Alfacalcidol Hair Loss Risk Calculator
Risk Assessment Tool
This tool helps assess your risk of hair loss while taking alfacalcidol based on your current dose, serum calcium levels, and other factors.
Ever heard that a vitamin D analog could be behind thinning strands? If you’ve started alfacalcidol and noticed more hair on your pillow, you’re not alone. This guide breaks down what’s really happening, who’s most at risk, and how to keep your scalp happy without ditching essential treatment.
What is Alfacalcidol?
Alfacalcidol is a synthetic form of vitamin D3, specifically 1α‑hydroxyvitamin D3. It bypasses the liver step needed to convert cholecalciferol into the active hormone, making it useful for people with kidney problems or certain bone disorders. Once in the bloodstream, the kidneys turn it into the fully active 1,25‑dihydroxyvitamin D, which regulates calcium and phosphate balance. Doctors prescribe it for osteoporosis, hypoparathyroidism, and chronic kidney disease‑related bone loss.
How Vitamin D Relates to Hair Health
Vitamin D isn’t just for bones; it plays a role in the hair growth cycle. Dermal papilla cells-those tiny structures that control follicle activity-express the vitamin D receptor (VDR). When VDR signaling is impaired, follicles can slip into the resting phase, leading to shedding. Research from the Journal of Dermatological Science (2023) shows that low serum 25‑hydroxyvitamin D correlates with higher rates of telogen effluvium, a type of diffuse hair loss.
Reported Side Effects: Hair Loss Cases
Although alfacalcidol is praised for its bone‑protecting benefits, a handful of case reports have linked it to unexpected hair thinning. In a 2022 Australian dermatology bulletin, three patients on high‑dose alfacalcidol (2 µg daily) experienced noticeable shedding within two months. All three had normal baseline vitamin D levels, suggesting the effect wasn’t from a deficiency correction but from an overshoot in active hormone levels.

Why Might Alfacalcidol Trigger Hair Loss?
- Calcium Overload: Excess active vitamin D pushes calcium absorption in the gut. High serum calcium can alter the hair follicle micro‑environment, making cells more prone to apoptosis.
- Hormonal Crosstalk: Elevated 1,25‑dihydroxyvitamin D can suppress the parathyroid hormone (PTH). PTH interacts with hair‑cycle regulators; its sudden dip may disrupt follicle signaling.
- Immune Modulation: Vitamin D shapes immune responses. In some individuals, a rapid shift can provoke an autoimmune flare, manifesting as alopecia areata‑like patches.
These mechanisms are still being pieced together, but they explain why not everyone on alfacalcidol sees hair loss-genetics, baseline calcium, and immune status matter.
Who Is Most at Risk?
- People taking doses above the standard 0.5-1 µg daily without regular serum monitoring.
- Individuals with pre‑existing hypercalcemia or borderline high calcium levels.
- Patients with autoimmune skin conditions such as seborrheic dermatitis or a family history of alopecia areata.
- Those who combine alfacalcidol with other calcium‑boosting supplements (e.g., calcium carbonate, vitamin D3).
Managing the Situation
If you suspect alfacalcidol is the culprit, don’t quit cold‑turkey. Instead, follow these steps:
- Schedule a blood test for serum calcium, phosphate, and 25‑hydroxyvitamin D. Aim for a baseline before any changes.
- Discuss dose adjustment with your prescriber. Reducing from 2 µg to 0.5 µg often normalizes calcium while still protecting bone.
- Consider adding a topical minoxidil regimen (2% for women, 5% for men) to stimulate follicles during the transition.
- If autoimmune‑type shedding appears, a short course of low‑dose corticosteroids may reset the immune balance-only under dermatologist guidance.
- Track hair shedding with a simple weekly count (pull test or pillow‑hair count). If the number drops steadily after dose change, the link is likely real.
When to Seek Help
Immediate medical attention is needed if you notice any of the following while on alfacalcidol:
- Rapid hair loss covering more than 30% of the scalp.
