Prilocaine is a local anesthetic you’ve probably never heard of-until you need it. It’s the numbing agent used in dental fillings, minor skin procedures, and sometimes during childbirth. Unlike lidocaine, which most people recognize, prilocaine is quieter, less talked about, and often assumed to be just as safe. But that’s where things get tricky. While it works well for blocking pain, prilocaine carries a unique risk that few patients are warned about: methemoglobinemia. This isn’t a rare side effect. It’s a real, measurable danger that can turn your blood from bright red to chocolate brown, leaving you short of breath, dizzy, or worse.
What Prilocaine Actually Does
Prilocaine blocks nerve signals in your body, stopping pain signals from reaching your brain. It’s often mixed with epinephrine to make the numbing last longer and reduce bleeding during procedures. Dentists use it for root canals. Dermatologists use it before removing moles or stitching cuts. Anesthesiologists sometimes use it in epidurals. It’s fast-acting, low in toxicity compared to other anesthetics, and breaks down quickly in the body. That’s why it’s popular.
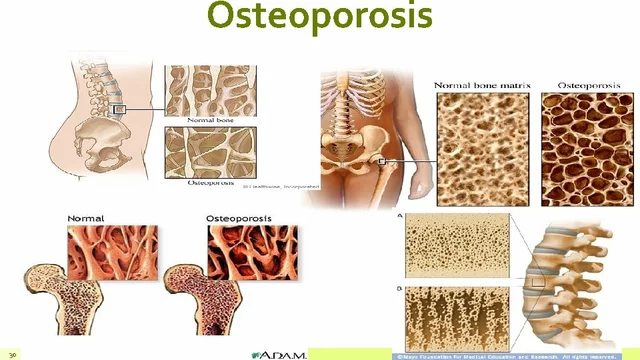
But here’s the catch: prilocaine breaks down into a chemical called o-toluidine. This compound interferes with hemoglobin-the protein in your red blood cells that carries oxygen. Normally, hemoglobin holds onto oxygen and releases it where your body needs it. When o-toluidine gets in the way, it changes hemoglobin into methemoglobin, which can’t carry oxygen at all. Your blood still looks red, but it’s not doing its job.
The Hidden Risk: Methemoglobinemia
Methemoglobinemia is the most serious side effect tied to prilocaine. It doesn’t happen to everyone. In fact, most people get a small amount of prilocaine and never notice anything wrong. But when it does happen, it can be dangerous. The risk goes up with higher doses-like when you get multiple injections in one visit, or if you’re given prilocaine for a large area like a full back procedure.
Symptoms usually show up within minutes to an hour after the injection. You might feel unusually tired. Your lips or fingertips could turn blue or gray. You might get a headache, feel dizzy, or notice your breathing is shallow. In severe cases, your skin turns a muddy brown color. Your pulse oximeter-the machine that checks your oxygen levels-might read normal, but you’re still not getting enough oxygen. That’s because those machines can’t tell the difference between normal hemoglobin and methemoglobin. Only a blood test can confirm it.
Studies show that methemoglobinemia from prilocaine happens in about 1 in 1,000 cases when doses exceed 400 mg. That’s more than most people get in a single dental visit. But if you’re getting a large skin procedure, like removing several moles or a tattoo, you could easily hit that threshold. Children and older adults are more vulnerable. People with certain genetic conditions, like G6PD deficiency, are at higher risk too.
Who Should Avoid Prilocaine
If you’ve ever had a bad reaction to a local anesthetic, or if you’ve been told your blood doesn’t carry oxygen well, you should speak up before any procedure. You don’t need to know the term methemoglobinemia-you just need to say, "I’m worried about side effects from numbing shots. Has this been used safely in people like me?"
