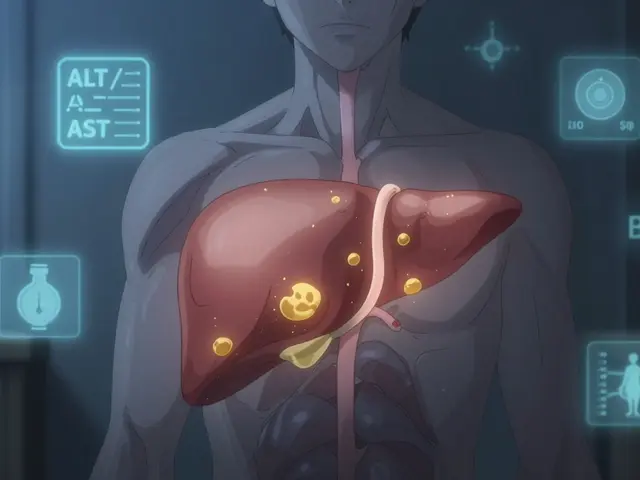
How Do You Know If You Have It?
Most people have no symptoms. No pain. No jaundice. No fatigue-at least not at first. That’s why it’s called a silent disease. It’s often found by accident during an ultrasound for another reason, or when routine blood tests show elevated liver enzymes (ALT, AST). But those enzymes can be normal even when there’s serious damage.
The gold standard for diagnosis used to be a liver biopsy. But now, non-invasive tools are replacing it. FibroScan, a quick, painless ultrasound-based test, measures liver stiffness and fat content. It’s accurate, fast, and widely used in Europe and Australia. In the U.S., only about 35% of primary care clinics have one. That’s a big gap.
If you’re overweight, have type 2 diabetes, high triglycerides, or high blood pressure, you should ask your doctor for a liver check. Don’t wait for symptoms. By then, it might be too late.
Reversing It: The Proven Path
The most powerful tool you have? Losing weight. Not a little. Not a quick fix. Real, sustained loss.
Studies show that losing just 3-5% of your body weight reduces liver fat. That’s about 6-10 pounds for someone weighing 200. But if you want to reverse inflammation and scarring, you need to lose 7-10%. In the LEAN study, 90% of people with NASH saw full resolution after losing 10% of their weight. That’s not a fluke. That’s science.
How you lose it matters more than how fast. Crash diets? They make it worse. Your body goes into survival mode, breaks down muscle, and your liver gets even more stressed.
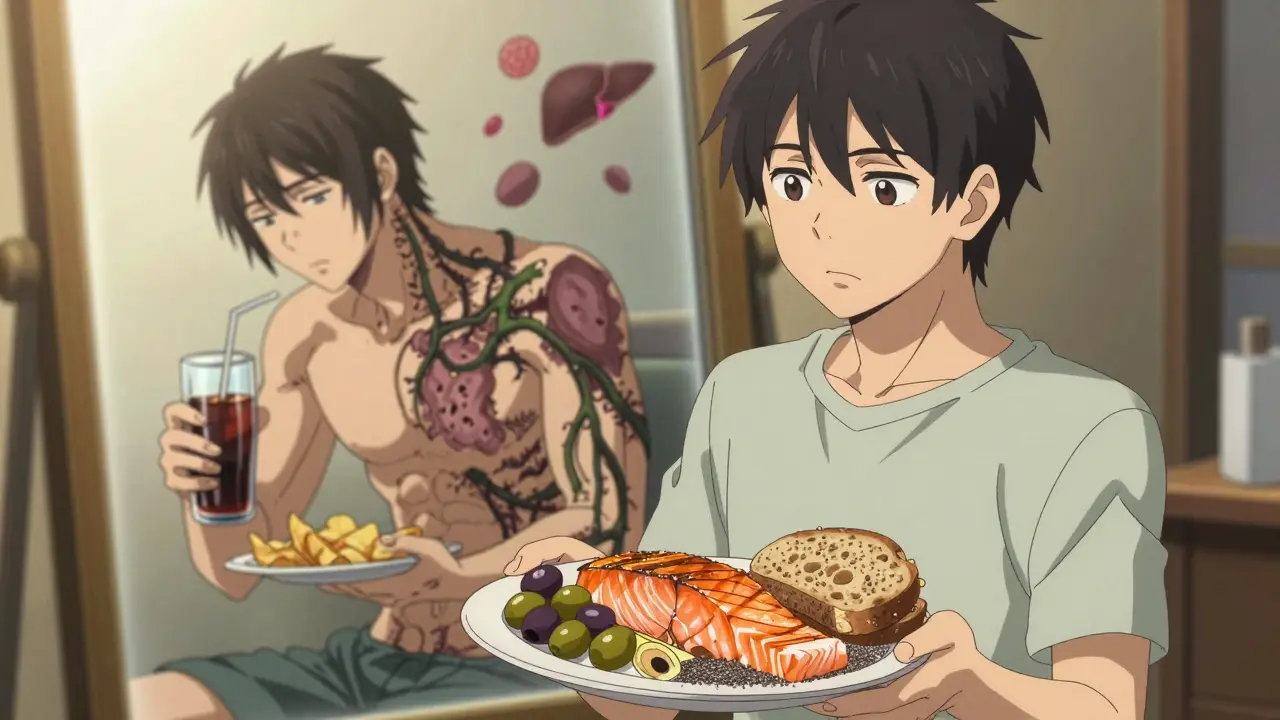
The Mediterranean Diet Works-Here’s How
The Mediterranean diet isn’t trendy. It’s backed by decades of data. It’s not low-fat. It’s high in healthy fats: olive oil, nuts, avocados, fatty fish. It’s rich in fiber from vegetables, legumes, and whole grains. It’s low in sugar and processed carbs.
