Medication Arrhythmia Risk Checker
Check if your medications may increase risk of heart rhythm problems. This tool identifies medications that may cause arrhythmias based on published medical evidence.
Add Your Medications
Risk Assessment
When you take a pill to treat one problem, you don’t expect it to cause another-especially not something as serious as an irregular heartbeat. But the truth is, medication-induced arrhythmias are more common than most people realize. Over 400 widely used drugs, from antibiotics to antidepressants, can mess with your heart’s rhythm. Some of these reactions are mild, like a flutter you feel in your chest. Others can be life-threatening, leading to emergency hospital visits or even sudden cardiac arrest.
What Exactly Is a Drug-Induced Arrhythmia?
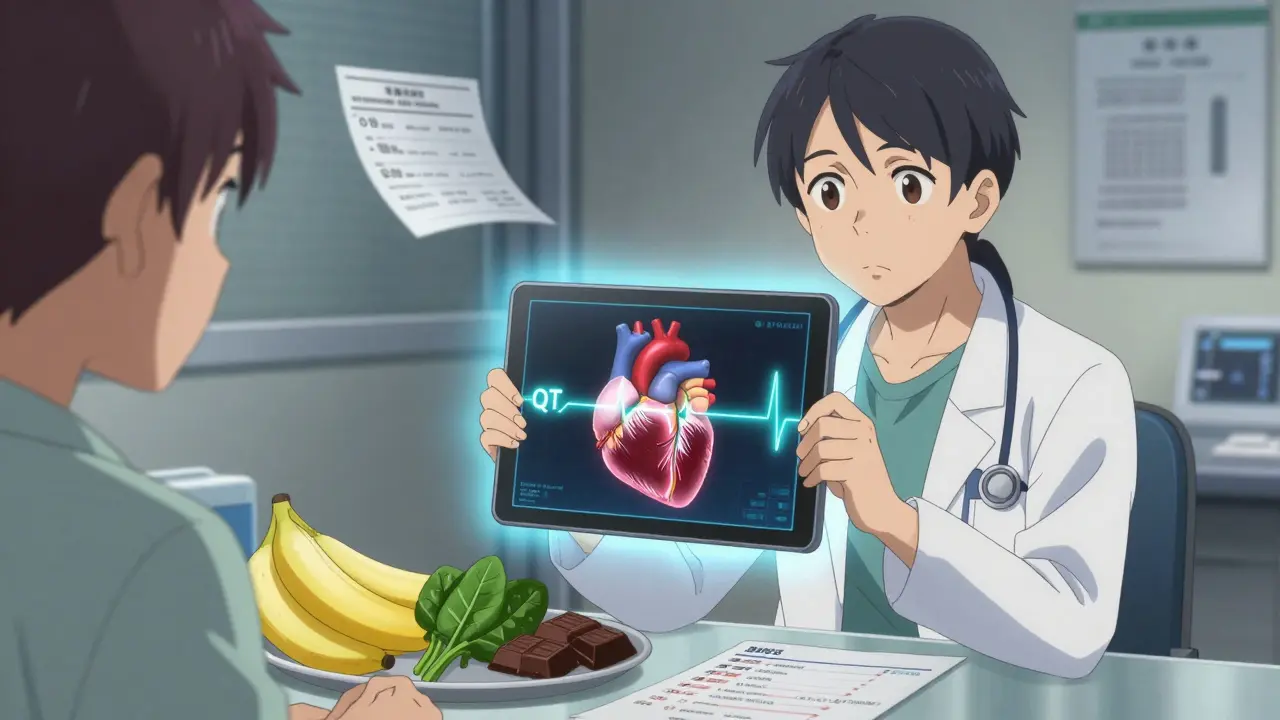
An arrhythmia is when your heart beats too fast, too slow, or irregularly. When it’s caused by a medication, it’s called a drug-induced arrhythmia. This isn’t rare. In fact, about 3-5% of all arrhythmia cases that land people in the emergency room come from medications. These aren’t just side effects you might read about in a leaflet-they’re real, measurable risks backed by decades of clinical data. The most dangerous type is QT prolongation. That’s when the electrical cycle of your heart takes longer than normal to reset between beats. This delay can trigger a wild, chaotic rhythm called torsades de pointes, which can turn into ventricular fibrillation-a condition that stops your heart from pumping blood. It’s not theoretical. Since 2010, the FDA has added black box warnings to 25 medications for this exact reason, with eight added just in 2022.Which Medications Are Most Likely to Cause Problems?
Some drugs are known culprits. Here’s a breakdown of the most common offenders and how they affect your heart:- Antibiotics: Macrolides like azithromycin and fluoroquinolones like levofloxacin can prolong the QT interval in 3-5% of users, especially in the first week of use.