Prilocaine is not recommended for:
- Infants under 6 months
- People with known methemoglobinemia
- Those with G6PD deficiency
- Pregnant women in the third trimester, unless absolutely necessary
- People taking medications that affect oxygen delivery, like nitroglycerin or certain antibiotics
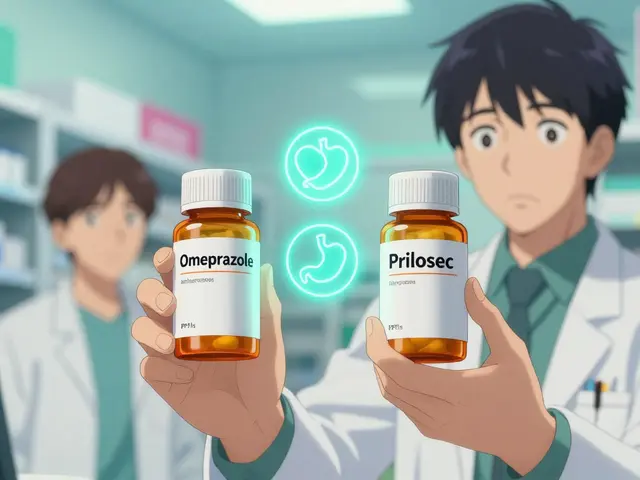
Even if none of these apply to you, it’s worth asking your provider if they’ve considered alternatives. Lidocaine, articaine, or bupivacaine are just as effective for most procedures and don’t carry the same methemoglobinemia risk.
What Happens If You Develop Methemoglobinemia
If you start feeling off after a prilocaine injection, don’t wait. Tell someone right away. If you’re at a clinic, alert the nurse or doctor. If you’re at home, call emergency services. This isn’t something you can treat yourself.
The treatment is simple if caught early: methylene blue. It’s a blue dye that’s been used since the 1930s to reverse methemoglobinemia. A single IV dose can restore your blood’s ability to carry oxygen within minutes. In mild cases, oxygen therapy alone may be enough. In severe cases, you might need a blood transfusion.
Most people recover fully if treated quickly. But if it’s missed, the lack of oxygen can damage your heart, brain, or other organs. There are documented cases where people went into cardiac arrest because methemoglobinemia wasn’t recognized. That’s why it’s so important to know the signs-even if you think you’re fine.
Alternatives to Prilocaine
You don’t have to accept prilocaine just because it’s the default option. Many clinics use it because it’s cheap and widely available. But there are better choices for safety.
Lidocaine is the most common alternative. It’s been used for over 70 years. It doesn’t break down into o-toluidine, so it doesn’t cause methemoglobinemia. Articaine is another option-it’s slightly stronger and faster-acting than lidocaine, and it’s widely used in Europe and Australia. Bupivacaine lasts longer, making it ideal for procedures where pain relief is needed for hours after.
Some providers still use prilocaine because they’ve always used it. But if you ask, most will switch without hesitation. You’re not being difficult-you’re being smart. Ask: "Is there another anesthetic that doesn’t carry the risk of methemoglobinemia?" If they say no, ask why. If they can’t explain, it’s time to find another provider.

What to Do Before Your Next Procedure
Before you get any local anesthetic, take five minutes to prepare:
- Ask what drug they’re using. Don’t assume it’s lidocaine.
- Ask if it’s prilocaine. If yes, ask why.
- Ask if there’s a safer alternative.
- Tell them if you’ve ever had trouble with oxygen or unusual reactions to medicine.
- If you’re getting multiple injections or a large area numbed, ask about total dosage limits.
Don’t be shy. This is your body. You have the right to know what’s going in it. Most providers appreciate the question. They’ve seen patients panic because they didn’t know what was happening. You’re preventing that.
Real Cases That Should Make You Pause
In 2023, a 68-year-old man in Queensland had three dental procedures done in one day. He got prilocaine each time. By the afternoon, he was dizzy and his lips turned blue. He went to the ER. His methemoglobin level was 28%-normal is under 1%. He needed methylene blue and stayed overnight. He’d never heard of prilocaine before.