A 2019 study showed that people following this diet for six months cut liver fat by 60-70%. Why? Because it reduces insulin resistance. It lowers inflammation. It cuts down on the sugar that turns into liver fat. And it’s sustainable. People don’t quit it because it’s satisfying, not restrictive.
Forget counting calories. Focus on these swaps:
- White bread → whole grain sourdough or rye
- Soda → sparkling water with lemon
- Processed snacks → almonds or olives
- Chicken nuggets → grilled salmon or lentils
And aim for 25-30 grams of fiber a day. That’s two apples, a cup of lentils, and a handful of chia seeds. Fiber slows sugar absorption, feeds good gut bacteria, and helps your liver breathe easier.
Exercise: Not Just for Weight Loss
You don’t need to run marathons. But you do need to move. Regular aerobic exercise-brisk walking, cycling, swimming-for 150 minutes a week cuts liver fat. Add two days of resistance training (weights, resistance bands, bodyweight squats), and you get 30% more fat reduction than aerobic alone.
Why? Muscle burns glucose. More muscle = better insulin sensitivity. Even if you don’t lose weight, exercise reduces liver fat. That’s huge. One patient I know lost 10% of his body weight and dropped his FibroScan score from F3 (advanced fibrosis) to F1 (minimal) after 12 months of daily walking and lifting weights. He didn’t take a pill. He just showed up.
What About Supplements and Pills?
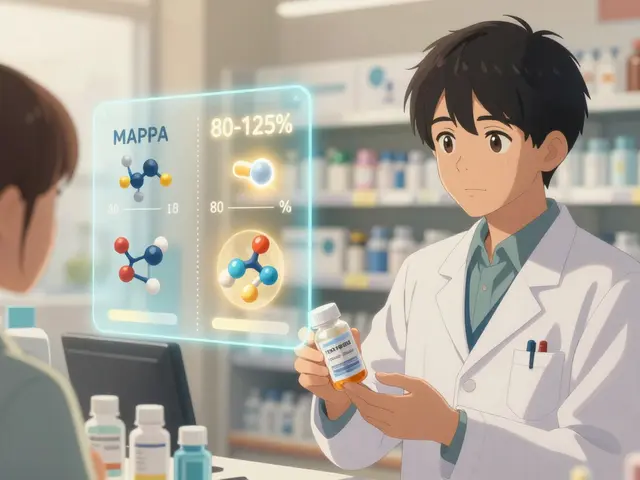
There’s no magic pill. But some are being used-and they work for specific people.
Vitamin E (800 IU daily) is approved for non-diabetic adults with NASH. It reduces inflammation. But long-term use has risks, including higher stroke risk. Don’t take it without medical supervision.
Pioglitazone, a diabetes drug, improves liver histology in over half of patients with NASH. But it causes weight gain and fluid retention. It’s not for everyone.