- Antidepressants and antipsychotics: Medications like citalopram, escitalopram, and haloperidol carry significant risk. Together, they account for 22-33% of all medication-related arrhythmias.
- Antiarrhythmics themselves: Ironically, drugs meant to fix heart rhythms-like flecainide, propafenone, and amiodarone-can make them worse. Flecainide can turn atrial flutter into a dangerous 1:1 conduction pattern. Amiodarone, while effective, can cause atrial fibrillation in 2-5% of patients by triggering thyroid dysfunction.
- Digoxin: Used for heart failure and atrial fibrillation, digoxin toxicity (serum levels above 2 ng/mL) leads to paroxysmal atrial tachycardia with block in about 1% of users. Risk spikes if you have kidney disease or low magnesium.
- Anticancer drugs: Trastuzumab (Herceptin) can cause atrial fibrillation in 2-5% of patients by increasing inflammation and oxidative stress in heart cells.
- Beta-blockers: While they’re used to slow the heart, too much can cause dangerously low heart rates. Symptoms include fatigue, dizziness, and fainting. About 10-15% of patients on beta-blockers for atrial fibrillation end up needing a pacemaker because their heart can’t keep up even at low doses.
Who’s at Highest Risk?
Not everyone who takes these drugs will have a problem. But certain people are far more vulnerable:- Age 65 and older: Sixty to seventy percent of severe cases occur in seniors. Aging hearts are less resilient, and older adults often take multiple medications.
- Electrolyte imbalances: Low potassium (hypokalemia) affects 20% of hospitalized patients. Low magnesium (hypomagnesemia) hits 10-15%. Both make the heart electrically unstable.
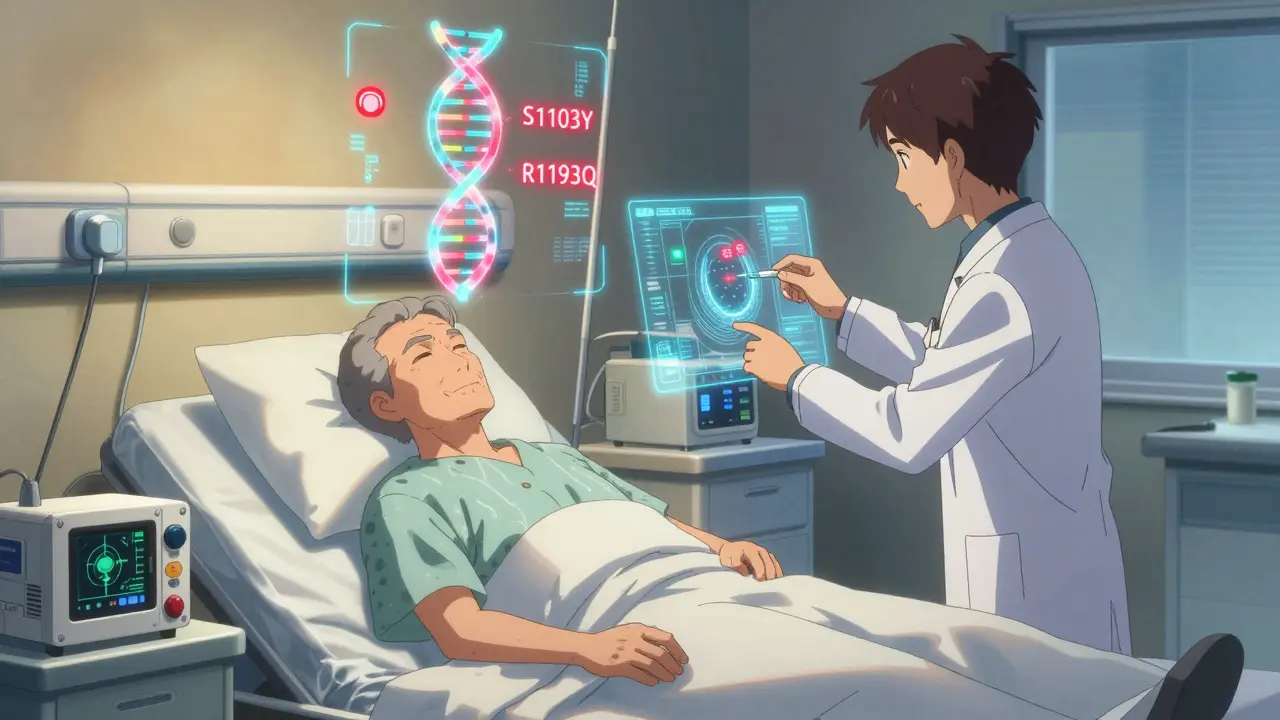
- Genetic factors: About 15% of people of African ancestry carry the S1103Y variant. Around 12% of East Asians carry R1193Q. These gene variants make heart cells much more sensitive to QT-prolonging drugs-even at normal doses.
