Warfarin-Antibiotic Interaction Checker
Antibiotic Interaction Checker
When you're on warfarin, even a simple antibiotic can throw your blood thinning off balance. It’s not rare - about one in five people taking warfarin will need an antibiotic at some point. And when that happens, your INR can spike unexpectedly, raising your risk of dangerous bleeding. Or, in some cases, it can drop, leaving you vulnerable to clots. The truth? You don’t have to avoid antibiotics. But you do need to know which ones are risky, how to monitor for problems, and what to do when things go sideways.
Why Warfarin and Antibiotics Don’t Always Get Along
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. It’s a tightrope walk: too little, and you clot; too much, and you bleed. The problem with antibiotics isn’t that they’re dangerous by themselves - it’s that they mess with your body’s ability to handle warfarin in three different ways. First, some antibiotics shut down the liver enzyme CYP2C9. This enzyme breaks down the most powerful part of warfarin (called S-warfarin). When it’s blocked, warfarin builds up in your blood. Drugs like trimethoprim-sulfamethoxazole (Bactrim), ciprofloxacin, and erythromycin do this strongly. Second, antibiotics wipe out good bacteria in your gut. These bacteria make about 10-15% of your vitamin K. Less vitamin K means warfarin works even harder - your INR climbs. This happens with almost all broad-spectrum antibiotics, especially cephalosporins like ceftriaxone. Third, some antibiotics compete with warfarin for binding to albumin, a protein in your blood. This temporarily frees up more warfarin, giving you a quick but short-lived spike in anticoagulation.Which Antibiotics Are Most Dangerous?
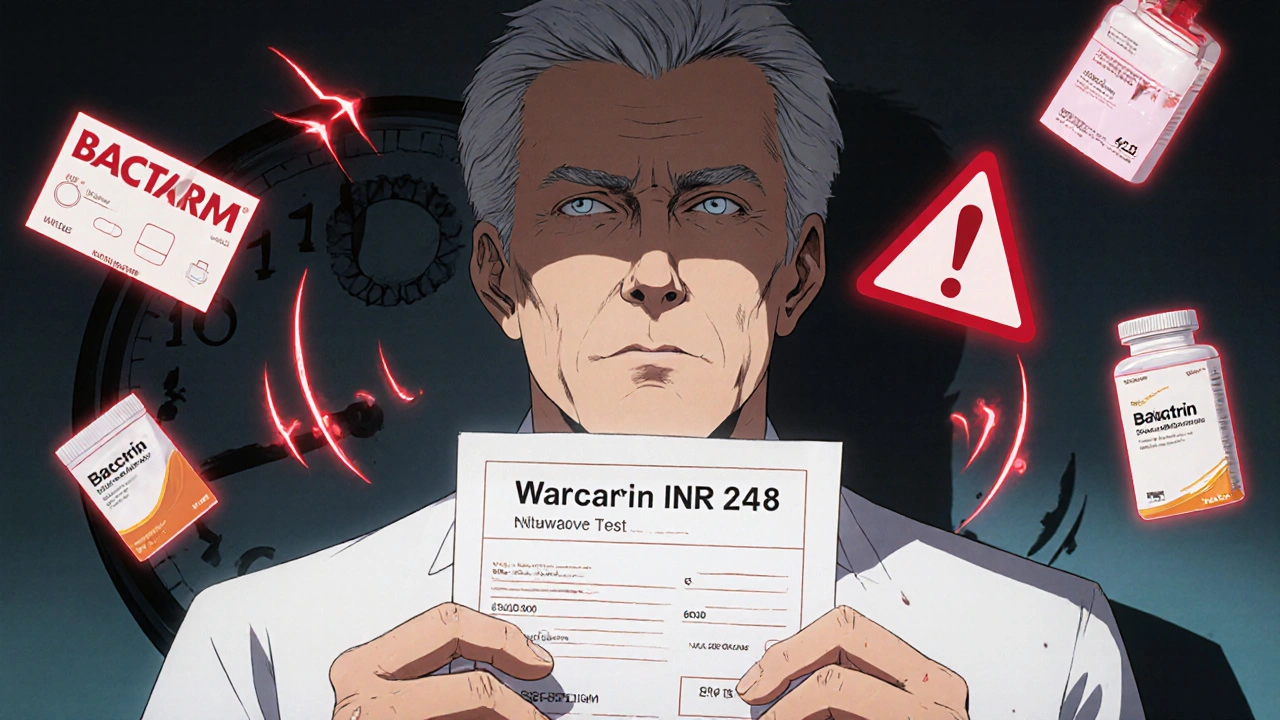
Not all antibiotics are created equal when you’re on warfarin. Some are low-risk. Others are red flags.- High-risk: Trimethoprim-sulfamethoxazole (Bactrim, Septra) is the biggest concern. Studies show it can raise your INR by 1.5 to 3 units in just a few days. Fluconazole (an antifungal, not an antibiotic, but often grouped here) does the same. For many patients, starting Bactrim means cutting your warfarin dose by 25-50% - sometimes even skipping a dose.
