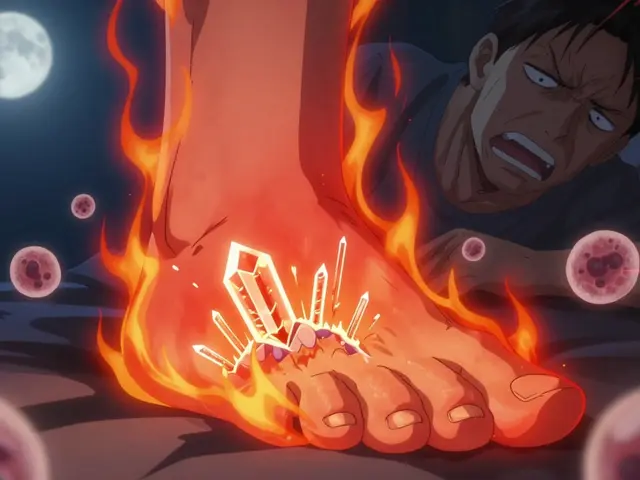
When your big toe suddenly swells up like a balloon, turns red, and feels like it’s on fire-no matter how gently you touch it-you’re not just having a bad day. You’re having a gout attack. It doesn’t come from lifting too much or twisting your ankle. It comes from something inside your blood that’s been building up for months, maybe years, without you noticing: uric acid.
What Exactly Is Uric Acid, and Why Does It Cause Pain?
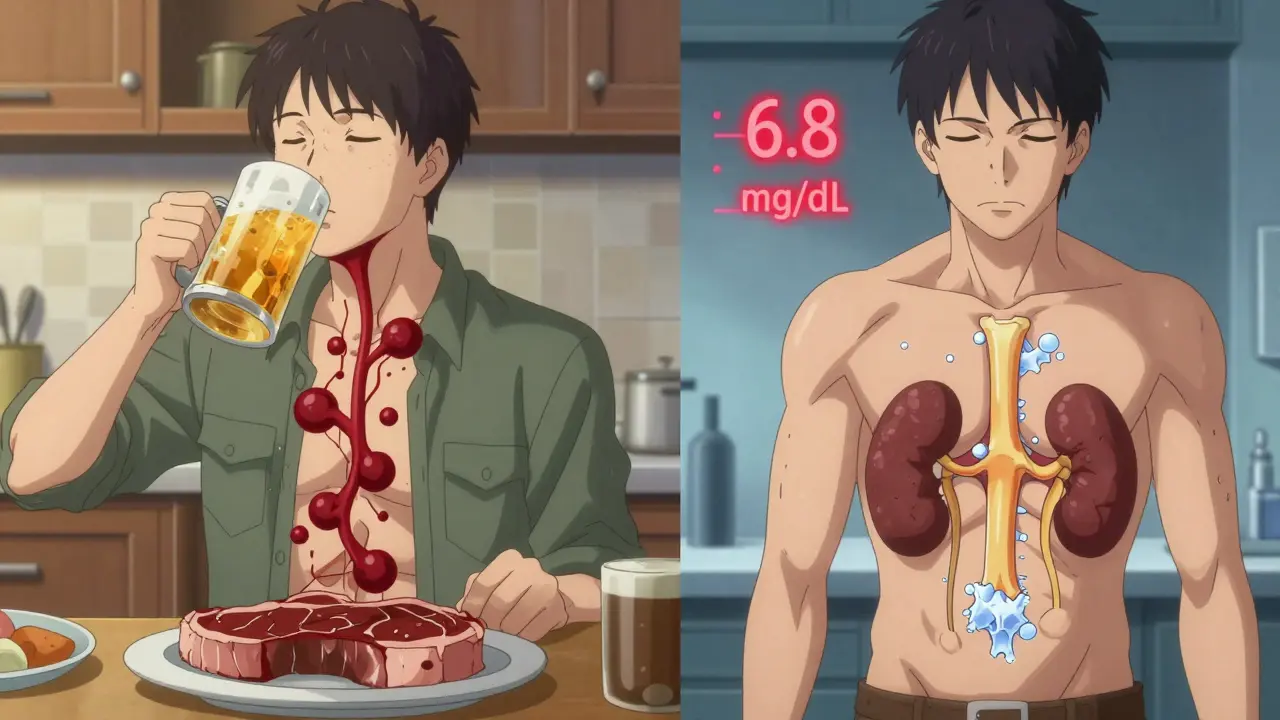
Uric acid isn’t a poison. It’s a natural waste product your body makes when breaking down purines-substances found in your cells and in certain foods. Most people’s kidneys flush it out easily. But if your body makes too much, or your kidneys can’t keep up, uric acid builds up. When it hits 6.8 mg/dL, it starts turning into sharp, needle-like crystals. These crystals don’t just sit there. They trigger your immune system like an alarm.
