Probiotic Timing Calculator
Optimal Probiotic Timing
Recommended probiotic timing based on medical research:
Take probiotics 2-3 hours after your antibiotic dose
Why this matters:
Antibiotics can kill probiotic bacteria if taken simultaneously. Spacing them out by 2-3 hours ensures the probiotics survive to reach your gut and help restore balance.
Important Note: For best results, take probiotics with 5-10 billion CFUs daily for 1-2 weeks after antibiotics.
Key Takeaways
When you’re on antibiotics, your body isn’t just fighting an infection-it’s also losing billions of good bacteria in your gut. This isn’t just a side note. It’s why so many people end up with stomach cramps, bloating, or worse-diarrhea that lasts days or even weeks. About 1 in 5 people on antibiotics get antibiotic-associated diarrhea. For some, it’s mild. For others, it’s a dangerous infection like Clostridioides difficile (C. diff), which can land you in the hospital. But there’s a simple, widely studied way to cut that risk: probiotics.
What Happens to Your Gut When You Take Antibiotics?
Antibiotics don’t pick and choose. They wipe out the bad bacteria causing your infection-and the good ones that help you digest food, make vitamins, and keep your immune system in check. Your gut is home to over 100 trillion bacteria. When antibiotics hit, it’s like a wildfire through a forest. The good bugs get burned along with the bad. That’s when symptoms show up. Diarrhea is the most common, but bloating, gas, cramps, and nausea follow close behind. These aren’t just annoying-they can make you skip doses, delay recovery, or even lead to a more serious infection. C. diff, for example, thrives when the normal gut flora is gone. It’s not rare: up to 35% of hospitalized patients on antibiotics develop it.How Do Probiotics Help?
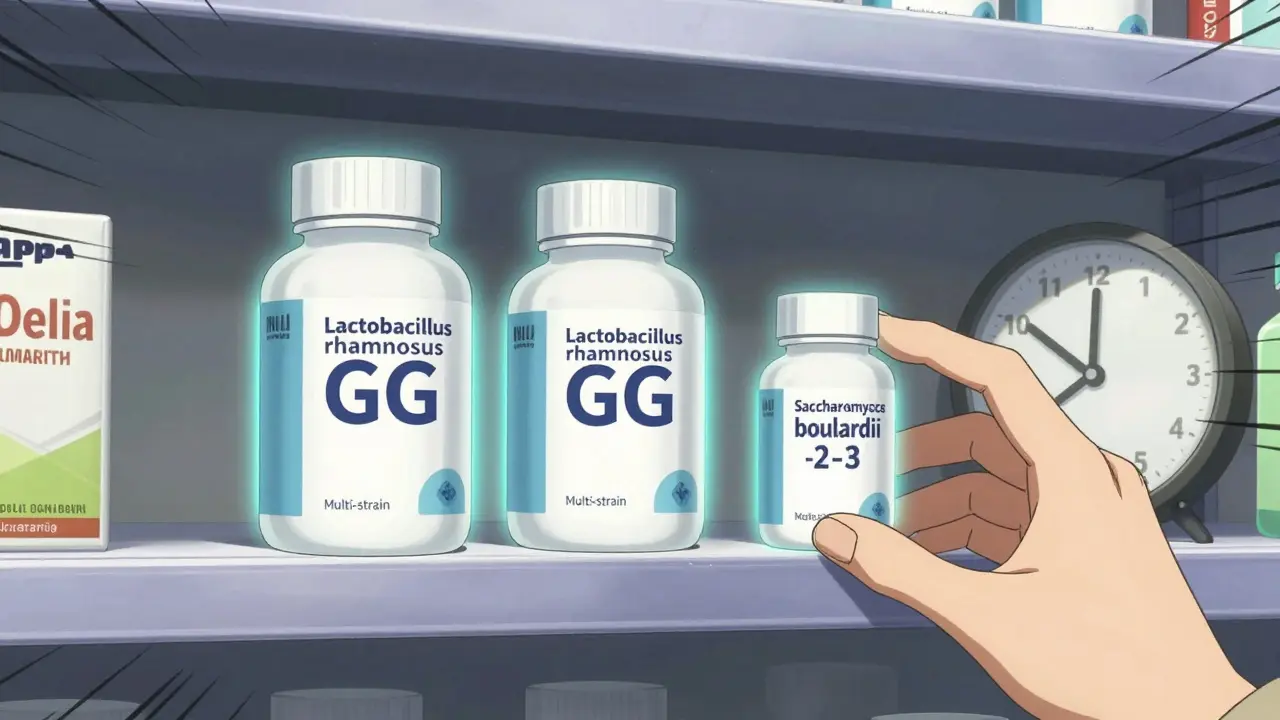
Probiotics are live microorganisms-mostly bacteria or yeast-that help restore balance. They don’t replace your original gut bugs, but they act like temporary reinforcements. Strains like Lactobacillus rhamnosus GG and Saccharomyces boulardii have been studied the most. In high-risk patients, probiotics cut the chance of C. diff diarrhea from 11.6% down to 3.1%. That’s a 73% drop. They work by competing with bad bacteria for space and food, producing acids that make the gut less friendly to pathogens, and strengthening the gut lining. Some even help your body make short-chain fatty acids, which calm inflammation. You don’t need to take them forever. Just during and for a week or two after your antibiotic course.Which Probiotics Actually Work?