- Moderate-risk: Fluoroquinolones (ciprofloxacin, levofloxacin), macrolides (erythromycin, clarithromycin), and penicillins (amoxicillin, ampicillin) can raise INR by 0.5 to 1.5 units. You’ll likely need a small dose reduction and close monitoring.
- Low-risk: Clindamycin and azithromycin are much safer. Clindamycin barely affects warfarin - it’s often the go-to for dental work in people on blood thinners. Azithromycin has almost no enzyme interference.
- The exception: Rifampin does the opposite. It speeds up warfarin breakdown. Your INR will drop, and you might need to increase your warfarin dose by 50% or more. This effect takes weeks to stabilize.
It’s not just about the drug name. Dose, duration, and your age matter too. Older adults, people with liver disease, or those on higher warfarin doses are more sensitive. A 75-year-old on 5 mg of warfarin who starts Bactrim for a UTI is at much higher risk than a 45-year-old on 2 mg.
When to Check Your INR - The Real Timeline
Waiting for your next scheduled INR test is not enough. You need to check sooner.- High-risk antibiotics (Bactrim, fluconazole): Check INR within 3 to 5 days after starting. Some clinics recommend checking even at 48 hours.
- Moderate-risk (ciprofloxacin, amoxicillin, erythromycin): Check at day 5 to 7.
- Low-risk (clindamycin, azithromycin): Stick to your regular schedule. No extra check needed unless you feel off.
- Rifampin: Check every 1-2 weeks for 6 to 8 weeks. The effect builds slowly and can last weeks after stopping.
Don’t wait for symptoms. Bleeding might not show up until it’s serious. A nosebleed, bruising, or dark stools could be your first warning - but by then, your INR might already be dangerously high. That’s why proactive testing matters.
What to Do If Your INR Spikes
If your INR jumps above 4.0, you’re in a danger zone. But don’t panic. Stopping warfarin suddenly can cause clots. Here’s what actually works:- INR 4.0-5.0: Skip your next warfarin dose. Recheck INR in 24-48 hours. Don’t take vitamin K unless your doctor says so.
- INR 5.0-9.0: Skip 1-2 doses. Your doctor may give you a small oral dose of vitamin K (1-2.5 mg). Avoid injections unless you’re actively bleeding.
- INR over 9.0 or active bleeding: Go to the ER. You’ll likely get vitamin K and possibly fresh frozen plasma.
Once the antibiotic finishes, your INR will usually settle back down. But don’t rush to increase your warfarin dose. It can take days to weeks for your liver enzymes and gut bacteria to return to normal. Recheck your INR 3-5 days after stopping the antibiotic before adjusting your dose.