- Multiple drugs at once: Taking two or more QT-prolonging medications increases risk by 300-500%. A common combo? An antibiotic plus an antidepressant. It sounds harmless, but it’s a ticking time bomb.
- Excessive alcohol: More than three drinks a day triples your risk. Alcohol directly affects ion channels and depletes magnesium.
Warning Signs You Can’t Ignore
Most people don’t realize their heart is out of rhythm until it’s too late. But there are clear signals-if you know what to look for:- Palpitations: A racing, pounding, or fluttering sensation in your chest. Reported by 70-80% of patients.
- Dizziness or lightheadedness: Especially when standing up. This isn’t just “getting old”-it’s your brain not getting enough blood.
- Fatigue: Constant tiredness that doesn’t improve with rest. Often mistaken for stress or depression.
- Chest discomfort: Not always a sharp pain. Sometimes it’s pressure, fullness, or just “something feels off.”
- Fainting or near-fainting: Syncope is the reddest of red flags. If you’ve passed out, even briefly, get checked immediately.
How Doctors Manage These Cases
The good news? Most cases can be reversed if caught early. Here’s what typically happens:- Stop or adjust the drug: In 75-85% of cases, simply changing the dose or switching to a safer alternative resolves the issue. For example, switching from citalopram to sertraline can eliminate QT risk.
- Correct electrolytes: If potassium is below 4.0 mEq/L or magnesium below 2.0 mg/dL, doctors give supplements. Simple, cheap, and often lifesaving.
- ECG monitoring: Before starting high-risk drugs, a baseline ECG is required. A second ECG is done within 72 hours. If the QT interval extends beyond 500 milliseconds or increases by more than 60 ms from baseline, the drug is stopped.
- Pacemakers or ablation: For patients with severe bradycardia from beta-blockers, a pacemaker may be implanted so they can keep taking the drug safely. Catheter ablation is needed in 5-10% of persistent cases.
- Surgery: Required in less than 2% of cases-usually only when other options fail and the arrhythmia is life-threatening.
What You Can Do to Protect Yourself
You don’t have to wait for a crisis. Here’s how to stay safe:- Know your meds: Ask your pharmacist or doctor: “Could this cause an irregular heartbeat?” Keep a list of all your medications-including over-the-counter ones like antihistamines (e.g., diphenhydramine) and cold remedies.
- Get tested: If you’re prescribed a high-risk drug, ask if a baseline ECG is recommended. If you have a family history of sudden cardiac death or unexplained fainting, genetic testing for S1103Y or R1193Q may be worth considering.
- Watch your diet: Eat potassium-rich foods (bananas, spinach, sweet potatoes) and magnesium-rich foods (nuts, seeds, dark chocolate). Avoid excessive salt and processed foods that deplete electrolytes.
- Limit alcohol and caffeine: More than three drinks a day doubles your risk. Even one cup of strong coffee can trigger palpitations in sensitive people.
- Don’t self-medicate: Combining herbal supplements like St. John’s Wort with antidepressants can spike serotonin and trigger arrhythmias. Always tell your doctor what you’re taking.
The Future: Personalized Medicine Is Here
The days of one-size-fits-all prescriptions are fading. Researchers at Vanderbilt and elsewhere are already using CRISPR-edited heart cells to test how individual genes react to drugs. In 2024, the American College of Cardiology is rolling out a clinical tool that calculates your personal arrhythmia risk based on your age, meds, electrolytes, and genetic profile. Soon, before you’re prescribed a drug like azithromycin or citalopram, your doctor might run a quick genetic screen. If you carry the S1103Y variant, they’ll choose a different antibiotic. That’s not science fiction-it’s already happening in top hospitals.Bottom Line
Medications save lives-but they can also stop them. Drug-induced arrhythmias are preventable. You don’t need to avoid treatment. You just need to be informed. If you’re on a long-term medication and feel off, don’t brush it off. Track your symptoms. Know your numbers. Ask the right questions. Your heart is counting on it.Can over-the-counter drugs cause heart arrhythmias?
Yes. Many common OTC meds can trigger arrhythmias. Antihistamines like diphenhydramine (Benadryl), decongestants like pseudoephedrine, and even some cough syrups containing dextromethorphan can prolong the QT interval. People with existing heart conditions or those taking other medications are especially at risk. Always check labels and ask your pharmacist before using these products.