- New‑onset skin rashes, especially around hair follicles.
- Symptoms of hypercalcemia: nausea, frequent urination, or muscle weakness.
- Bone pain that worsens despite therapy.
These signs could indicate a broader metabolic issue rather than isolated hair loss.
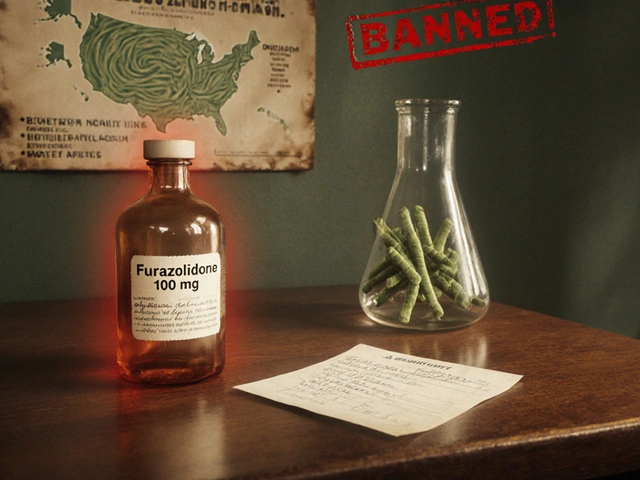
Alternatives to Alfacalcidol
For patients who can’t tolerate alfacalcidol, other options exist:
| Drug | Activation Path | Typical Dose | Hair‑Loss Risk |
|---|---|---|---|
| Cholecalciferol (Vitamin D3) | Liver → Kidney | 800-2000 IU daily | Low (requires liver/kidney function) |
| Calcifediol (25‑hydroxyvitamin D) | Liver‑derived, needs kidney activation | 0.25 µg daily | Moderate |
| Alfacalcidol | Liver bypassed, kidney‑activated | 0.5-2 µg daily | Potential (dose‑dependent) |
Switching to cholecalciferol may reduce scalp side effects, but it’s crucial to have renal function checked because the kidney still needs to finish activation.
Bottom Line
Alfacalcidol is a powerful tool for bone health, yet its ability to push calcium and hormone levels can unintentionally tip the hair‑growth balance. By monitoring labs, adjusting dosage, and keeping an eye on your scalp, you can stay on the medication without losing the hair you’ve worked hard to keep.
Can a short break from alfacalcidol reset hair loss?
A brief, doctor‑approved pause (usually a week) can lower active vitamin D levels, allowing follicles to recover. However, you should never stop abruptly without a replacement plan for bone protection.
Is hair loss a common side effect of alfacalcidol?
It’s uncommon; most patients experience bone‑related benefits without scalp issues. Reported cases usually involve higher-than‑recommended doses or underlying calcium imbalances.
Should I get a calcium test before starting alfacalcidol?
Yes. A baseline calcium, phosphate, and PTH panel helps the prescriber choose the right dose and spot anyone at risk for hypercalcemia‑related hair loss.
Can topical treatments counteract the hair loss caused by alfacalcidol?
Topical minoxidil is the most evidence‑backed option. It works by widening blood vessels around follicles, which can offset the temporary hormonal shift.
Are there dietary changes that help while on alfacalcidol?
Limit high‑calcium foods (e.g., fortified orange juice, excessive dairy) if labs show borderline levels. Focus on magnesium‑rich foods like leafy greens, which aid calcium balance.







Comments
Dude, that vitamin D spike can really mess with your mane!
While the anecdotal observations are valid, it is prudent to consider that serum calcium monitoring can delineate whether the hair loss is pharmacologically induced or merely coincidental. A review of the patient’s baseline labs, followed by a titrated dose adjustment, often mitigates the follicular shedding without compromising skeletal benefits.
