Over 470 million people worldwide live with asthma or COPD. For many, an inhaler is the difference between breathing normally and struggling for air. But here’s the hard truth: 70 to 90% of people use their inhalers wrong. That means most of the medicine never reaches their lungs. It’s not the device’s fault. It’s the technique.
Why Your Inhaler Might Not Be Working
You take your inhaler like clockwork. You feel like you’re doing everything right. But your symptoms don’t improve. Your rescue inhaler runs out faster than it should. You keep getting coughing fits or throat irritation. The problem isn’t that the medicine is weak-it’s that it’s not getting where it needs to go. Studies show that when technique is poor, only 8-30% of the dose actually lands in your lungs. That’s less than a third. With perfect technique, that jumps to 40-60%. That’s not a small difference. It’s the difference between staying out of the ER and needing emergency care. The reason? Most people don’t know how to use their inhaler properly. And doctors rarely check. A 2023 JAMA Internal Medicine study found that patients who had their inhaler technique reviewed at every visit had 22% fewer emergency trips. That’s not magic. That’s just making sure the medicine works.The Three Main Types of Inhalers
Not all inhalers are the same. There are three main types, and each works differently. Using the wrong method for your device means wasted medicine.- Metered-Dose Inhalers (MDIs) - These are the classic canisters you shake and spray. Examples: ProAir HFA, Ventolin HFA. They use a propellant to push out a puff of medicine. You have to press the canister and breathe in at the exact same time. If you’re too early or too late, most of the dose hits your throat instead of your lungs.
- Dry Powder Inhalers (DPIs) - These don’t need a propellant. You breathe in hard and fast to pull the powder into your lungs. Examples: Diskus, Turbuhaler, Ellipta. They’re easier for some people because there’s no timing to coordinate. But if you can’t take a strong, fast breath-like if you’re having a bad flare-up or are older-this device won’t work well.
- Soft Mist Inhalers - These are newer. They create a slow, fine mist that lasts about 1.5 seconds. Example: Respimat. You don’t need to time your breath as precisely. They’re good for people who struggle with coordination, but they’re not as widely available.
Here’s the catch: MDIs with a spacer are more effective than DPIs for most people. A spacer is a plastic tube you attach to the inhaler. It holds the puff so you can breathe in slowly. It cuts down on throat irritation and boosts lung delivery by 70-100%. The National Asthma Council Australia and the Global Initiative for Asthma (GINA) both recommend spacers for everyone using MDIs-even adults.
How to Use an MDI Correctly (With Spacer)
If you’re using a metered-dose inhaler, here’s the step-by-step that actually works:- Remove the cap and shake the inhaler well for 5 seconds.
- Attach the spacer. Make sure it’s clean and dry.
- Breathe out fully-away from the spacer.
- Place the spacer mouthpiece between your teeth and seal your lips around it.
- Press the inhaler once to release one puff into the spacer.
- Breathe in slowly through your mouth over 3-5 seconds. Don’t rush.
- Hold your breath for 10 seconds. This lets the medicine settle in your airways.
- Breathe out slowly.
- If you need a second puff, wait 60 seconds before repeating.
Common mistakes? People skip shaking the inhaler (45% do this). They breathe in too fast. They don’t hold their breath. They exhale into the spacer before pressing the canister. All of these kill effectiveness.

How to Use a Dry Powder Inhaler (DPI)
DPIs don’t need a spacer. In fact, using one with a DPI cuts effectiveness by 50-70%. Here’s how to use them right:- Load the dose as instructed. For Diskus or Ellipta, slide the lever until you hear a click. For Turbuhaler, twist the base until it clicks.
- Breathe out fully-away from the device. Never exhale into the mouthpiece.
- Put the mouthpiece in your mouth and seal your lips.
- Breathe in quickly and deeply-like you’re trying to suck a thick milkshake through a straw.
- Hold your breath for 10 seconds.
- Breathe out slowly.
Biggest mistake? People breathe in too slowly. DPIs need force. If you’re tired, weak, or having a bad day, you might not generate enough airflow. That’s why many older adults or people with severe COPD struggle with DPIs. A 2022 study from the National Asthma Council Australia found 62% of patients over 65 couldn’t use DPIs effectively. If you’re struggling, ask your doctor about switching to an MDI with a spacer.