Dental Visits and Minor Procedures
You don’t need to stop warfarin for most dental work - even extractions. The risk of bleeding is low if your INR is under 4.0. What you do need is the right antibiotic.If your dentist prescribes an antibiotic for infection or prevention, ask: Is this clindamycin? If not, ask why. Clindamycin is the safest choice. Avoid amoxicillin or ciprofloxacin unless absolutely necessary. Also, make sure your dentist knows you’re on warfarin. They may check your INR the day before your procedure - and that’s a good thing.

What the Research Really Says
One big study from 2012 found that warfarin users on antibiotics had more than double the risk of bleeding that led to hospitalization. That sounds scary. But a later study in JAMA Internal Medicine found something surprising: most people on antibiotics didn’t need a warfarin dose change. Their INR went up, but not enough to cause harm.The truth? The risk is real, but the harm isn’t inevitable. It’s about awareness, not avoidance. Patients who got their INR checked within a week of starting an antibiotic had far fewer bleeding events than those who didn’t. Monitoring is the shield. Not stopping the antibiotic. Not avoiding the doctor. Just checking your numbers.
Bottom Line: What You Should Do Today
- If you’re on warfarin and your doctor prescribes an antibiotic, ask: Is this one of the high-risk ones? If they say yes, ask about alternatives like clindamycin or azithromycin.
- Don’t wait for your next INR test. Schedule a check 3-5 days after starting the antibiotic.
- Keep a log: write down the antibiotic name, dose, start date, and your INR results. Bring it to every appointment.
- If you notice unusual bruising, bleeding gums, or dark urine - call your doctor immediately. Don’t wait.
- Never stop warfarin on your own. Even if you feel fine, stopping can cause a clot.
Warfarin isn’t outdated. It’s still the best option for many people - especially those with mechanical heart valves or severe mitral stenosis. Antibiotics aren’t the enemy. But together, they need careful handling. The goal isn’t to avoid one or the other. It’s to manage both safely - with smart checks, clear communication, and a little bit of vigilance.
Can I take amoxicillin while on warfarin?
Yes, but with caution. Amoxicillin is considered a moderate-risk antibiotic for warfarin users. It can raise your INR by 0.5 to 1.5 units in some people. Check your INR 5 to 7 days after starting amoxicillin. Your doctor may reduce your warfarin dose by 10-25% temporarily. Don’t stop either medication without advice.
Is Bactrim safe with warfarin?
No, Bactrim (trimethoprim-sulfamethoxazole) is high-risk. It can cause dangerous INR spikes - sometimes over 5.0 - within 2-3 days. Most patients need a 25-50% reduction in warfarin dose, or even skipping one dose. Always check your INR within 3-5 days of starting Bactrim. If you’re prescribed Bactrim, ask your doctor if a safer alternative like azithromycin is possible.
Do I need to stop warfarin before dental work?
Almost never. Stopping warfarin increases your risk of clotting more than the risk of bleeding from dental procedures. Keep taking it. Use clindamycin instead of amoxicillin or ciprofloxacin if an antibiotic is needed. Your dentist should check your INR the day before - a value under 4.0 is generally safe. Apply pressure after extraction and avoid aspirin or ibuprofen.
How long does it take for warfarin and antibiotics to interact?
It depends on the antibiotic. For CYP2C9 inhibitors like Bactrim or ciprofloxacin, the interaction can start within 24-48 hours. For gut microbiome effects (like with cephalosporins), it takes 3-5 days. Rifampin works slower - its effect builds over 1-2 weeks. That’s why timing your INR checks matters: check too early, and you miss the rise. Check too late, and you’ve already bled.
Can vitamin K help if my INR is too high?
Yes, but only under medical supervision. Oral vitamin K (1-2.5 mg) can help lower a high INR without causing rebound clots. It’s not a quick fix - it takes 12-24 hours to work. Don’t take vitamin K supplements on your own. Too much can make your warfarin less effective long-term. Your doctor will decide if and how much to give based on your INR and bleeding risk.
Does azithromycin affect warfarin?