GLP-1 receptor agonists like semaglutide (Wegovy) and liraglutide (Saxenda) are game-changers. They help you lose weight, reduce liver fat, and calm inflammation. In trials, they cut liver enzymes and markers of fibrosis. But they’re expensive. Insurance often denies coverage for NAFLD alone-even though they’re FDA-approved for weight loss.
New drugs are coming fast. Resmetirom, approved by the FDA in March 2024, targets liver metabolism directly. In trials, it resolved NASH in 26% of patients and improved fibrosis. It’s the first drug specifically approved for this disease. More are in Phase 3.

The Gut-Liver Connection
Your gut and liver talk to each other. When your gut lining gets leaky (due to poor diet, stress, or antibiotics), toxins like LPS (endotoxin) leak into your bloodstream and hit your liver. That triggers inflammation.
Probiotics like Lactobacillus rhamnosus GG have been shown in studies to reduce liver fat by 30-40% in animal models by tightening the gut barrier. Human trials are promising. Eating fermented foods-sauerkraut, kimchi, plain yogurt, kefir-helps too.
Fecal microbiota transplants (FMT) from healthy donors have improved liver fat in early human studies. It’s still experimental, but it shows how deeply your gut microbiome affects your liver.
Why Most People Fail
Patients on forums like Reddit and HealthUnlocked say the same thing: "I tried. I ate better. I walked every day. But nothing changed for months."
That’s because progress is slow. Liver fat doesn’t vanish overnight. Liver enzymes take 3-6 months to normalize. Fibrosis takes 6-12 months to improve. Most people give up before they see results.
Also, many doctors still don’t take NAFLD seriously. A 2022 survey found 62% of patients felt their doctor didn’t understand their condition. You might need to be your own advocate. Bring research. Ask for a FibroScan. Ask about GLP-1RAs if you’re overweight and have diabetes.
What’s Next?
By 2030, NASH is expected to be the top reason for liver transplants. But we’re not helpless. The tools to reverse it are here: diet, movement, weight loss, and now, targeted drugs.
The biggest threat? The global obesity epidemic. The WHO predicts 3.3 billion adults will be overweight by 2035. That means more liver disease. But it also means more awareness.
AI tools like Deep Liver’s algorithm can now predict fibrosis progression with 89% accuracy-using just a blood test and a simple scan. Personalized care is coming.
Don’t wait for cirrhosis. Don’t wait for a diagnosis. If you have metabolic syndrome, insulin resistance, or extra belly fat-get your liver checked. Start eating real food. Move every day. Lose weight slowly, but keep going. Your liver doesn’t need a miracle. It just needs you to stop poisoning it.
It’s not about perfection. It’s about consistency. One meal. One walk. One day at a time. Your liver will thank you.



Comments
Man, I never thought my love for fruit juice was slowly turning my liver into a greasy fryer. I swapped all that crap for sparkling water with lemon and honestly? My energy’s up, my belly’s flatter, and my last bloodwork showed my ALT dropped like it was on a diet too. Who knew the real villain wasn’t pizza but the ‘healthy’ smoothie I drank every morning?
Let’s be real-this isn’t about ‘lifestyle.’ It’s about the government letting Big Sugar poison us while we’re busy scrolling TikTok. Fructose? It’s not a snack-it’s a slow-motion chemical weapon disguised as ‘natural sweetness.’ And don’t even get me started on how the FDA still lets ‘vitamin water’ with 40g of sugar sit on shelves next to milk! Wake up, America!
The metaphysical irony here is that the liver-a symbol of detoxification, of primal wisdom-is being sabotaged not by toxins from outside, but by the very metabolic arrogance of post-industrial consumption. We’ve turned sustenance into signal noise. The body, in its ancient wisdom, doesn’t know how to process the dopamine-driven, fructose-laced hallucinations of modern diet culture. It’s not fatty liver-it’s spiritual malnutrition.
And the drugs? Resmetirom? GLP-1 agonists? They’re not cures-they’re Band-Aids on a severed artery. We’re pharmacologically medicating the symptoms of a civilization that forgot how to eat. The real therapy is silence. Slowness. Unplugging from the algorithm and tasting food like it matters.