That alarm is called the NLRP3 inflammasome. It’s a protein complex in your white blood cells that goes into overdrive when it spots these crystals. It releases interleukin-1β, a powerful chemical that causes swelling, heat, and pain. That’s why your joint feels like it’s being stabbed from the inside. And here’s the twist: humans are one of the few mammals that can’t break down uric acid fully. We lost the enzyme that does it, evolutionarily speaking. That’s why gout is so common in people and not in dogs or cats.
Why Do Gout Attacks Happen Suddenly?
You might think a big steak or a beer last night caused the attack. But it’s rarely that simple. The real trigger is a sudden change in uric acid levels-not just high levels. That’s why people often get flares when they start taking allopurinol or febuxostat. Even lowering uric acid too fast can shake loose crystals stuck in your joints, causing inflammation. Same thing happens if you get dehydrated, injured your toe, or have surgery.
Other common triggers:
- Beer-not just because it’s alcohol, but because it’s packed with purines. One 12-ounce serving raises your risk by 49%.
- Fructose-sweetened drinks-soda, energy drinks, even fruit juices. Fructose forces your liver to make more uric acid.
- Red meat and organ meats-liver, kidney, sweetbreads. A 3-ounce serving can contain 300-500 mg of purines.
- Dehydration-if you’re not drinking at least 2 liters of water a day, your kidneys can’t flush uric acid properly.
- Medications-thiazide diuretics (water pills), low-dose aspirin, and even some chemotherapy drugs can raise uric acid.
And here’s something most people don’t know: gout flares often happen at night. That’s because your body temperature drops slightly while you sleep, making it easier for uric acid to crystallize. Also, you’re more dehydrated after hours without water.
How Do You Treat a Gout Attack?
When the pain hits, you need to calm the fire fast. There are three main options, and your doctor will pick based on your health history.
- NSAIDs-like indomethacin or naproxen. These reduce swelling and pain. Indomethacin is often prescribed at 50 mg three times a day for 3-5 days. But if you have kidney problems or stomach ulcers, this isn’t safe.
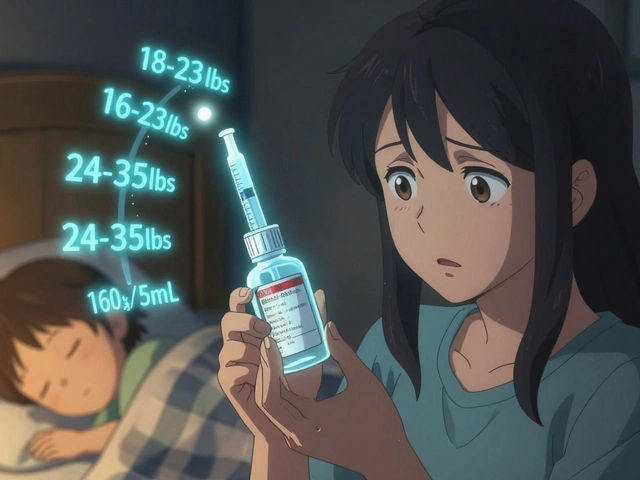
- Colchicine-a drug that blocks the immune response triggered by crystals. The standard dose is 0.6 mg three times a day for a few days. But it causes diarrhea in 10-20% of people. Lower doses (0.6 mg once or twice daily) work just as well with fewer side effects.
- Corticosteroids-like prednisone. If you can’t take NSAIDs or colchicine, your doctor might give you a 5-day course of 30-40 mg daily, then taper off. Steroid injections directly into the joint can also work wonders.
Important: Never stop your urate-lowering meds during a flare. That’s a common mistake. Stopping allopurinol won’t make the pain go away-it might make the next flare worse.
