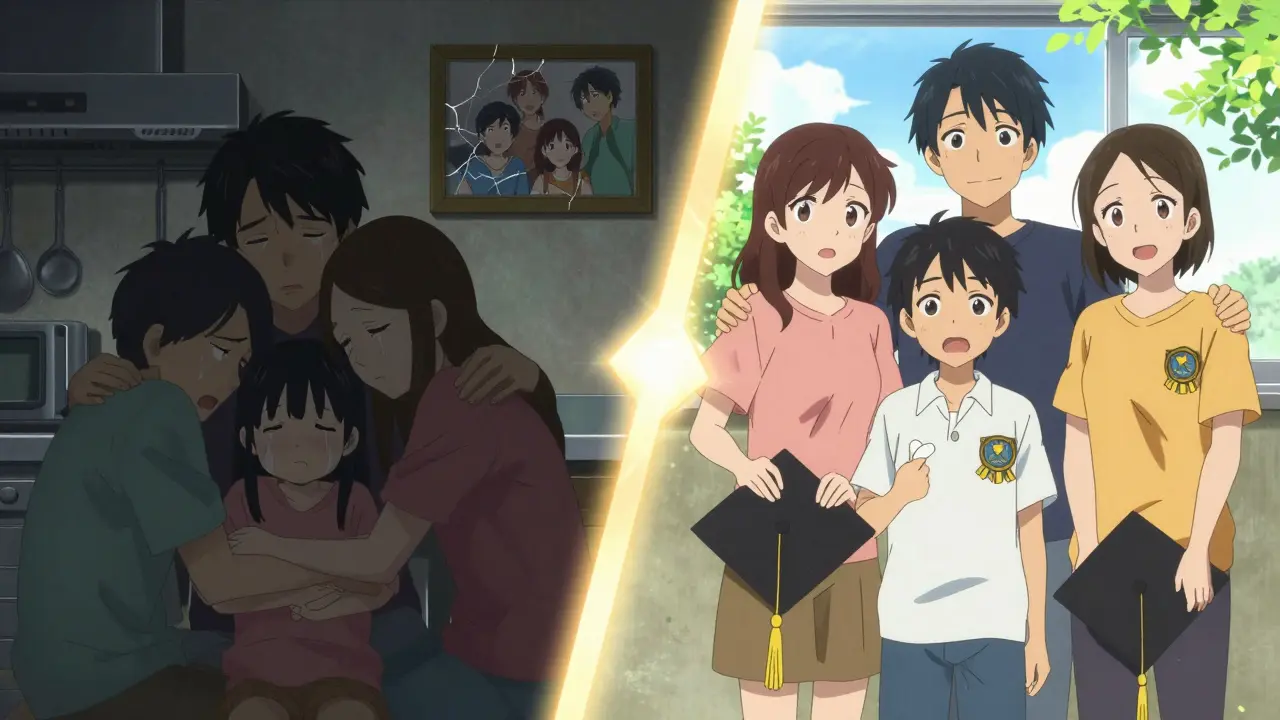
When someone experiences their first episode of psychosis, everything changes. They might hear voices no one else can hear, believe things that aren’t true, or struggle to speak clearly. It’s terrifying - not just for them, but for everyone around them. Families often feel lost, confused, and afraid they’re losing someone they love. The truth is, this moment is not the end of the story - it’s the most important turning point. First-episode psychosis is treatable. And when help arrives fast, with the right support, people don’t just recover - they rebuild their lives.
What Exactly Is First-Episode Psychosis?
First-episode psychosis (FEP) isn’t a diagnosis. It’s a warning sign - the first time someone’s brain starts to lose its grip on reality. Symptoms can include hallucinations (hearing, seeing, or feeling things that aren’t there), delusions (strong false beliefs, like being watched or persecuted), disorganized speech (jumping between topics or saying things that don’t connect), or behaviors that seem strange or out of place. These aren’t just "bad days." They’re signals that the brain needs urgent care.
It usually hits between ages 15 and 30. Think of a high school student suddenly withdrawing from friends, a college student stopping attendance, or a young adult quitting their job because they believe coworkers are plotting against them. These aren’t laziness or rebellion. They’re early signs of psychosis. And every day that passes without treatment makes recovery harder.
Why Timing Matters More Than Anything
There’s a window - a critical 12 weeks after symptoms start - where the brain is still responsive to treatment. The World Health Organization says if you wait longer than three months, you risk permanent damage to a person’s ability to work, learn, or maintain relationships. That’s not an exaggeration. Studies show that people who get help within six weeks have a 45% higher chance of full symptom remission than those who wait six months.
Why? Because psychosis isn’t just a mental event - it’s a biological one. The longer the brain is stuck in this altered state, the more it rewires itself around the symptoms. Think of it like a muscle that’s been overused in the wrong way. The sooner you correct the pattern, the better the outcome. Delayed treatment doesn’t just mean more symptoms - it means more hospitalizations, more lost jobs, more broken relationships.
The Gold Standard: Coordinated Specialty Care (CSC)
Forget the old way - one doctor, one pill, one appointment. That’s not enough. The new standard is Coordinated Specialty Care (a team-based approach that brings together medication, therapy, family support, and job training under one roof). It’s not just better. It’s dramatically better.
CSC teams include:
- A case manager who helps the person navigate appointments, insurance, housing - basically, life.
- A psychiatrist who prescribes antipsychotic medication at low, careful doses - never starting high. The National Institute for Health and Care Excellence (NICE) warns that doses over 400mg chlorpromazine equivalent increase side effects without helping symptoms.
- A therapist trained in cognitive behavioral therapy for psychosis, helping the person understand what’s happening without judgment.
