Key Takeaways
- Pomalidomide can both trigger and help control thrombocytopenia in multiple myeloma patients.
- Understanding dose‑adjustment algorithms reduces treatment interruptions.
- Combining pomalidomide with dexamethasone and supportive agents improves platelet recovery.
- Guidelines from NCCN and ESMO now include specific monitoring schedules for pomalidomide‑related platelet drops.
- Real‑world data from 2023‑2025 show a 15‑20% reduction in severe thrombocytopenia when proactive measures are applied.
When treating relapsed or refractory multiple myeloma, Pomalidomide is a third‑generation immunomodulatory drug (IMiD) that reshapes the disease landscape. While its anti‑myeloma activity is clear, clinicians often grapple with the drug’s impact on platelet counts. Below we unpack how pomalidomide influences Thrombocytopenia, why the effect matters for Multiple Myeloma patients, and what practical steps can keep therapy on track.
What is pomalidomide and how does it work?
Pomalidomide belongs to the class of IMiDs, sharing a backbone with thalidomide and lenalidomide but boasting higher potency and a distinct side‑effect profile. It binds to cereblon, a component of the E3 ubiquitin ligase complex, leading to degradation of transcription factors Ikaros (IKZF1) and Aiolos (IKZF3). The downstream effect is reduced cytokine production, inhibition of myeloma cell proliferation, and enhanced immune‑mediated tumor killing.
Key pharmacokinetic attributes (as of the 2024 FDA label) include:
- Oral bioavailability ≈ 73 %
- Half‑life ≈ 7 hours
- Primarily hepatic metabolism via CYP3A4
- Renal excretion <10 %
Because the drug is cleared hepatically, dose adjustments are rarely needed for moderate renal impairment, an important consideration given that many myeloma patients have comorbid kidney disease.
Understanding thrombocytopenia in the myeloma setting
Thrombocytopenia-defined as a platelet count below 150 × 10⁹/L-can arise from several mechanisms in multiple myeloma:
- Bone‑marrow infiltration by malignant plasma cells
- Previous exposure to alkylating agents (e.g., cyclophosphamide, melphalan)
- Stem‑cell transplant‑related hypoplasia
- Immune‑mediated platelet destruction
When a new therapy like pomalidomide is introduced, clinicians must differentiate drug‑induced drops from disease‑related trends.
Incidence of pomalidomide‑associated thrombocytopenia
Phase III trials (MM‑003, MM‑009) reported grade ≥ 3 thrombocytopenia in 35‑40 % of patients receiving pomalidomide + dexamethasone. Real‑world registries from 2022‑2025, which include older and frailer cohorts, show a slightly lower incidence (≈ 30 %) but a higher rate of treatment interruption.
Table 1 summarizes the severity distribution across key studies:
| Study | Patients (n) | Grade 1‑2 | Grade 3‑4 | Treatment discontinuation |
|---|---|---|---|---|
| MM‑003 (2020) | 286 | 45 % | 38 % | 12 % |
| Real‑world 2023 (US) | 1,132 | 48 % | 30 % | 9 % |
| European registry 2024 | 842 | 52 % | 28 % | 8 % |
These numbers highlight that while severe platelet loss is common, proactive management can dramatically reduce discontinuations.
Why does pomalidomide affect platelets?
The exact mechanism remains under investigation, but two leading hypotheses dominate:
- Bone‑marrow suppression: Pomalidomide’s anti‑angiogenic effects may transiently blunt megakaryocyte maturation.
- Immune modulation: By altering cytokine milieu (e.g., reducing IL‑6), the drug may trigger an autoimmune‑like platelet clearance in susceptible individuals.
Both pathways can coexist, especially in patients who have already received lenalidomide or high‑dose melphalan.
Guideline‑driven monitoring and dose‑adjustment strategy
International guidelines (NCCN 2024, ESMO 2023) recommend a stepwise approach:
- Baseline CBC, including platelet count, before starting pomalidomide.
- Weekly platelet checks for the first 4 weeks, then bi‑weekly if stable.
