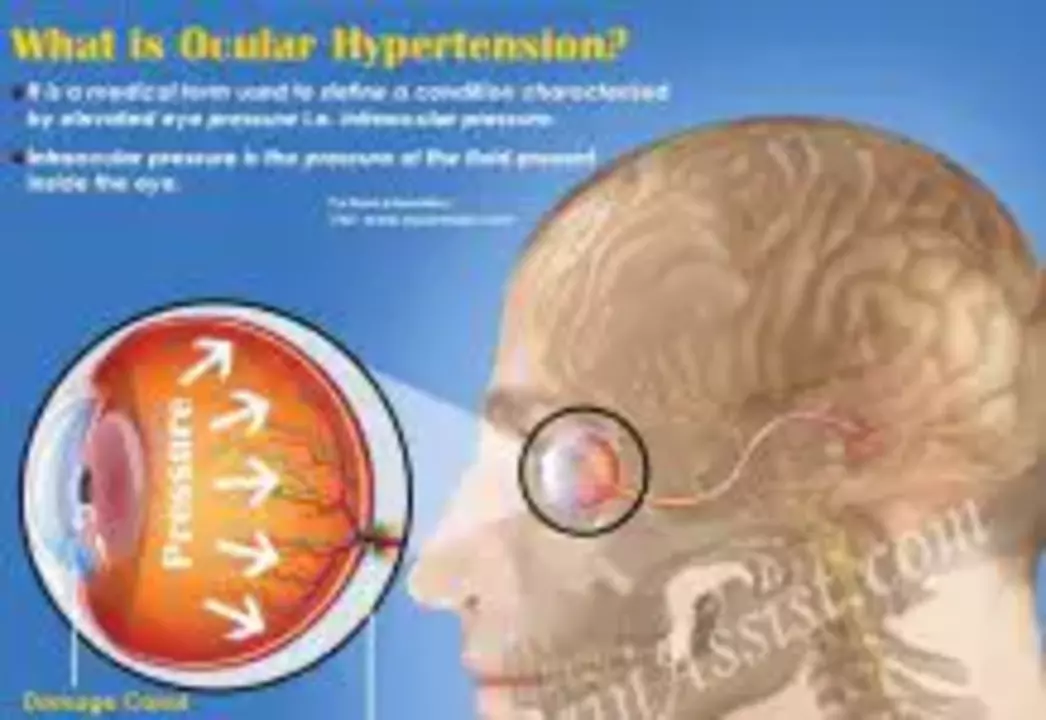
Understanding Ocular Hypertension
Ocular hypertension is a condition where the pressure inside the eye, known as intraocular pressure (IOP), is higher than normal. While it is not necessarily harmful by itself, it can be a risk factor for developing glaucoma, a serious eye disease that can lead to vision loss. In this section, we will explore the causes, symptoms, and potential complications of ocular hypertension.
The exact cause of ocular hypertension is not fully understood, but it is believed to be related to an imbalance in the production and drainage of aqueous humor, the fluid that fills the front part of the eye. Some possible risk factors include age, family history, certain medical conditions, and the use of steroid medications. Ocular hypertension does not typically cause any noticeable symptoms, which is why it is crucial to have regular eye exams to detect any possible issues. If left untreated, it can eventually lead to glaucoma and permanent vision loss.
Introduction to Brinzolamide
Brinzolamide is a medication that belongs to a class of drugs known as carbonic anhydrase inhibitors. It works by inhibiting the enzyme carbonic anhydrase, which plays a crucial role in the production of aqueous humor. By reducing the production of this fluid, brinzolamide effectively lowers intraocular pressure, making it a useful treatment for ocular hypertension. In this section, we will discuss the properties, mechanism of action, and potential side effects of brinzolamide.