- A vocational specialist who uses Individual Placement and Support (IPS) - a method proven to get 50-60% of participants back into work or school, compared to 20-30% with traditional programs.
- A family support specialist who runs structured education sessions.
These teams meet weekly. Every member talks to every other member. No one works in a silo. And it works. The RAISE study found that people in CSC stayed in treatment 65-75% of the time - compared to just 40-50% with standard care. Their quality of life improved 25% more. Their ability to work or study jumped 40%.

Family Support Isn’t Optional - It’s Essential
When psychosis hits, families aren’t bystanders - they’re frontline caregivers. But most have no idea what’s happening. They blame themselves. They panic. They push too hard or pull away completely.
Family psychoeducation changes that. It’s not therapy for the family. It’s education. Over 8 to 12 sessions, families learn:
- What psychosis actually is - not "crazy" or "evil," but a medical condition.
- How to respond to delusions without arguing. (Hint: Don’t try to convince them they’re wrong. Say, "I understand that feels real to you." Then shift focus.)
- How to reduce stress at home - which lowers relapse risk by 25%.
- How to support recovery without taking over.
Studies show that when families are involved, hospitalizations drop, medication adherence improves, and recovery speeds up. And yet, only 55% of eligible families even show up for these sessions. That’s a gap we can’t afford to ignore.
What Happens If You Don’t Act?
The cost of waiting isn’t just emotional - it’s financial. Untreated psychosis costs the U.S. $155.7 billion a year. That’s mostly lost productivity - people who can’t work, can’t study, can’t live independently. Early intervention? It cuts that cost to $28.5 billion. That’s an 80% savings.
And the human cost? A 3-6 month delay can mean the difference between finishing college and dropping out. Between keeping a job and losing it. Between living at home and needing long-term institutional care. The brain doesn’t recover the same way after prolonged psychosis. It’s not about willpower. It’s about biology.
Barriers to Care - And How Some Places Are Beating Them
Here’s the hard truth: only 18% of people with first-episode psychosis get help within the WHO’s 12-week window. Why? Because CSC programs are still rare. Only 35% of U.S. counties have them. In rural areas, it’s worse - 62% have no access at all.
Insurance is another hurdle. Only 31 states have Medicaid waivers covering all CSC components. That means families often pay out of pocket - or wait until the crisis is unbearable before seeking help.
But some places are proving it’s possible. Washington State’s New Journeys program reduced the average delay in treatment from 78 weeks to just 26 weeks. Louisiana uses mobile crisis teams that respond in under 14 days. Telehealth helped boost family participation by 35% during the pandemic. These aren’t miracles - they’re systems.
The Future: Digital Tools and Broader Access
Now, innovation is stepping in. The PRIME Care smartphone app tracks mood, sleep, and symptoms in real time. Early trials show a 30% drop in hospitalizations. The National Institute of Mental Health is pouring $50 million into research to find biological markers - blood tests or brain scans - that could detect psychosis before it fully develops.
But technology won’t fix this alone. We need funding. We need trained clinicians. We need policies that treat psychosis like diabetes or heart disease - not as a last-resort crisis.
What You Can Do Right Now
If you or someone you love is showing signs of first-episode psychosis:
- Don’t wait. Call a mental health provider today. Don’t wait for it to get worse.
- Find a CSC program. Use the Early Psychosis Intervention Network (EPINET) directory to locate one near you.
- Include family. Even if they’re scared, invite them to one session. Education changes everything.
- Ask about medication. Insist on low-dose, second-generation antipsychotics. Avoid high doses - they do more harm than good.
- Push for work or school support. Recovery isn’t just symptom-free - it’s life-filled.
The goal isn’t just to stop the voices. It’s to help someone get back to their life - their job, their studies, their friendships. And it’s possible. Not someday. Now.
What are the first signs of psychosis?
Early signs include social withdrawal, trouble concentrating, unusual beliefs (like thinking someone is spying on you), mood swings, neglecting personal hygiene, talking in a confusing way, or hearing faint noises that others don’t. These often start subtly - not with full hallucinations, but with changes in behavior, thinking, or emotion.
Is psychosis the same as schizophrenia?
No. Psychosis is a symptom - not a diagnosis. Schizophrenia is one possible diagnosis that includes psychosis, but many people have a single episode of psychosis and never develop schizophrenia. Other causes include severe stress, drug use, sleep deprivation, or other mental health conditions like bipolar disorder. Early intervention helps determine what’s really going on.
Do antipsychotic medications cure psychosis?
They don’t cure it - but they help control symptoms so recovery can begin. Medication is only one part of Coordinated Specialty Care. Low doses are used at first to reduce side effects. The goal is to use the least amount needed for the longest time, not to medicate indefinitely. Many people eventually reduce or stop medication with proper support.
Can family members really make a difference?
Yes - dramatically. Studies show that when families learn how to respond without judgment or pressure, relapse rates drop by 25%. Family support reduces stress at home, improves medication adherence, and helps the person feel safe. You don’t need to be a therapist. You just need to be informed and calm.
Why isn’t early intervention more widely available?
Mainly because funding is patchy. CSC programs cost more upfront - $8,000-$12,000 per person per year - compared to $5,000-$7,000 for standard care. But they save money long-term by preventing hospitalizations and lost productivity. Many states lack Medicaid waivers, and there’s a shortage of trained clinicians. Without consistent funding, these programs disappear after grants run out.
What should I do if I think someone is in crisis?
Call a crisis line or go to the nearest emergency room. But don’t wait for a full-blown crisis. If symptoms have been present for more than a few weeks, contact a mental health provider who specializes in early psychosis. You can also search for an EPINET-certified program online. The sooner you act, the better the outcome.






Write a comment