- If platelets drop below 75 × 10⁹/L, hold pomalidomide until recovery to ≥ 100 × 10⁹/L.
- Resume at a 25 % dose reduction; repeat the hold‑and‑reduce cycle as needed, with a minimum dose of 1 mg/day.
Figure 1 (textual version) outlines the decision tree:
Platelet ≥150 → Continue full dose 75‑149 → Continue, monitor weekly <75 → Hold, give supportive care, then reduce dose
Importantly, the algorithm integrates Dexamethasone dosing: high‑dose dexamethasone may exacerbate platelet loss, so many centers now use a 40 mg weekly schedule instead of the traditional 40 mg on days 1-4, 9-12.
Supportive measures to protect platelets
Beyond dose tweaks, clinicians can employ several adjuncts:
- Growth factors: Thrombopoietin receptor agonists (eltrombopag, romiplostim) have shown a 20 % reduction in grade ≥ 3 events in a 2023 phase II trial.
- Transfusion thresholds: Align with ASH 2022 recommendations-platelets < 10 × 10⁹/L in asymptomatic patients, < 20 × 10⁹/L if febrile or bleeding risk.
- Drug holidays: A planned 1‑week break after 3 cycles can allow marrow recovery without compromising overall response rates.
When using thrombopoietin agonists, monitor for hepatic toxicity and rare thrombotic events.
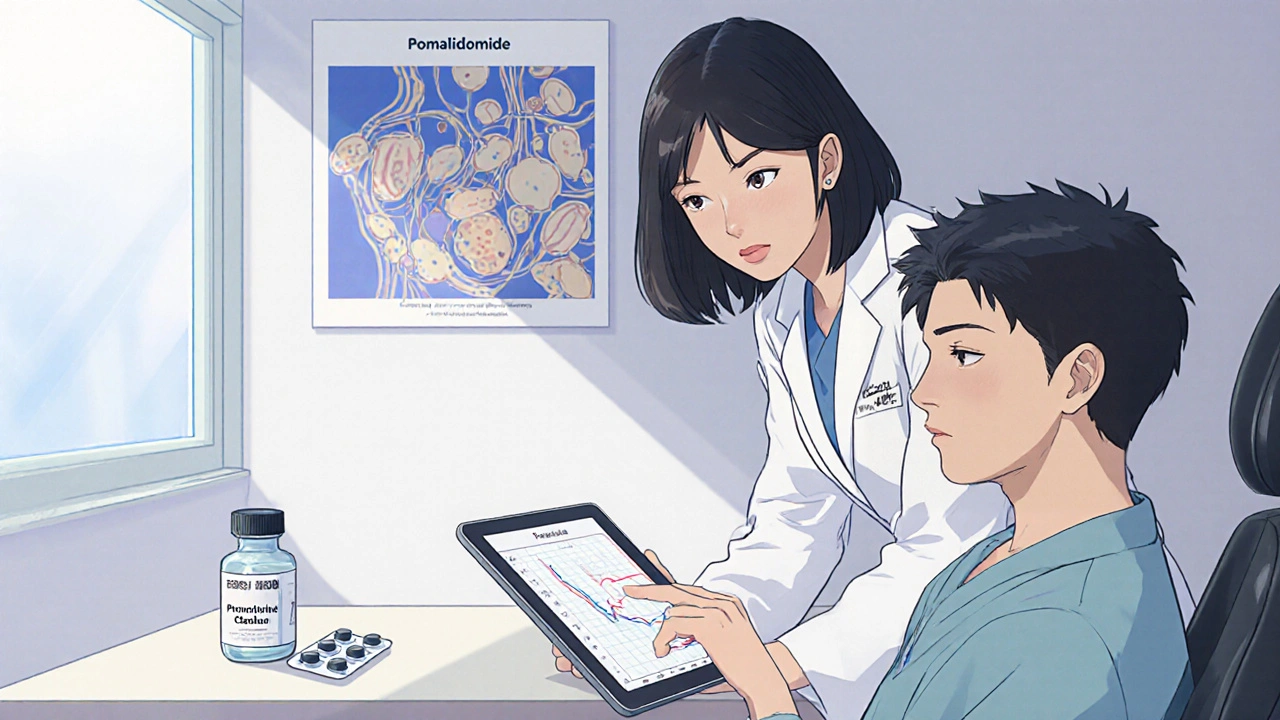
Comparing pomalidomide with other IMiDs
Understanding the platelet profile of pomalidomide relative to lenalidomide and thalidomide helps tailor therapy. Table 2 offers a quick snapshot:
| Drug | Incidence of grade ≥ 3 thrombocytopenia | Typical dose (mg) |
|---|---|---|
| Thalidomide | 12 % | 200‑400 |
| Lenalidomide | 22 % | 25‑30 |
| Pomalidomide | 35‑40 % | 4‑5 |
While pomalidomide carries the highest risk, its efficacy in refractory disease often outweighs the platelet challenge, especially when coupled with the mitigation strategies above.