In 2022, a newborn in Melbourne developed methemoglobinemia after a circumcision with prilocaine. The baby turned gray and stopped breathing. The medical team acted fast, but the child spent three days in intensive care. The hospital changed its protocol after that.
These aren’t outliers. They’re predictable. And they’re preventable.
Bottom Line: Prilocaine Isn’t Dangerous-But It’s Not Risk-Free
Prilocaine works. It’s not a bad drug. But it’s not the safest choice for everyone. The risk of methemoglobinemia is low, but when it happens, it’s serious. And unlike most side effects, it’s invisible until it’s too late.
If you’re getting a small procedure-like a filling or a mole removal-and you’re healthy, the odds are in your favor. But if you’re getting multiple shots, a large area numbed, or you have any underlying health issues, you should insist on an alternative. Lidocaine is just as effective. Articaine is just as common. There’s no reason to gamble with your oxygen supply.
Knowledge is your best defense. Ask the question. Know the signs. Don’t let silence be your only safety net.
Can prilocaine cause long-term damage?
In most cases, no. If methemoglobinemia is caught early and treated with methylene blue, full recovery happens within hours. There’s no evidence that a single episode causes lasting harm. But if oxygen levels stay low for too long-especially in children or older adults-it can damage the heart or brain. That’s why quick recognition and treatment matter more than the drug itself.
Is prilocaine banned anywhere?
No, prilocaine is not banned. It’s approved by the FDA, TGA in Australia, and the EMA in Europe. But some countries, like Sweden and Norway, have issued strong warnings against using it in children and during childbirth. Many clinics in Australia now avoid it for routine dental work unless there’s a specific reason.
Can I get prilocaine if I’m pregnant?
It’s not recommended, especially in the third trimester. Prilocaine crosses the placenta, and the fetus is more vulnerable to methemoglobinemia. Lidocaine is the preferred choice for pregnant women needing local anesthesia. If prilocaine is used, it’s only when the benefits clearly outweigh the risks-and even then, the dose is kept as low as possible.
How do I know if I have G6PD deficiency?
Most people don’t know unless they’ve had a reaction to certain medications, like sulfa drugs or antimalarials, or if they’ve had unexplained jaundice as a baby. A simple blood test can confirm it. If you’re of African, Mediterranean, or Southeast Asian descent, your risk is higher. If you’re unsure, ask your doctor before any procedure involving prilocaine.
What should I do if I feel weird after a prilocaine injection?
Don’t wait. Tell someone immediately. Symptoms like blue lips, dizziness, confusion, or trouble breathing are red flags. If you’re at a clinic, ask for help. If you’re at home, call emergency services. Don’t assume it’s just anxiety. Methemoglobinemia doesn’t go away on its own. Early treatment saves lives.






Comments
This is so important! 😊 I got prilocaine for a wisdom tooth removal last year and had no idea about this risk. My lips turned gray for like 5 minutes after - thought it was just nerves. Now I know it was probably mild methemoglobinemia. Always ask now. Thank you for sharing this 🙏
Of course the internet is full of fearmongering pseudo-medical nonsense. You think people should avoid a perfectly safe, FDA-approved anesthetic because of a 0.1% risk? That’s not awareness - that’s panic dressed up as education. If you’re going to be this anxious about every chemical in your body, maybe just don’t leave the house. Or better yet - stop posting this crap and let actual doctors do their jobs.
Prilocaine’s metabolite o-toluidine oxidizes hemoglobin’s ferrous iron to ferric, forming methemoglobin which cannot bind oxygen. The mechanism is well-documented in Anesthesiology journals since the 1970s. The LD50 for methemoglobinemia is approximately 300–400 mg in adults. The 1 in 1,000 incidence rate cited is conservative - studies from the UK and Australia show higher rates in pediatric populations. Lidocaine is not without risk either - it can cause CNS toxicity at higher doses. Context matters.