What You Should Never Do
Some habits seem harmless. They’re not.- Never remove the capsule from a DPI. The powder is designed to be inhaled from the device. Opening it and trying to inhale the powder directly? You’ll get none of the dose. About 15% of users try this-per Allergy & Asthma Network.
- Never rinse your mouth after using a rescue inhaler. Only rinse after using corticosteroid inhalers (like fluticasone or budesonide). Rinsing reduces oral thrush risk by 75%. Skip this, and you could develop a yeast infection in your mouth.
- Don’t store your inhaler in the bathroom. Heat and humidity kill medicine. The FDA says storing above 30°C reduces effectiveness by 15-20%. Keep it in a cool, dry place-like your bedroom drawer.
- Don’t use multiple inhalers without training. Switching between MDIs, DPIs, and soft mist devices without learning each one? You’ll mess up technique. The European Respiratory Society says this cuts effectiveness by 35-50%.
When to Call Your Doctor
You don’t need to wait until you’re in crisis. Here are signs your inhaler technique might be off:- Your inhaler runs out faster than it should.
- You still feel tightness or wheezing after using it.
- You get frequent throat irritation, hoarseness, or a bad taste.
- You’ve never had your technique checked by a nurse or doctor.
- You’re unsure if you’re even getting the medicine.
Ask for a demonstration. Bring your inhaler to your next appointment. Ask: “Can you watch me use this?” Most doctors will say yes. If they don’t, ask for a respiratory therapist. They specialize in this.
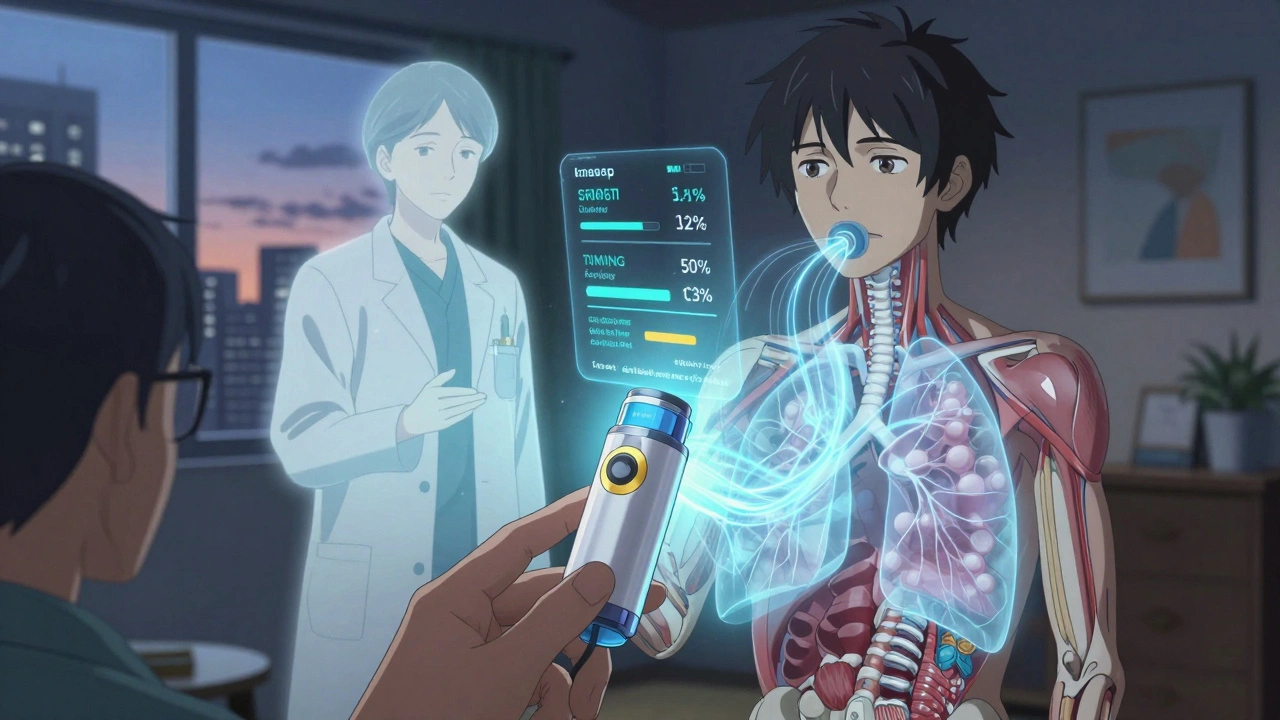
The Future Is Smart
Technology is catching up. In 2021, the FDA approved the first smart inhaler sensor-Propeller Health-that clips onto your device and tracks when and how you use it. It even tells you if your inhalation was too weak or too fast. A 2022 study in Annals of Internal Medicine found it was 92% accurate. By 2025, 40% of inhalers are expected to include digital tracking. That’s huge. It means your doctor will know if you’re using it right-not just if you’re using it at all. But here’s the thing: no smart device fixes bad technique. It just shows you that you’re doing it wrong. The real fix? Learning how to breathe right.Final Tip: Practice Like You Mean It
You wouldn’t drive a car without learning how to shift gears. Why treat your inhaler any differently? Practice in front of a mirror. Watch your lips seal. Watch your breath. Use a spacer. Hold your breath. Do it slowly. Do it again. YouTube has good videos. But don’t just watch-do it. Try it three times in a row. Then ask someone to watch you. Your lungs don’t care how much the inhaler costs. They don’t care if it’s branded or generic. They only care if the medicine gets there. And if you’re not getting it right? You’re not failing. You’re just untrained.Can I use my inhaler without a spacer?