Available as an eye drop solution, brinzolamide is typically prescribed to be used two to three times a day. The exact dosage and frequency of use will depend on the severity of the condition and the patient's response to the medication. Some common side effects of brinzolamide may include eye redness, blurred vision, and a bitter taste in the mouth. However, these side effects are generally mild and tend to subside as the body adjusts to the medication. It is essential to inform your doctor of any other medications or medical conditions you may have, as brinzolamide may interact with certain drugs or be contraindicated in some situations.
Brinzolamide vs. Other Glaucoma Medications
There are several types of glaucoma medications available, each working through different mechanisms to lower intraocular pressure. Some examples include prostaglandin analogs, beta-blockers, and alpha agonists. In this section, we will compare the efficacy and side effects of brinzolamide to these other classes of glaucoma medications.
Studies have shown that brinzolamide is effective in reducing intraocular pressure, though its efficacy may be slightly lower than that of some prostaglandin analogs and beta-blockers. However, brinzolamide has the advantage of causing fewer systemic side effects, making it a safer option for certain patients, particularly those with heart or lung problems. Additionally, brinzolamide can be used in combination with other glaucoma medications to achieve better IOP control, which can be particularly beneficial for patients with more severe or uncontrolled ocular hypertension.
Monitoring Your Progress with Brinzolamide
As with any medication, it is crucial to closely monitor your progress while using brinzolamide to ensure that it is effectively lowering your intraocular pressure and not causing any adverse side effects. In this section, we will discuss the importance of regular eye exams, potential warning signs to watch for, and how to communicate with your healthcare provider about your treatment.
Regular eye exams, including IOP measurements, are essential for tracking the effectiveness of brinzolamide and adjusting the treatment plan as needed. It is important to report any side effects or changes in your vision to your doctor, as these may be signs that the medication is not working as intended or that a different treatment approach is necessary. Keeping an open line of communication with your healthcare provider and following their recommendations will help ensure the best possible outcome for your ocular hypertension treatment.
Combination Therapy with Brinzolamide
For some patients, brinzolamide alone may not be sufficient to adequately control intraocular pressure. In these cases, combination therapy with other glaucoma medications may be necessary. This section will explore the benefits and considerations of using brinzolamide in conjunction with other IOP-lowering drugs.
Combination therapy can be highly beneficial for patients with more severe ocular hypertension or those who do not respond well to a single medication. By targeting multiple mechanisms that regulate IOP, combination therapy can provide a more robust pressure-lowering effect. Brinzolamide can be safely combined with other classes of glaucoma medications, such as prostaglandin analogs, beta-blockers, and alpha agonists. However, it is essential to closely monitor side effects and IOP levels when using multiple medications, as this can increase the risk of complications.
Lifestyle and Ocular Hypertension Management
While medications like brinzolamide play a crucial role in treating ocular hypertension, lifestyle factors can also have a significant impact on IOP levels and overall eye health. In this section, we will discuss some helpful tips and recommendations for managing ocular hypertension through lifestyle adjustments.
Maintaining a healthy lifestyle can help support the effectiveness of brinzolamide and other glaucoma medications. Some recommendations include engaging in regular physical activity, maintaining a balanced diet, and managing stress levels. Additionally, avoiding excessive caffeine intake and practicing proper eye care, such as wearing sunglasses to protect your eyes from harmful UV rays, can also contribute to maintaining healthy IOP levels. It is essential to discuss any lifestyle changes with your healthcare provider to ensure that they are appropriate for your specific needs and health condition.
Conclusion: The Importance of Early Detection and Treatment
In conclusion, brinzolamide is an effective and generally well-tolerated medication for the treatment of ocular hypertension. By reducing the production of aqueous humor, it effectively lowers intraocular pressure and helps prevent the development of more serious eye diseases, such as glaucoma. Regular eye exams, open communication with your healthcare provider, and maintaining a healthy lifestyle can all contribute to successful ocular hypertension management.