You know what’s wild? This whole post is basically a masterclass in taking power back from the medical system. 🙌 Most people just roll up, get numb, and assume everything’s fine. But you? You asked questions. You did your homework. And now you’re helping others do the same. That’s not being difficult - that’s being brave. Keep speaking up. The system doesn’t change unless people like you force it to. You’re not annoying - you’re essential.
I appreciate how clearly this was written. No fearmongering, no jargon overload - just facts, context, and actionable advice. I work in a clinic and we switched to lidocaine for all routine procedures last year after a patient had a mild reaction. It’s not about fear - it’s about choice. Asking "Is there another option?" is a reasonable question. No one should feel weird for asking it.
I’m a nurse and I’ve seen methemoglobinemia twice. Both times, it was from prilocaine in older patients with no warning. The scariest part? The pulse oximeter looked fine. We only caught it because the patient’s lips were blue and they said they couldn’t catch their breath. I wish every patient knew this. Please, if you’re reading this - ask your provider. It takes 10 seconds. It could save your life.
Let’s be real - this is just another example of the modern medical-industrial complex being lazy. Prilocaine is cheap. It’s easy. It’s been around. But it’s also a chemical landmine disguised as convenience. Meanwhile, lidocaine? Expensive. Requires more training. So they stick with the dangerous default. And now you’re being told to "just ask" - as if the patient has the power to negotiate with a system designed to ignore them. Wake up. This isn’t about awareness. It’s about systemic negligence.
I’m from India, and here, dentists almost always use prilocaine - they don’t even tell you what’s in the shot. I had a friend’s brother go into cardiac arrest after a dental procedure - they didn’t know what was happening until it was too late. This post? It’s not just helpful - it’s lifesaving. Please, everyone - share this. Especially with elders. They don’t know to ask. And if you’re a doctor? Please, stop assuming. Start explaining.
I got prilocaine for a tattoo removal last year and my whole face went numb and I felt like I was gonna pass out and I thought it was the adrenaline but now I think it was the methemoglobinemia and I just kept breathing and it went away but I didnt tell anyone because I was embarrassed and now I feel like I almost died and no one even warned me and I hate that I trusted them and I hate that this is normal and I hate that people just accept this
Methylene blue is a dye used in the 1930s. Do you realize how many modern drugs have been banned because they were "safe" back then? This is the same pattern. The FDA approves based on outdated data. The EMA ignores pediatric risk. The fact that you’re being told to "just ask" is proof the system is broken. They don’t want you to know. They want you to stay quiet. Methemoglobinemia isn’t rare - it’s underreported. And you’re being lied to.
I’ve been a dental assistant for 15 years. We used to use prilocaine all the time. Then one day, a patient came back saying she felt weird after her filling. We checked her chart - she’d had three procedures in one day. We looked up the dosage limits. We switched to lidocaine. No drama. No fuss. Just better care. If you’re a provider reading this - you don’t need permission to do the right thing. Just do it.
Western medicine is obsessed with individual risk and ignores collective harm. In India, we have millions who can’t even afford basic dental care. You think they’re getting lidocaine? No. They’re getting whatever’s cheapest. So you come along and say, "avoid prilocaine" - but what’s the alternative? A system that doesn’t care? This isn’t empowerment - it’s privilege. You’re telling people to demand better while ignoring the fact that most don’t even have access to the baseline.
This whole thing is a scam. Prilocaine is fine. The real problem is that people are too lazy to breathe. If you’re getting dizzy after a shot maybe you need to stop eating carbs and start doing yoga. I’ve had 12 dental procedures with prilocaine and never had an issue. Your fear is your problem not mine
I’m curious - is there any data on how often methemoglobinemia is misdiagnosed as anxiety or panic attack? I’ve had patients tell me they felt "like they were dying" after a procedure and were told it was just nerves. Could this be happening more than we think?