Yes, but only if you’re using a dry powder inhaler (DPI). For metered-dose inhalers (MDIs), using a spacer is strongly recommended. Spacers increase lung delivery by 70-100% and reduce throat irritation. Without a spacer, most of the medicine sticks to your mouth and throat, making it far less effective.
Why does my inhaler sometimes taste bitter?
That’s usually a sign the medicine is landing in your mouth instead of your lungs. This happens when you don’t coordinate your breath with the puff (for MDIs) or breathe too slowly (for DPIs). Rinsing your mouth after using corticosteroid inhalers helps, but the real fix is improving your technique. If you’re always tasting it, your inhaler isn’t working as it should.
Are DPIs better than MDIs?
Not necessarily. DPIs are easier for people who struggle with timing, but they require a strong, fast breath. If you have severe COPD or are elderly, you might not generate enough airflow. MDIs with spacers work better for most people, including older adults and those with weak breath. The best inhaler is the one you can use correctly.
How long should I hold my breath after using an inhaler?
Hold your breath for 10 seconds. This gives the medicine time to settle into your airways instead of being breathed right back out. Studies show this increases lung deposition by 20-30%. If you can’t hold it for 10 seconds, do as long as you can-even 5 seconds helps more than nothing.
Can children use inhalers the same way as adults?
No. Children often can’t coordinate pressing and inhaling, or hold their breath for 10 seconds. For kids, the best option is an MDI with a spacer and a face mask. They breathe normally through the mask for 30-60 seconds after the puff is released. This is called tidal breathing and works better than forcing a deep breath.
Why does my inhaler feel empty but still has medicine in it?
MDIs often have a counter, but the canister can still spray even after the medicine is gone. The propellant lasts longer than the drug. Always check the number of puffs listed on the label and track how many you’ve used. Don’t rely on how it feels. If you’re unsure, take it to your pharmacy-they can test if it’s still active.
Can I share my inhaler with someone else?
Never. Even if the person has the same condition. Inhalers are personal medical devices. Sharing can spread infections like thrush or viruses. Plus, the dose and type of medicine are tailored to your needs. What works for you might be wrong-or dangerous-for someone else.
What should I do if I miss a dose of my maintenance inhaler?
If you miss a dose of your daily controller inhaler (like a corticosteroid), take it as soon as you remember. But if it’s almost time for your next dose, skip the missed one. Don’t double up. Consistency matters more than perfection. Missing one dose won’t cause a flare-up, but missing several over weeks can.