Not all probiotics are created equal. The strain matters more than the brand. Here’s what the evidence shows:- Saccharomyces boulardii (a yeast): Reduces antibiotic diarrhea risk by about 50%. Works well even with strong antibiotics like clindamycin.
- Lactobacillus rhamnosus GG: One of the most researched strains. Proven to reduce diarrhea in both kids and adults.
- Multi-strain blends: Often contain L. acidophilus, Bifidobacterium, and others. Mixed results, but some studies show benefit, especially if they include GG or S. boulardii.
How and When to Take Them
Timing is everything. Antibiotics can kill probiotics if you take them at the same time. The fix? Space them out.- Take your probiotic 2 to 3 hours after your antibiotic dose.
- Some experts say take it with food to protect the microbes from stomach acid. Others say empty stomach is better for acid-resistant strains like S. boulardii.
- Stick to a daily dose-no skipping days. Most studies use 5 to 10 billion CFUs (colony-forming units) per day.
- Keep taking probiotics for at least 1 to 2 weeks after finishing antibiotics. Your gut needs time to rebuild.
What You Might Experience at First
When you start, you might feel more bloated or gassy. That’s normal. Your gut is adjusting. These symptoms usually fade in a few days. If they get worse, or you develop constipation, try lowering the dose or switching strains. Some people with IBS or sensitive guts report flare-ups. That’s not a sign the probiotic isn’t working-it might mean you’re using the wrong strain. S. boulardii tends to be gentler than some bacterial strains for sensitive individuals.The Big Problem: Not All Products Are Created Equal
Here’s the ugly truth: most probiotics sold in the U.S. are classified as dietary supplements. That means the FDA doesn’t require manufacturers to prove they work or even contain what’s on the label. Independent testing found:- 30% of probiotic supplements didn’t have the number of live organisms advertised.
- 15% contained microbes not listed at all-some even harmful.
- List the exact strain (e.g., Lactobacillus rhamnosus GG, not just “Lactobacillus”)
- Provide the CFU count at expiration, not just at manufacture
- Have third-party testing seals (like USP, NSF, or ConsumerLab)

Who Should Avoid Probiotics?
They’re safe for most people-but not everyone. If you have:- A weakened immune system (from chemo, HIV, or steroids)
- Been recently hospitalized or had major surgery
- Are critically ill or have a central line
What About Long-Term Gut Recovery?
Some recent studies suggest probiotics might actually slow down your gut’s natural recovery after antibiotics. One 2021 study in Nature found that people who took probiotics took longer to return to their original microbiome than those who didn’t. Their gut bacteria were still out of balance months later. This doesn’t mean you shouldn’t take them. It means the goal isn’t to “repopulate” your gut with the same bugs you had before. It’s to prevent harm while your body heals. The evidence still strongly supports using probiotics to avoid diarrhea and C. diff-especially during treatment.Bottom Line: What to Do
If you’re on antibiotics and want to avoid stomach trouble:- Choose a probiotic with L. rhamnosus GG or S. boulardii.
- Take it 2-3 hours after your antibiotic, daily.
- Use 5-10 billion CFUs per day.
- Continue for 1-2 weeks after finishing antibiotics.
- Check the label: strain name, CFU count, expiration date.
- Stop and call your doctor if you’re immunocompromised or symptoms worsen.
Can I get enough probiotics from yogurt instead of supplements?
Most yogurts contain far fewer live bacteria than what’s needed to help with antibiotic side effects-usually under 1 billion CFUs. They also rarely include the specific strains proven to work, like L. rhamnosus GG or S. boulardii. Supplements give you a targeted, reliable dose. Yogurt is fine for general gut health, but not enough for antibiotic support.
Do probiotics interfere with antibiotics?
Not if you take them at the right time. Taking probiotics and antibiotics together can kill the probiotics before they reach your gut. Spacing them 2-3 hours apart prevents this. Studies show this timing doesn’t reduce how well the antibiotic works.
How long should I take probiotics after finishing antibiotics?
Continue for at least 1 to 2 weeks after your last antibiotic dose. Your gut microbiome needs time to recover, and probiotics help prevent late-onset diarrhea. Some people keep taking them longer for general gut health, but that’s optional.
Are there any side effects from taking probiotics?
The most common are temporary bloating, gas, or increased thirst-usually gone within a few days. In rare cases, people with weakened immune systems can develop serious infections. If you feel worse after starting, stop and talk to your doctor.
Why do some people say probiotics didn’t work for them?
It’s often because they used the wrong strain, didn’t take enough, or took them at the same time as antibiotics. Some products are also low-quality and don’t contain live organisms. Stick to well-researched strains like L. rhamnosus GG or S. boulardii, and check the label for live CFUs at expiration.