Is it safe to take antibiotics if I have a history of heart rhythm problems?
It depends. Macrolides like azithromycin and fluoroquinolones like levofloxacin carry known risks. If you’ve had arrhythmias before, your doctor should avoid these unless absolutely necessary. Safer alternatives like amoxicillin or doxycycline are often preferred. Always tell your provider about your heart history before starting any new antibiotic.
How long does it take for a drug-induced arrhythmia to go away?
In most cases, stopping the drug leads to improvement within 24 to 72 hours. QT prolongation usually resolves once the medication is cleared from your system. But if the arrhythmia has triggered structural changes or if electrolytes are severely low, recovery may take longer-up to a week or more. Persistent cases require further evaluation and possibly a pacemaker or ablation.
Can caffeine cause dangerous arrhythmias?
Caffeine alone rarely causes life-threatening arrhythmias. However, 25-30% of people with heart rhythm issues report that caffeine triggers palpitations. For those with underlying conditions or who consume large amounts (5+ cups of coffee a day), it can worsen existing arrhythmias. Moderation is key-limiting intake to 2-3 cups daily is generally safe for most people.
Should I get genetic testing before taking heart medications?
Routine genetic testing isn’t standard yet, but it’s becoming more common in high-risk cases. If you’re prescribed a QT-prolonging drug and have a personal or family history of unexplained fainting, sudden cardiac death, or arrhythmias, ask your doctor about testing for S1103Y or R1193Q variants. These tests are becoming faster and cheaper, and they can prevent serious complications.







Comments
Really well-researched breakdown. I’ve been on escitalopram for years and never knew it could mess with my QT interval. I’ll ask my cardiologist for a baseline ECG next visit. Good to see the stats on electrolytes too-my magnesium’s been low since I started diuretics for blood pressure. Small tweaks, big impact.
The data here is selectively curated to scare people into avoiding medications. Yes, QT prolongation exists-but so does the placebo effect, and no one tracks how many people panic and stop life-saving drugs because of fear-mongering like this. The real risk is overtreatment and unnecessary ECGs that clog up ERs. Don’t confuse statistical correlation with clinical necessity.
You people are too trusting of pharmaceuticals. The FDA only added those black box warnings because they were forced to-after decades of cover-ups. Amiodarone? It’s basically chemical warfare on your thyroid. And digoxin? That’s a plant toxin from foxglove they’ve been selling since the 1700s. If your heart’s beating wrong, maybe it’s not the meds-it’s your body screaming you’ve been poisoned by corporate medicine.
They don’t want you to know that potassium from bananas works better than a pacemaker. They want you dependent. Ask yourself: who profits when you need a device implanted every five years?
Okay but like… why does every single article about heart stuff now sound like a medical textbook written by a robot? 🤡 I get it, QT prolongation is a thing. But can we just say ‘some meds can mess with your heart’ and leave it at that? Also, I just took Benadryl for allergies and now I’m paranoid I’m gonna drop dead. Thanks, internet.
As someone who works in rural primary care in the Midwest, I see this daily. Elderly patients on five meds, no regular labs, no ECGs, and they’re told to ‘just keep taking it.’ The real issue isn’t the drugs-it’s the lack of follow-up. We don’t have the resources to screen everyone, but we could do so much more with basic electrolyte checks and simple ECGs at refill time. It’s not rocket science-it’s basic care.
And yes, St. John’s Wort with SSRIs? That’s a recipe for disaster. I’ve seen it twice. Always ask about supplements. Always.
bro i took azithromycin last year and felt like my heart was trying to escape my chest for 3 days. i thought i was dying. i went to the er and they just laughed and said ‘it’s the antibiotic.’ i left with a $2000 bill and zero answers. now i refuse all antibiotics unless i’m literally choking. this is why people don’t trust doctors. they don’t listen.
u ever think the gov is using these meds to control the population? 3-5% of arrhythmias from drugs? that’s not a side effect, that’s a feature. they want us weak, dependent, and hooked on pacemakers. look at the pharma ads on tv-always happy old people with pills. they’re not healing u, they’re programming u. and the gene thing? s1103y? that’s a bioweapon for black people. i read it on a forum. it’s real.
Wow. So we’re supposed to be terrified of every pill we take, but also not take anything because ‘it might kill you’? And yet somehow, people are living longer than ever. Maybe the real problem isn’t the meds-it’s the anxiety about meds. I’ll take my sertraline, thank you very much. And yes, I eat bananas. And yes, I asked my doctor. And no, I’m not Googling symptoms at 2 a.m. anymore.