Comments
This is the kind of post that saves lives. I used to be one of those people who thought shaking the inhaler was optional. Turns out, I was just wasting money and breathing worse. Now I use a spacer every single time. My ER visits dropped from once a month to zero in six months. If you’re reading this and still not using a spacer-stop. Just stop. Go get one. Your lungs will thank you.
The data is unequivocal: improper inhaler technique is a public health failure disguised as patient negligence. The 70–90% misuse rate isn’t anecdotal-it’s documented across multiple global cohorts. Healthcare systems are failing by not mandating technique verification at every visit. It’s not about patient compliance; it’s about provider accountability. If your doctor hasn’t watched you use your inhaler in the past year, you’re being medically neglected.
They say spacers are the answer but who’s really behind this? Big Pharma knows people will buy new inhalers if they can’t use the old ones right. Spacers? They’re cheap. Why not just redesign the damn thing so it works without you needing a plastic tube? And why do they still use propellants that hurt the planet? This whole thing’s a scam. They want you dependent on gadgets, not educated. Also, your bathroom? Totally fine. I’ve had mine there for 8 years. Still works.
I’m from India and we don’t always have access to spacers, but I learned to use my MDI properly by watching videos on YouTube. The key is slow breath-not fast. I used to inhale like I was trying to suck up water from a puddle. Now I breathe like I’m smelling a flower. It made all the difference. No fancy gear needed. Just patience.
There’s an existential layer here beyond technique. We treat inhalers like tools, but they’re extensions of our autonomy. When you fumble the puff, you’re not just wasting medicine-you’re losing control over your own body’s rhythm. The 10-second hold isn’t medical advice; it’s a meditation. A pause to reclaim breath as something sacred, not mechanical. The spacer? It’s not a crutch. It’s a bridge between intention and outcome.
They’re hiding the truth. Smart inhalers? That’s surveillance disguised as care. Propeller Health? They’re tracking your every breath, feeding it to insurers, employers, maybe even the government. They don’t care if you breathe better-they care if you’re ‘compliant.’ And don’t get me started on the ‘rinse your mouth’ thing. That’s just to cover up the fact that steroids are slowly killing your immune system. Wake up. This isn’t medicine. It’s control.
Most people don’t realize that DPIs require peak inspiratory flow rates above 30-60 L/min. If you’re elderly or in a flare, your inspiratory flow drops to 15-20. That’s why DPIs fail. It’s physics, not laziness. MDIs with spacers are the only truly universal solution. The data doesn’t lie. The problem is doctors still think ‘just show them once’ is enough. It’s not. It’s like teaching someone to drive by handing them keys.
lol so you're telling me I've been wasting my money for 10 years because I didn't know to hold my breath? my bad. i thought the inhaler was magic. guess i'll just stop using it now. maybe i'll get lucky and die faster.
I teach asthma classes at the community center and I always bring my own inhaler and spacer. We practice together. One lady said she thought the spacer was for ‘smoking’ because it looked like a bong. We laughed, then we practiced. Now she’s been symptom-free for 8 months. It’s not about being smart. It’s about being shown. And being patient with each other.
thank you for this 💙 i used to hate my inhaler because it made my throat hurt and i felt dumb for not getting it right. now i use a spacer and i actually feel like i’m helping myself. it’s not magic, but it’s mine. i’m proud i learned how to do it right.
Hey-this isn’t just info. This is power. You’ve got a device in your hand that can keep you alive. But it only works if you treat it like a tool, not a chore. I used to be the guy who took 3 puffs at once because ‘it felt better.’ Now I do one. Slow. Hold. Breathe out. Repeat. My peak flow improved 40%. You can too. Just start today. One breath. One puff. One spacer. You’ve got this.
So… you’re saying the reason I’m still wheezing is because I didn’t shake it enough? My doctor gave me this thing 3 years ago and never asked me to demonstrate. Guess I’m just supposed to Google it? Cool. Thanks for the 20-page essay on how I’m failing. Now I feel great.