Long-Term Management: It’s Not About Pain, It’s About Uric Acid Levels
Most people think gout is a one-off problem. It’s not. Without treatment, attacks get more frequent, last longer, and damage your joints permanently. That’s why long-term management is non-negotiable.
The goal? Keep your blood uric acid below 6 mg/dL. For people with tophi (those visible lumps under the skin), aim for 5 mg/dL or lower. Why? Because below that level, crystals start dissolving. Research shows that after 12 months at 5 mg/dL, 70% of tophi disappear. At 6 mg/dL, only 30% do.
First-line drugs:
- Allopurinol-starts at 100 mg daily. Your doctor will increase it by 100 mg every few weeks until your target level is reached. Most people need 300-600 mg daily. Some need up to 800 mg. It’s cheap, effective, and works for most people.
- Febuxostat-if you can’t tolerate allopurinol. Usually 40-80 mg daily. More expensive, but good for those with kidney issues.
- Probenecid-helps your kidneys excrete more uric acid. Only works if your kidneys are still functioning well (GFR >50 mL/min). Not for people with kidney stones.
Here’s the catch: when you start these drugs, you’ll likely have more flares for the first 3-6 months. That’s because dissolving crystals stir things up. That’s why doctors now prescribe low-dose colchicine (0.6 mg once or twice daily) as a preventive during the first six months. Studies show this cuts flare risk by 50-75%.
Diet and Lifestyle: What Actually Helps?
Yes, diet matters-but not as much as medication. You can’t out-eat gout. But smart choices make treatment work better.
- Drink water-2-3 liters a day. Keeps your kidneys flushing uric acid.
- Choose low-fat dairy-milk, yogurt, cheese. One serving a day lowers risk by 43%. The exact reason isn’t clear, but it helps.
- Avoid beer and spirits-beer is the worst. Spirits are less risky than beer but still bad. Wine? Probably fine in moderation.
- Limit sugary drinks-even if they’re "natural" fruit juice.
- Eat more vegetables-even high-purine veggies like spinach or mushrooms don’t increase gout risk. Don’t avoid them.
- Maintain a healthy weight-losing 10% of your body weight can drop uric acid by 1-2 mg/dL.
And forget the old myth: you don’t need to go on a no-purine diet. It’s impossible and unnecessary. Just cut the worst offenders-organ meats, shellfish, and sugary drinks.
What Happens If You Ignore It?
Left untreated, gout doesn’t just hurt-it destroys. Over time, crystals form tophi: hard, chalky lumps under the skin, often on fingers, elbows, or ears. These can break through the skin and get infected. Joints become stiff, deformed, and permanently damaged. Your kidneys can get clogged with uric acid crystals too, leading to kidney stones or even kidney failure.
And here’s the scary part: if you stop your medication, your uric acid level rebounds in just 2-4 weeks. Flares come back. The cycle repeats. Gout isn’t something you "get over." It’s a chronic condition that needs lifelong management.

New Hope: What’s on the Horizon?
Research is moving fast. In 2023, trials showed a new drug called dapansutrile-designed to block the NLRP3 inflammasome-cut gout flare duration by 40% compared to placebo. This is the first treatment that targets the actual cause of pain, not just the symptoms.
Scientists are also looking at gut bacteria. Early studies suggest certain probiotics may help break down purines in the intestines, lowering uric acid by 10-15%. It’s early, but promising.
For now, the best strategy remains simple: lower uric acid, keep it low, and protect your joints. The tools are here. The science is clear. You just need to stick with it.
Frequently Asked Questions
Can gout be cured?
No, gout can’t be cured-but it can be fully controlled. With consistent urate-lowering therapy and lifestyle changes, most people stop having flares entirely. Tophi can disappear, joint damage can halt, and you can live without pain. The key is lifelong management, not temporary fixes.
Why does my gout flare up even when I’m taking medication?
When you start a urate-lowering drug like allopurinol, your body begins dissolving old crystals. That process irritates your joints and triggers inflammation. That’s why doctors prescribe low-dose colchicine for the first 6 months-it prevents these flares. It’s not the medication failing; it’s part of the healing process.
Is it safe to drink alcohol if I have gout?
Beer is the worst offender-it raises your risk by nearly 50% per daily serving. Spirits are less risky but still not safe. Wine in moderation (one glass) doesn’t seem to trigger flares in most people. But if you’re still having attacks, cutting alcohol entirely is the safest move. Alcohol slows down uric acid excretion and adds purines.
