When a hospital adds a new drug to its list, it’s not just a paperwork exercise. It’s a high-stakes decision made by a team of pharmacists, doctors, and economists who weigh clinical data, patient safety, and cost - all while keeping supply chains intact. This process happens behind the scenes, but it directly affects what medication you get when you’re admitted, what your doctor prescribes, and even how long you stay in the hospital. At the heart of this system is the hospital formulary - a living, breathing list of approved medications that determines what’s available on the shelves and in the IV bags.
What Is a Hospital Formulary, Really?
A hospital formulary isn’t just a catalog. It’s a controlled list of drugs that the institution has vetted and approved for routine use. Unlike retail pharmacies where you can buy almost any brand or generic, hospitals operate on what’s called a closed formulary. That means if a drug isn’t on the list, it’s not stocked - unless there’s a special exception. About 87% of U.S. hospitals use this model, according to a 2022 study in PMC. The goal? To ensure every medication used has been proven safe, effective, and cost-efficient. The formulary typically includes between 300 and 1,000 drug dosage forms - think pills, injections, creams - and is updated regularly. Most academic hospitals review it quarterly. Community hospitals do it twice a year. These aren’t static documents. They’re living systems that respond to new evidence, drug shortages, and changes in patient outcomes.The Pharmacy and Therapeutics Committee: The Real Decision-Makers
Who decides what makes the cut? It’s not the CEO. It’s not the marketing rep from Pfizer. It’s the Pharmacy and Therapeutics (P&T) committee. This group usually has 12 to 15 members: clinical pharmacists, physicians from different specialties, a healthcare economist, and sometimes a nurse or administrator. Many are board-certified - pharmacists with BCPP credentials, doctors with specialty training. They meet monthly, sometimes more often, to review new drug requests. A drug doesn’t just walk in the door and get added. Someone - usually a clinician or pharmacist - has to submit a formal request. That request includes a dossier: clinical trial data, pharmacology details, comparisons to existing drugs, and evidence of cost savings. The committee doesn’t just look at price. They dig into how the drug affects hospital length of stay, readmission rates, and even how easy it is for patients to take correctly. A cheaper pill that causes more side effects? That might cost more in the long run.How Generic Drugs Get Selected: Beyond the Orange Book
Generic drugs are the backbone of hospital formularies. They make up 90% of prescriptions but only 26% of total drug spending, according to 2023 IQVIA data. But not all generics are treated the same. The FDA’s Orange Book tells you if a generic is bioequivalent to the brand - meaning it delivers the same amount of active ingredient into the bloodstream within 80-125% of the original. That’s the baseline. But hospitals go further. They look at:- Efficacy: At least 15-20 peer-reviewed studies per drug class, reviewed systematically.
- Safety: Adverse event data from the FDA’s FAERS database - not just what’s on the label.
- Formulation differences: A generic version with a different filler might cause stomach upset in some patients. That matters.
- Supply reliability: If a manufacturer has frequent shortages, the drug gets flagged - even if it’s cheap.

Tiers, Costs, and Patient Impact
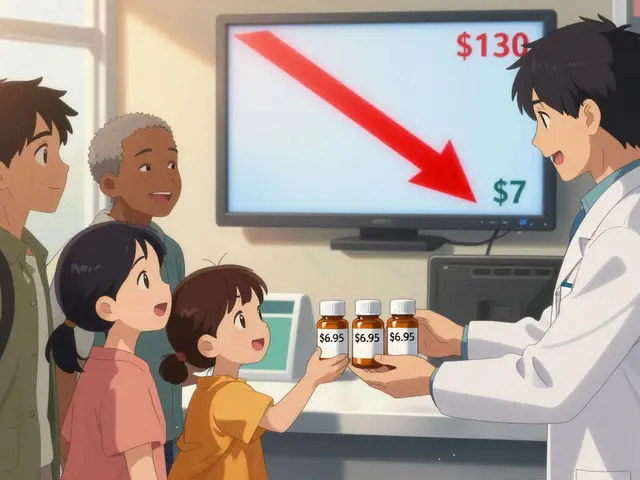
Most hospital formularies are divided into tiers. Generic drugs almost always sit in Tier 1 - the lowest cost tier. That means patients pay the least out of pocket. But here’s the twist: in hospitals, patient cost-sharing isn’t the main driver. It’s about clinical outcomes and system-wide savings. For example, switching from a brand-name ACE inhibitor to a generic version might save $10 per prescription. But if that switch reduces hospital readmissions by 5%, you’re saving thousands per patient. That’s why top hospitals now use predictive analytics to model the total cost of care, not just the acquisition price. A 2023 KLAS Research report found 61% of hospitals now use these tools. One case from Johns Hopkins saved $1.2 million annually by switching to formulary-preferred generic anticoagulants - with no rise in bleeding events. That’s the sweet spot: same results, lower cost.The Hidden Friction: When Formularies Cause Problems