Comments
Okay but can we just take a second to appreciate how wild it is that we’re still figuring out how to coexist with the trillions of tiny organisms living in our guts? Like, we send probes to Mars but we’re still learning that yogurt isn’t a magic fix. Probiotics aren’t a cure-all, but skipping them when you’re on antibiotics is like bringing a water gun to a wildfire. I took Culturelle with my clindamycin last year and barely had a hiccup. My gut thanked me.
I’ve been recommending S. boulardii to my patients for years. It’s yeast, not bacteria, so antibiotics don’t kill it. That’s the whole advantage. And yes, timing matters - take it two hours after the antibiotic, not with breakfast. I’ve seen people get diarrhea even with probiotics because they took them together. It’s not the probiotic’s fault. It’s the timing.
This whole probiotic thing is a scam pushed by supplement companies. Your gut fixes itself. You don’t need to buy $30 bottles of powder just to poop normally. I’ve taken six rounds of antibiotics in the last five years and never used probiotics. Never had C. diff. Stop fearmongering with percentages and just let your body work.
Wait - so you’re telling me to spend money on supplements because some study says ‘73% drop’? But then you admit in the next section that probiotics might actually delay your gut’s natural recovery? So are we helping or hurting? Why does every article like this sound like a sales page for Culturelle? Also, why is no one talking about fecal transplants? They’re way more effective and way cheaper. Just saying.
LOL at the ‘30% don’t have the CFUs advertised’ stat. That’s the whole point of supplements bro. They’re unregulated. You think the FDA gives a damn? They’re too busy banning glitter and regulating CBD gummies. And why are we still pretending ‘L. rhamnosus GG’ is some miracle strain? It’s just the most marketed one. I’ve seen 12 different studies with conflicting results. This isn’t science - it’s marketing with a lab coat.
Look, I get it - Western medicine loves selling you pills to fix problems it created. Antibiotics wipe out your gut, then we sell you probiotics to fix it? That’s like burning down your house and then selling you a new carpet. In India, we’ve been using fermented foods for centuries - curd, kanji, idli batter - no fancy supplements needed. People here don’t get C. diff because they eat real food, not lab-made powders. This whole ‘take a capsule after antibiotics’ thing is a Western overcomplication. Your ancestors survived without Culturelle. So can you.
And don’t get me started on the ‘third-party tested’ nonsense. USP? NSF? Those are just logos slapped on bottles by companies who pay for the seal. I’ve seen Indian brands with 100 billion CFUs and no testing, and they work better than half the Amazon junk. Stop trusting labels. Trust tradition. Trust your gut.
Also, why is everyone obsessed with ‘strain names’? Who the hell remembers Lactobacillus rhamnosus GG? My grandmother just ate yogurt with a pinch of black salt and called it a day. She lived to 92. No probiotic bottles. No CFUs. Just food. Maybe we’re overengineering this whole thing because we’ve lost touch with simple things.
And let’s be real - if you’re so worried about C. diff, maybe don’t take antibiotics unless you absolutely need them. That’s the real solution. Not buying a $25 bottle of pills. Stop treating your body like a broken machine that needs a software update. It’s a living system. Let it breathe.
Also, I’m tired of people acting like yogurt is useless. In India, we make homemade yogurt with 10x the live cultures of store-bought stuff. You don’t need a supplement. You need a jar, some milk, and patience. That’s not ‘alternative medicine.’ That’s wisdom.
And for the love of God, stop calling it ‘gut health.’ That’s a marketing term. It’s your microbiome. Your ecosystem. Your inner jungle. Stop talking like you’re at a Whole Foods checkout.
Probiotics might help some people. But don’t make it a religion. And for the love of all that’s holy, don’t buy anything that doesn’t say ‘made in India’ on the bottle.
Just want to say that if you’re immunocompromised, don’t take probiotics without talking to your doctor. I had a patient on chemo who developed fungemia from Saccharomyces boulardii. It was rare, but it happened. The risk is low for most, but not zero. Always check with your care team.
As someone from Nigeria, I’ve seen people use fermented millet drinks and pap during antibiotic courses. No pills. Just food. Works fine. Maybe the real issue isn’t probiotics - it’s that we’ve forgotten how to eat. The West overcomplicates everything. Simple, local, fermented foods have been the answer for millennia. Why are we chasing lab-made capsules when our grandmothers knew better?
I took probiotics with my antibiotics and felt way better. No diarrhea, no bloating. Just a small daily capsule. I didn’t even think about it until now. But I’m so glad I did. It’s like giving your gut a little hug while the antibiotics do their job. No magic, just smart support.
Bro probiotics are just fancy yogurt. I took them once and felt like a balloon. Waste of money. Just drink kefir if you wanna be healthy. No cap.
Thank you for the clear, evidence-based summary. Many people don’t realize that strain specificity matters - and that timing is critical. I’ve shared this with my patients and they’ve reported fewer GI issues. Also, the note about label transparency is essential. Not all products are created equal. This is exactly the kind of information we need in public health communication.