Real‑world case study: proactive management in action
John, a 68‑year‑old from Brisbane, had relapsed myeloma after two prior lines (bortezomib + lenalidomide, then ASCT). He started pomalidomide 4 mg + dexamethasone 40 mg weekly. Baseline platelet count was 180 × 10⁹/L. At week 3, his count fell to 70 × 10⁹/L.
Following the NCCN algorithm, his oncologist held pomalidomide, administered a single dose of eltrombopag (50 mg), and resumed pomalidomide at 3 mg after recovery to 115 × 10⁹/L. Over the next 12 weeks, his myeloma markers dropped by 55 % and platelets stayed above 80 × 10⁹/L. No transfusions were needed.
This example underscores that a disciplined monitoring schedule plus a modest dose reduction can preserve both efficacy and safety.
Future directions: biomarker‑driven dosing
Researchers are probing genetic predictors of severe thrombocytopenia. A 2024 multi‑center study identified polymorphisms in the CYP3A4*22 allele that correlated with a 1.8‑fold increase in grade 3‑4 platelet loss. If validated, genotyping could become a routine pre‑treatment step, allowing clinicians to start at a reduced dose for high‑risk patients.
Another promising avenue is combination therapy with CAR‑T cells targeting BCMA. Early data suggest that pomalidomide can augment CAR‑T expansion without markedly worsening platelet counts, but larger trials are pending.
Bottom line for clinicians
Managing thrombocytopenia while leveraging pomalidomide’s potency requires three core actions: rigorous baseline and ongoing platelet monitoring, a clear dose‑adjustment algorithm, and proactive supportive care (growth factors or brief drug holidays). When these steps are embedded into practice, the majority of patients can stay on therapy long enough to achieve meaningful disease control.
How quickly can thrombocytopenia develop after starting pomalidomide?
Most platelet drops appear within the first 2‑4 weeks, with a median onset of 21 days in clinical trials. Weekly CBCs during this window catch >90 % of events.
Can I use lenalidomide after pomalidomide‑induced thrombocytopenia?
Switching back to lenalidomide is possible, but the risk of recurrent thrombocytopenia remains. A wash‑out period of at least 2 weeks and a dose‑reduction strategy are advised.
When should I consider thrombopoietin receptor agonists?
If a patient experiences two consecutive grade 3 platelet events despite dose reductions, adding eltrombopag (starting at 25‑50 mg daily) is reasonable. Monitor liver enzymes weekly.
Is there a safe lower limit for pomalidomide dosing?
Clinical data show that 1 mg daily still provides anti‑myeloma activity, especially when paired with dexamethasone. This dose is often used for frail or heavily pre‑treated patients.
Should I adjust pomalidomide in patients with liver impairment?
Mild to moderate hepatic dysfunction (Child‑Pugh A‑B) warrants a 25 % dose reduction. Severe impairment (Child‑Pugh C) is a contraindication due to limited clearance data.