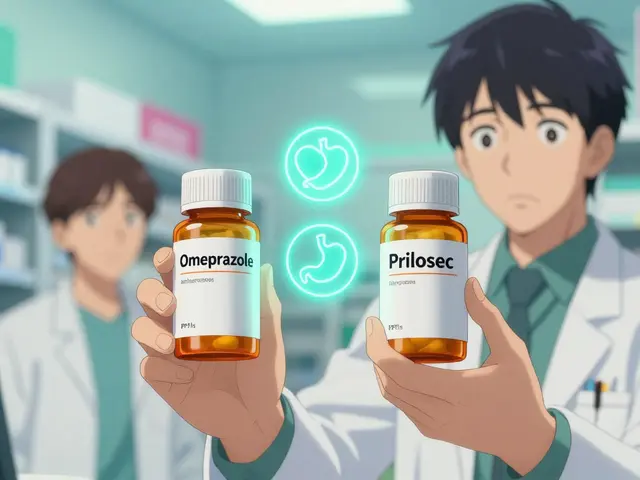
Formularies aren’t perfect. They create tension. A 2021 AMA survey found 32% of physicians felt formulary restrictions delayed patient care. Why? Sometimes, the preferred generic isn’t the best fit for a specific patient. A 68-year-old with kidney disease might need a different salt form than what’s on the formulary. But getting an exception means paperwork - prior authorization, appeals, delays. Nurses report workflow disruptions too. When a hospital switches from one generic to another, staff have to relearn dosing, storage, and administration. One AllNurses thread from March 2023 had 142 comments - 73% of nurses said medication errors spiked during transitions. Pharmacists and doctors also clash over therapeutic interchange. That’s when a pharmacist swaps a prescribed brand for a generic without asking the doctor. In 57% of cases, according to the American Pharmacists Association, physicians push back. They worry about subtle differences in absorption or patient tolerance. It’s not resistance to generics - it’s resistance to assumptions.
Who Influences the List? Industry, Data, and Ethics
You might think drug reps push hard to get their product on the formulary. You’re right. Dr. Jerry Avorn from Harvard documented in JAMA Internal Medicine that pharmaceutical detailing - sales reps visiting doctors - still influences decisions, even with conflict-of-interest disclosures. Hospitals now require annual COI training for all P&T members. But it’s not just pharma. Independent groups like the Institute for Clinical and Economic Review (ICER) now shape formulary decisions. Their cost-effectiveness analyses are used by 65% of large hospital systems. These reports look at long-term outcomes: quality-adjusted life years, hospitalization rates, even caregiver burden. That’s a big shift from just looking at pill price.What’s Next? Biosimilars, Genomics, and the Future
The biggest challenge ahead isn’t old generics - it’s new ones. Biosimilars, the biologic version of generics, are still catching on. Only 37% of hospital formularies have clear protocols for them, according to a 2023 FDA workshop. These drugs are complex. They’re not identical copies like traditional generics. They require different evaluation methods. Some hospitals are starting to use pharmacogenomics - testing a patient’s genes before prescribing. If a patient has a variant that makes them metabolize a drug slowly, the formulary might exclude certain generics. Eighteen percent of academic centers are piloting this. It’s early, but it’s the future. The Inflation Reduction Act of 2022 is also changing the game. By 2025, Medicare Part D rules will force hospital formularies to align more closely with outpatient drug coverage. That means even more pressure to standardize and reduce costs.Why This Matters to You
If you’re a patient, you might never see the formulary. But it’s why your doctor prescribed a generic instead of a brand. It’s why your IV bag looked different than last time. It’s why you didn’t get the drug your friend got at another hospital. It’s also why your hospital can afford to treat more people. Without formularies, drug costs would balloon. Hospitals would spend more on medication than on nurses. Formularies keep care affordable without sacrificing safety - when they’re done right. The system isn’t flawless. It’s bureaucratic. It’s slow. It sometimes gets it wrong. But it’s built on evidence, not profit. And in a world where healthcare costs are rising faster than wages, that’s the best safeguard we have.Are generic drugs as safe as brand-name drugs in hospitals?
Yes. All generic drugs approved by the FDA must meet the same strict standards as brand-name drugs. Hospitals go even further - they review clinical studies, safety data, and real-world outcomes before adding a generic to their formulary. The key is therapeutic equivalence: the generic must deliver the same amount of active ingredient into the bloodstream as the brand, within an 80-125% range. Most hospital formularies only include generics with an FDA ‘A’ rating in the Orange Book, meaning they’re fully interchangeable.
Why do hospitals use closed formularies instead of letting doctors prescribe anything?