Do I need to stop eating meat altogether?
No. You don’t need to go vegetarian. Avoid organ meats (liver, kidney, sweetbreads) and shellfish like shrimp and mussels. Red meat in small portions (once or twice a week) is usually fine. Focus more on cutting beer, sugary drinks, and excess weight. Vegetables-even those high in purines-are safe and helpful.
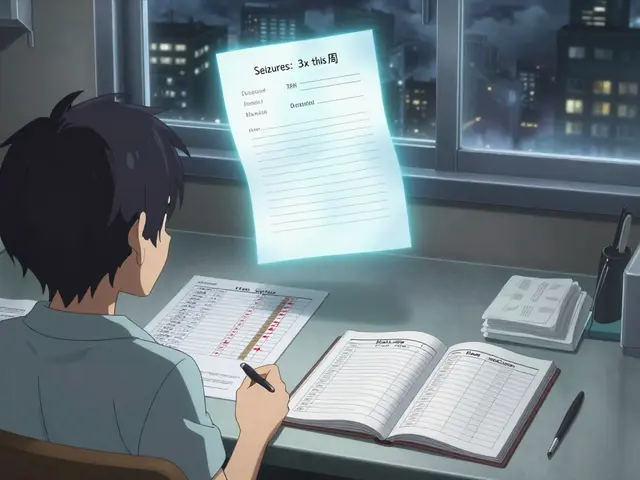
How often should I get my uric acid tested?
When starting or adjusting medication, test every 2-5 weeks until your level is below 6 mg/dL. Once stable, check every 6 months. If you miss a dose or feel a flare coming, get tested sooner. Uric acid levels can swing fast, and your treatment needs to keep up.
What to Do Next
If you’ve had one gout attack, don’t wait for the next. Talk to your doctor about starting urate-lowering therapy-even if you’re pain-free now. The goal isn’t to stop the pain today; it’s to stop the damage tomorrow.
Write down your triggers: What did you eat? Did you drink? Were you stressed or dehydrated? Bring that list to your appointment. Keep a journal. Track your uric acid levels. Stick to your meds-even when you feel fine.
Gout isn’t a punishment. It’s a signal. Listen to it. Manage it. And take back control of your joints.




Comments
So let me get this straight - I’ve been blaming my late-night tacos for the pain, but it’s actually my body’s ancient evolutionary glitch? Thanks for making me feel like a biological mistake. Also, I just drank a soda and now I’m terrified. 😅
Uric acid is a sign of weak discipline. If you ate clean and drank water like a normal person, you wouldn’t be here. This isn’t medicine - it’s a lifestyle failure.
Colchicine gives you diarrhea so you stop drinking beer. That’s not treatment. That’s punishment disguised as science.
Bro. Uric acid crystals are basically tiny angry gods screaming inside your joint. And your body’s immune system? It’s like a toddler with a flamethrower trying to fight them. We lost the enzyme to break it down because evolution said ‘nah, let them suffer, it’ll teach them to stop eating liver.’ 🙃
But then we made allopurinol and now we’re playing god with our own biochemistry. I’m not mad. I’m just... profoundly confused.
And also - why does this happen at night? Because the universe hates us and wants us to wake up screaming into the void. It’s not a disease. It’s a cosmic joke.
Low-dose colchicine is the quiet hero here. The unsung Gandalf of gout. You don’t see him, but he’s holding the line.
And yes, I cried when I read that tophi can disappear. I’m not ashamed.
It is scientifically documented that the consumption of fructose-sweetened beverages in the United States correlates directly with the increased prevalence of gout among the population. This is not a medical condition - it is a systemic failure of public health policy. I recommend immediate legislative intervention to regulate high-fructose corn syrup in all nonessential food products.
hey i had gout last year and i just started drinking more water and eating more bananas and it got better lol i know its not science but i felt way better after that
So let me get this straight - you’re telling me I can’t blame my 3am pizza anymore? That’s not a trigger, that’s just a ‘convenient coincidence’? Thanks for ruining my favorite excuse.
Allopurinol is just Big Pharma’s way of monetizing human biology. If we hadn’t evolved to lose uricase, we wouldn’t need this. The real solution? Go back to being a hunter-gatherer. Or at least stop eating processed food. But no, let’s just keep selling pills.