Azithromycin has minimal effect on warfarin. It doesn’t strongly inhibit CYP2C9 or disrupt gut bacteria significantly. Most patients can take it without changing their warfarin dose. Standard INR monitoring is enough - no extra checks needed unless you have other risk factors like liver disease or are elderly.
What if I forget to check my INR after starting an antibiotic?
If you’ve been on the antibiotic for more than 5 days and haven’t checked your INR, get it tested as soon as possible. Don’t wait for symptoms. If you feel dizzy, weak, or notice unusual bruising or bleeding, go to an urgent care center or ER. If you’re asymptomatic but overdue, schedule a test within 24 hours. Missing one check doesn’t mean disaster - but it increases your risk. Stay on schedule.





Comments
Look, I've been on warfarin for 8 years and I've had like 5 different antibiotics. Bactrim is a nightmare, I know. But honestly? Most docs don't even think about this stuff until you're bleeding out. I had a nurse tell me 'just skip your next dose' when my INR hit 6.5. No warning, no follow-up. This post is the first time anyone explained WHY it happens. Thank you.
Indian doctors never warn about this. My uncle took ciprofloxacin for fever and ended up in ICU. No one told him warfarin and antibiotics don't mix. Why do Western doctors care more? Maybe because they have insurance to cover the lawsuits.
Clindamycin is the only safe choice. End of story. Anyone prescribing amoxicillin to a warfarin patient is negligent.
bro i just took amoxicillin last week for a tooth infection and my INR went from 2.8 to 3.9 and i didn't even know it. i thought i was just tired. now i'm scared to even take tylenol.
This is so important for everyone on blood thinners. I'm from India and we don't talk about this enough. My cousin had a stroke because she stopped her warfarin after a dentist visit. Please share this with your family. Knowledge saves lives.
Actually, the JAMA study showed most people don't need dose adjustments. This post is fearmongering. If your INR is stable and you're asymptomatic, don't overreact. Over-monitoring causes anxiety and unnecessary dose changes.
Thank you for this. I printed it out and gave it to my cardiologist. He said 'good job' and added it to his patient handouts. 🙌 Also, clindamycin for dental work is the way. No drama. No panic. Just safety.
I'm a nurse practitioner and I can't tell you how many patients I've seen who didn't know about these interactions. This is exactly the kind of information that should be in every pharmacy's warfarin starter kit. Thank you for writing this so clearly.
America's healthcare system is broken. You need to know which antibiotic is risky? That's on you. Why isn't this in the drug label? Why isn't the EHR auto-alerting? Because profit > safety. Wake up.
While the clinical data presented is generally accurate, one must consider the pharmacokinetic variability among individuals, particularly with regard to hepatic metabolism and gut flora composition, which may significantly alter the magnitude of interaction
This is the kind of post that makes me believe in Reddit. Clear, accurate, practical. I've been on warfarin since 2018 and I wish I'd read this back then. I'll be sharing it with my support group. Thank you.
Clindamycin isn't 'safe'. It causes C. diff. You're trading one risk for another. This advice is dangerous.
My grandma takes warfarin and gets amoxicillin every time she gets a sinus infection. She's 82 and never had a bleed. Maybe this stuff matters more for some people than others?
if you're on warfarin and your doc prescribes an antibiotic just ask 'is this gonna mess with my blood thinner?' 90% of the time they'll say 'oh yeah good call let me check' and swap it. no big deal.
The CYP2C9 polymorphism significantly modulates the interaction magnitude, particularly in patients with *2 or *3 alleles. Additionally, gut microbiome dysbiosis from antibiotics may induce compensatory vitamin K synthesis in the colon, potentially attenuating INR elevation in chronic users.
YOU'RE WELCOME FOR THIS POST. I spent 3 weeks in the hospital because my doctor didn't know this. Now I'm the one educating every new warfarin patient I meet. 🩸🩹 #WarfarinWarrior
My cousin died from a brain bleed after taking ciprofloxacin. He didn't even know he was on warfarin. His doctor said 'it's fine'. Don't let this happen to your family. This post is a lifeline.