I was skeptical at first-thought this was just another ‘eat salad and lose weight’ article. But then I started doing the 150-minute walk + 2 days weights thing. Didn’t even lose much weight. But my FibroScan? Went from F2 to F0 in 8 months. No pills. No keto. Just consistency. If you’re reading this and feel stuck? Just show up. One walk. One less soda. One more veggie. That’s all it takes. Your liver doesn’t need perfection-it needs presence.
Look, I get it-you want to be ‘holistic.’ But let’s not pretend this is a Western problem. In Nigeria, South Africa, even rural India, people are getting NAFLD because they’re trading traditional whole foods for cheap, imported refined carbs and sugary drinks. It’s cultural colonization disguised as ‘progress.’ You think your avocado toast is the issue? Try surviving on subsidized white bread and powdered milk for 20 years. Then tell me it’s just ‘lifestyle.’
There’s a neuroendocrine cascade here that’s rarely discussed: chronic hyperinsulinemia → hepatic de novo lipogenesis → mitochondrial oxidative stress → ceramide accumulation → apoptosis → fibrogenesis. But boiled down? Sugar turns to fat inside your liver like a slow-motion oil spill. And the worst part? Your pancreas is screaming for help, but you’re too busy checking your Fitbit to notice. The liver doesn’t lie. It just doesn’t scream until it’s too late.
And yes-resmetirom is a breakthrough. But it’s not a cure. It’s a bridge. Until we fix the root-metabolic dysregulation caused by industrial food systems-we’re just rearranging deck chairs on the Titanic.
Oh please. You think eating ‘real food’ is the answer? My cousin ate nothing but kale and quinoa for a year and still got cirrhosis. Meanwhile, my uncle eats bacon, beer, and fried chicken every day and his liver enzymes are normal. So much for ‘science.’ This whole thing is just fear-mongering dressed up as nutrition. Wake up-your liver doesn’t care about your Instagram food pics.
Man, I used to think ‘liver detox’ was a scam. Then I stopped drinking soda, started eating lentils, and my wife said I stopped snoring. Not joking. My liver’s like a grumpy roommate-you treat it like trash, it’ll trash your whole house. But if you give it olive oil, fiber, and a little space? It’ll start doing its job again. It’s not magic. It’s just… basic. Like brushing your teeth. But nobody wants to hear that.
Let’s not pretend this isn’t a class issue. People with real access to organic produce, personal trainers, and doctors who actually listen? They reverse NAFLD. The rest of us? We’re stuck eating $1.50 frozen burritos because our jobs don’t pay enough for kale. This article reads like a luxury ad for the 1%. Meanwhile, my cousin works two shifts and still has a fatty liver. No one’s talking about that.
fibroscan? u sure it's accurate? my doc said alt can be normal even if u got scarring... so why even bother? i just eat what i want. my liver's fine. lol
The notion that ‘weight loss reverses NAFLD’ is oversimplified and potentially dangerous. It implies moral responsibility for a complex metabolic disorder, ignoring genetic predisposition, epigenetic factors, and pharmaceutical interference. The Mediterranean diet? Elegant, yes-but not universally applicable. One size does not fit all. To suggest otherwise is not science; it is ideological nutritionism.
Just wanted to say: I’ve been following the walking + weights routine for 6 months. My liver fat dropped 40%. I didn’t even lose 10% of my weight. Point is-movement matters. Even if you think you’re ‘not doing enough.’ Just keep showing up. You’re doing better than you think.
My grandma lived to 98 eating lard and cornbread. My cousin, vegan since 2015, got NASH at 34. This isn’t about food. It’s about stress. Sleep. Trauma. The body doesn’t care what’s on your plate-it cares if you’re alive or just surviving. Stop blaming the liver. Start healing the soul.
in nigeria, we call this 'oil liver'... people think it's from too much palm oil, but it's the sugar tea and bread. i tell my friends: stop drinking sweet tea. they laugh. but one stopped... his liver test improved. small change. big difference. 🙏
Big Pharma pushed this whole NAFLD thing to sell GLP-1 drugs. The real cause? 5G radiation + chemtrails. They don’t want you to know your liver can heal itself if you stop eating ‘processed food’ and start drinking distilled water with lemon and Himalayan salt. Also, the FDA is in cahoots with Monsanto. 🤫👁️