Early detection and treatment are crucial for preventing vision loss and other complications associated with ocular hypertension. If you have any concerns about your eye health or are experiencing any changes in your vision, do not hesitate to schedule an appointment with your eye care professional. Together, you can work to develop an effective treatment plan to protect your vision and overall eye health.



Comments
Behold, the silent tyrant that is ocular hypertension, lurking unseen yet poised to betray our sight. In the grand theatre of ophthalmology, brinzolamide strides onto the stage as a carbonic anhydrase inhibitor, daring to temper the relentless tide of aqueous humor. Its modest dosing schedule-two to three drops daily-belies the profound impact it can have on intra‑ocular pressure. Though a bitter taste may linger, the sacrifice is worth the promise of preserving vision. Let us not forget that vigilance, through regular exams, remains the loyal companion to any pharmacologic hero.
brinzolamide sounds like a solid option 😎💧
From a practical standpoint, brinzolamide can be paired with prostaglandin analogs when a single agent doesn’t achieve target pressure. Combining mechanisms often yields better control without drastically increasing systemic side effects, which is beneficial for patients with comorbidities. Monitoring IOP after each adjustment remains essential to gauge efficacy.
That’s a solid plan-just make sure you keep track of any redness or visual changes.
Got to love the simplicity of eye drops, right? 😅
Just remember: consistency is key, and don’t skip a dose even if you feel fine.
The interplay between lifestyle and IOP is fascinating; regular exercise and reduced caffeine can subtly aid the medication’s effect.
In a formal sense, it is advisable to document baseline intra‑ocular pressures prior to initiating brinzolamide and to schedule follow‑up assessments at regular intervals, typically every one to three months, to evaluate therapeutic response and adjust the regimen accordingly.
i think this med is overhyped. many ppl cant even affort it and the pharma will just push it for profit. can we trust the studies?
Oh sure, because nothing says "effective treatment" like a bitter‑tasting drop that leaves you questioning your life choices. Yet, here we are, still relying on it. How marvelously contrarian.
Let us consider the semantics: the inhibition of carbonic anhydrase reduces aqueous humor synthesis, thereby lowering intra‑ocular pressure-a fact that aligns with the principle of targeted pharmacotherapy. Precision matters.
brinzolamide?? maybe if u no other options.. idk.
Never forget that big pharma loves eye drops; they hide the real cure behind endless prescriptions. It's all about control, not health.
Supporting fellow patients is essential-share your experiences with brinzolamide, but always remind them to consult their eye specialist before making changes.
Ah, the noble pursuit of ocular equilibrium, a quest wherein brinzolamide holds its modest yet indispensable place. One must first recognize that intra‑ocular pressure, akin to a delicate tide, ebbs and flows under the governance of aqueous humour dynamics. By curbing the enzyme carbonic anhydrase, brinzolamide gently diminishes the production of this fluid, thereby averting the perilous ascent toward glaucomatous thresholds. Yet, let us not be complacent; the therapeutic regimen demands disciplined adherence, two to three administrations daily, lest the benefits wane like a sunrise behind clouds. In the grand mosaic of glaucoma management, combination therapy may be invoked, harmonizing brinzolamide with prostaglandin analogues, beta‑blockers, or alpha agonists, each contributing a unique mechanism of pressure reduction. While systemic side effects remain minimal-a virtue for patients with cardiopulmonary concerns-ocular irritation, transient redness, or a fleeting bitter taste may manifest, reminding us of the pharmacologic cost. Vigilant monitoring, through periodic tonometry, is paramount; without it, one risks the silent progression toward optic nerve damage. Lifestyle considerations-regular physical activity, moderated caffeine intake, and stress management-serve as adjuncts, bolstering the pharmacologic armamentarium. Moreover, patient education stands as a cornerstone; an informed individual is empowered to report adverse sensations promptly, facilitating timely adjustments. In sum, brinzolamide, though perhaps not the most potent monotherapy, earns its place as a reliable, well‑tolerated agent within the comprehensive strategy to safeguard visual function.