Vitamin D receptors are abundantly expressed in the dermal papilla, so a sudden surge in active metabolite can throw the hair cycle into disarray. The literature you cited points to telogen effluvium as a downstream effect of disrupted VDR signaling. Moreover, calcium overload can induce follicular apoptosis, a mechanism highlighted in several dermatologic case series. It's also worth noting that patients with underlying autoimmune predispositions may experience an alopecia areata‑like picture when the immunomodulatory balance shifts. Regular monitoring of calcium, phosphate, and PTH therefore isn’t just a bone health checklist; it’s a scalp‑health safeguard. Adjusting the alfacalcidol dose to the minimal effective amount often restores equilibrium without abandoning therapy. In practice, incorporating a low‑dose minoxidil topical can serve as a bridge while labs normalize.
Yo, if you think the doc's just spitting pills you should quit, you’re missing the bigger picture – alfacalcidol ain’t some random candy. Shoudnt ignore the calcium spikes, they can turn your hair into a shed‑fest.
yeah man, i get ur point,, but like,, skipping meds totally can lead to bone fractures,, which is way worse,, tbh,, just get those labs checked,, keep it chill,,
They’re hiding the real side‑effects on purpose.
Oh my gosh!!! This whole alfacalcidol saga is like a soap opera for our scalps!!! 🎭💇♀️
While many readers may dismiss hair loss on alfacalcidol as an anecdotal nuisance, the biochemical cascade it initiates warrants a more nuanced discussion. First, the bypass of hepatic 25‑hydroxylation places a heavier reliance on renal 1‑α‑hydroxylase, which can produce supraphysiologic levels of 1,25‑dihydroxyvitamin D in susceptible individuals. These elevated active hormones increase intestinal calcium absorption, occasionally pushing serum calcium into a hypercalcemic range that is not immediately obvious clinically. Hypercalcemia, in turn, alters the extracellular matrix surrounding hair follicles, making the keratinocytes more prone to programmed cell death. Concurrently, the suppression of parathyroid hormone disrupts the delicate paracrine signaling that coordinates the anagen‑catagen transition, potentially prolonging the telogen phase. Adding to this complexity, vitamin D also modulates innate and adaptive immunity, and an abrupt shift can paradoxically ignite an autoimmune flare reminiscent of alopecia areata. The literature you referenced correctly notes case reports from Australia and Europe, yet larger cohort studies are still lacking, leaving clinicians to rely on case‑by‑case judgment. From a practical standpoint, baseline laboratory panels-including calcium, phosphate, 25‑hydroxyvitamin D, and PTH-are indispensable before initiating therapy. Subsequent monitoring every three to six months can catch incipient hypercalcemia before it manifests as follicular loss. Dose titration, especially reducing from 2 µg to the conventional 0.5–1 µg range, often ameliorates the hair shedding while preserving osteoporotic protection. For patients who cannot tolerate even low‑dose alfacalcidol, switching to cholecalciferol or calcifediol may provide a gentler activation pathway, albeit with the caveat of requiring intact hepatic function. Topical adjuncts such as minoxidil, though not a cure, can maintain follicular vascularity during the transitional phase. Nutritional adjustments-limiting excessive calcium‑rich foods and emphasizing magnesium‑rich greens-can also support calcium homeostasis. Finally, a collaborative approach involving endocrinologists, dermatologists, and primary care physicians ensures that both skeletal and scalp health are addressed in concert. In summary, alfacalcidol remains a valuable therapeutic agent, but its impact on hair biology should be monitored with the same rigor as its effects on bone, lest patients lose more than just their confidence.
whoa, that's a lot to take in, but basically keep an eye on labs and maybe swap to a milder vitamin d if your hair starts falling out, easy peasy.
Listen up!!! The pharmaceutical world loves to dump these “miracle” drugs on us without a disclaimer about losing our precious strands-seriously, it's a betrayal of trust!!! If you’re scared of a bald patch, you’re not alone; the community is shouting for clearer warnings!!!
I totally get the frustration; navigating treatment while watching your hair thin can feel overwhelming. It helps to set up regular check‑ins with your doctor and maybe keep a simple hair‑shed diary so you can see trends and adjust before it gets out of hand.