Closed formularies help control costs, reduce medication errors, and ensure consistent care. Without them, doctors might prescribe expensive brand-name drugs when cheaper, equally effective generics exist. Hospitals also face supply chain issues - if a drug is in short supply, a closed system lets them quickly switch to a pre-approved alternative. It’s about standardization and safety, not restriction.
How long does it take for a new generic drug to get added to a hospital formulary?
The average review process takes 45 to 60 days. The request must include clinical evidence, cost data, and a comparison to existing drugs. The Pharmacy and Therapeutics committee meets monthly to review submissions. For urgent cases - like during a drug shortage - expedited reviews can happen in 14 to 21 days. But even then, evidence is required. There’s no shortcut for safety.
Can a hospital remove a generic drug from its formulary even if it’s still on the market?
Yes. Hospitals can and do remove generics for several reasons: supply shortages, new safety data, or the arrival of a better alternative. For example, if a new generic version has fewer side effects or lower cost, the old one may be phased out. In 2022, over 260 generic drugs experienced shortages in the U.S., forcing hospitals to temporarily suspend formulary status for affected products. It’s not about the drug being bad - it’s about finding the best option available.
Do formularies affect how quickly patients get their medications?
Sometimes. If a doctor prescribes a non-formulary drug, the hospital may require prior authorization - which can delay treatment by hours or days. But this only happens with drugs not on the list. Most common medications - especially generics - are already approved and available immediately. The goal is to prevent delays caused by expensive or unsafe choices, not to slow down care. In fact, formularies often speed up access by reducing confusion and ensuring the right drug is always stocked.






Comments
So let me get this straight - we’re paying $200 for a brand-name pill when a $2 generic does the exact same thing? 🤦♂️ And yet somehow, my cousin’s hospital still gives out the expensive one because ‘the doctor likes it.’ This isn’t healthcare. It’s a casino with stethoscopes. 💊💸
I work in a community hospital in Ontario and let me tell you - formularies are the unsung heroes. We cut 30% off our med bill last year by switching to generics with better supply chains. One guy complained his ‘brand’ was ‘more reliable’ - until we showed him the FDA bioequivalence data. He shut up. And then he thanked us. 🤝💉 Don’t let the hype fool you - generics aren’t cheap because they’re bad. They’re cheap because they’re *smart*.
I love how people act like formularies are some evil corporate plot. Nah. It’s just nurses and pharmacists trying to keep you alive without bankrupting the system. I’ve seen patients get the wrong generic because the label looked similar - that’s why we standardize. It’s not control. It’s care. ❤️🩺
The system works until it doesn’t and then everyone acts surprised
The real innovation isn’t the generics - it’s the *data-driven* P&T committees that now integrate real-world evidence from EHRs, FAERS, and even patient-reported outcomes. We’re moving from reactive formularies to predictive formularies - where algorithms flag potential adverse events before the drug even hits the shelf. It’s not just cost containment anymore. It’s precision pharmacology. 📊🧬
You know what’s funny? The same people who scream about Big Pharma are the ones who get mad when a hospital doesn’t stock their favorite brand. Meanwhile, the ‘generic’ they’re mad about? Same active ingredient. Same FDA approval. Same clinical outcomes. But no - it has to be the one with the rainbow logo and the jingle on TV. It’s not about safety. It’s about branding. And we’re all just pawns in a $500 billion marketing game. 🎭💊
In India, formularies are a luxury. We have hospitals where the drug list is written on a napkin. The ‘generic’ is often a counterfeit. The ‘bioequivalence’ is a fantasy. Your system is advanced. Ours is survival. Do not mistake your privilege for progress.
If you think hospitals care about patients, you’ve never seen the formulary committee minutes. They don’t pick drugs based on what’s best for you. They pick what’s easiest to audit. What’s cheapest to buy. What doesn’t trigger a whistleblower call. You’re not a person. You’re a line item.
I got switched to a generic for my blood pressure and I swear I felt like a robot. Like my body didn’t recognize it anymore. I had headaches for a week. My nurse said it was ‘just placebo.’ But I know what I felt. They don’t listen. They just push the cheap stuff.
I get why people are frustrated. I really do. But I’ve also seen what happens when a hospital doesn’t have a formulary - random meds, confusion, errors, delays. It’s chaos. The system isn’t perfect, but it’s the best we’ve got. Let’s fix the gaps, not tear it down. We all want the same thing: safe, affordable care. Let’s work together.
generic drugs r just as good but no one tells u that bc pharma wants u to think u need the fancy one lol
In India, we call generics ‘life-savers’ - not because they’re cheap, but because without them, millions couldn’t afford treatment. I once saw a diabetic man cry because he got his insulin for $1 instead of $100. That’s not a formulary. That’s dignity. Your system is complex. Ours is survival. Both matter.
The formulary is a necessary mechanism for institutional efficiency and pharmacoeconomic accountability. Without standardized protocols, therapeutic variability would compromise clinical integrity and increase liability exposure.