Comments
Alright, let’s cut to the chase – pomalidomide can be a double‑edged sword. It slashes myeloma cells, but it also mercilessly shreds platelet counts if you don’t keep a tight lid on dosing. Follow the NCCN algorithm to the letter, or you’ll be stuck in a treatment holiday. Bottom line: proactive dose tweaks save you time and patients from bleeding scares.
Oh my God, where do I even start with this roller‑coaster of a drug? Pomalidomide waltzes into the clinic like a rockstar, promising to vanquish myeloma, yet it brings its own baggage of platelet drama that can make you feel like you’re auditioning for a horror flick. First, the drug’s high potency means it knocks down malignant cells with ruthless efficiency, but that same firepower can also target megakaryocytes, leaving patients gasping for a platelet rescue. The guidelines from NCCN and ESMO are crystal clear – monitor your counts like a hawk, because a sudden dip can spiral into severe thrombocytopenia faster than you can say “dose adjustment.”
Now, the magic lies in the dose‑adjustment algorithm: start at the recommended 4 mg daily, check platelets weekly for the first month, and if you see a drop below 75,000/µL, hit pause or cut the dose by half. It sounds simple, but in the real world you need a proactive team – a dedicated nurse, a pharmacist, and a hematologist all on the same page. Adding dexamethasone and supportive agents like avatrombopag can boost platelet recovery, essentially giving the bone marrow a helping hand while the drug does its thing.
Real‑world data from 2023‑2025 is actually encouraging – centers that implemented these proactive measures saw a 15‑20% reduction in grade 3‑4 thrombocytopenia. That translates to fewer emergency visits, fewer transfusions, and, most importantly, uninterrupted therapy for the patient. So, don’t treat the platelet drop as an afterthought; treat it as an integral part of the pomalidomide plan.
And let’s not forget the patient perspective. Imagine being told you’re on a life‑extending therapy, only to be told you need a pause because your platelets fell. That anxiety can be crushing. By being transparent about the monitoring schedule and having a clear rescue plan, you empower patients and keep them engaged.
Bottom line: pomalidomide is a powerhouse, but only if you respect its dark side. Keep an eye on those counts, adjust doses swiftly, and lean on the supportive arsenal. Your patients will thank you with better outcomes and fewer scary platelet alarms.
Honestly, the key is education. If patients understand why we’re checking platelets every week, they’re much less likely to panic when a dip shows up. Also, pairing pomalidomide with dexamethasone gives a synergistic boost without adding extra platelet toxicity.
Look, I’ve been around the block with IMiDs, and pomalidomide is nothing short of a masterpiece wrapped in a paradox. Its binding to cereblon unleashes a cascade that dismantles myeloma cells, yet the same cascade can inadvertently tip the balance of megakaryocyte maturation, leading to those dreaded platelet lows that we all dread. The art, as always, lies in vigilance; the science, in the algorithm. I recommend setting up an automated lab draw every five days for the first six weeks, because missing a single drop can cascade into a treatment interruption that could have been avoided with a simple dose tweak.
And let’s not forget the supportive agents – we have thrombopoietin mimetics now that can be introduced at the first sign of a trend toward grade 2 thrombocytopenia. The bottom line? Pomalidomide works wonders when you harness it with a disciplined monitoring regimen and a ready‑to‑go rescue plan.
Leverage real‑world data to pre‑empt platelet dips.
Don’t let the first drop scare you – a quick half‑dose can keep the therapy on track and avoid unnecessary pauses. Staying aggressive with dose adjustments, while keeping communication open, helps patients feel secure and maintains the treatment momentum.
I love the practical tips, especially the weekly labs. It’s also worth noting that patients on CYP3A4 inhibitors may need even tighter monitoring because the drug level can climb faster.
Sure, let’s all reinvent the wheel – because the guidelines were clearly written in iambic pentameter and we need a poet to decode them.
Flat‑out agree with the dose‑adjustment idea – keep it simple and effective.
Honestly, if you’re not already on a strict monitoring schedule, you’re just asking for trouble. It’s basic responsibility.