Most people with fatty liver don’t know they have it. No pain. No symptoms. Just a routine blood test showing slightly elevated liver enzymes-and suddenly, you’re told you have NAFLD. But what does that really mean? Is it harmless, or is it a warning sign for something worse? The difference between simple fatty liver and its more dangerous cousin, NASH, isn’t just medical jargon-it’s the difference between watching and waiting, and taking real action before your liver starts to scar.
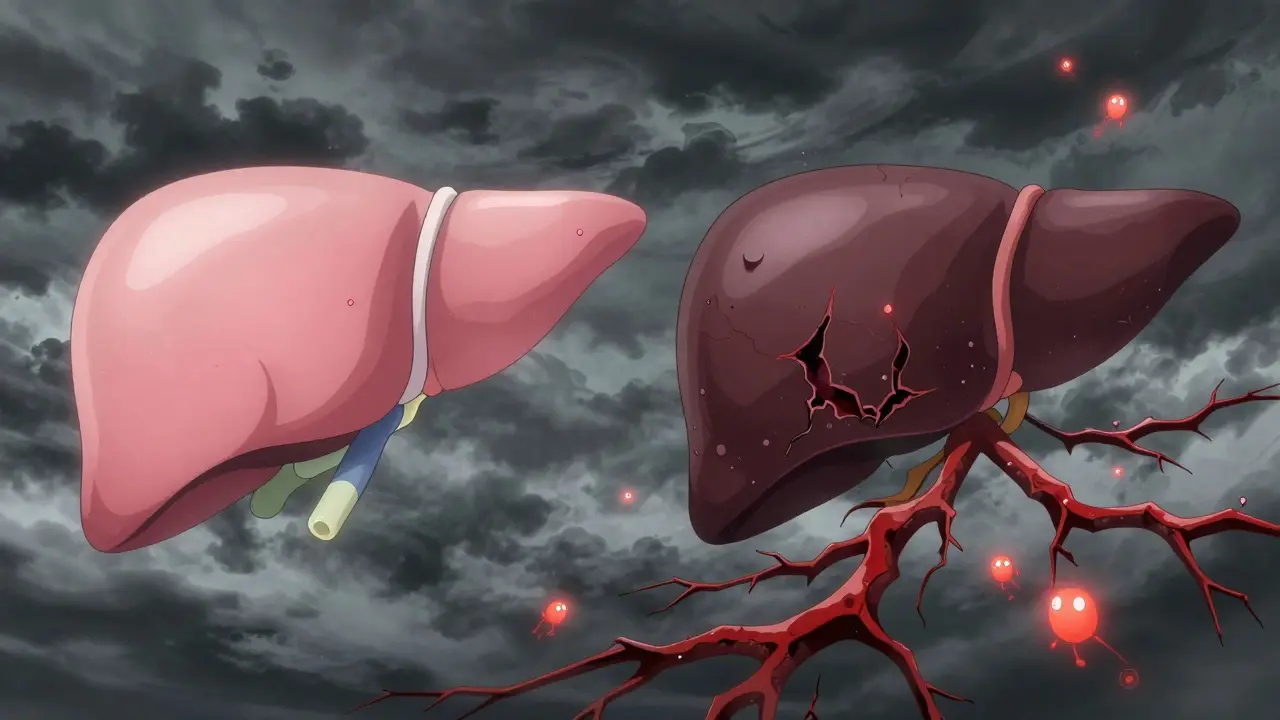
What’s the real difference between NAFLD and NASH?
NAFLD stands for Non-Alcoholic Fatty Liver Disease. It’s not caused by drinking alcohol. It’s caused by fat building up in your liver-5% or more of its weight. That’s it. No inflammation. No cell damage. Just fat sitting there. This version is called NAFL-simple fatty liver. About 80% of people with NAFLD fall into this category. For most, it doesn’t progress. Their liver stays healthy, even with the fat.
NASH is the problem child. It’s when that fat triggers inflammation and starts killing liver cells. You get ballooning cells, immune cells moving in, and the liver trying to heal itself-by making scar tissue. That’s fibrosis. And once fibrosis starts, it doesn’t always stop. NASH isn’t just fat anymore. It’s active damage. And that’s what puts you at risk for cirrhosis, liver failure, or even liver cancer.
Here’s the catch: you can’t tell the difference just by looking at an ultrasound or even by your ALT levels. A fatty liver on a scan could be NAFL or NASH. The only way to know for sure is a liver biopsy. And that’s why so many people are caught off guard-they think they just have "a bit of fat," but by the time they feel symptoms, the damage is already advanced.
Fibrosis is the real enemy
Doctors don’t just care if you have NASH. They care how far the scarring has gone. That’s fibrosis staging: 0 to 4.
- Stage 0: No scarring
- Stage 1: Tiny scars around blood vessels
- Stage 2: Scars spreading
- Stage 3: Bridges of scar tissue forming across the liver
- Stage 4: Cirrhosis-the liver is hardened, shrunken, and failing
Here’s the hard truth: fibrosis stage is the best predictor of your future. A 2022 study tracking over 1,200 patients found that people with stage 3 or 4 fibrosis had a 12-25% chance of dying from liver disease in the next 10 years. Those with stage 0-2? Less than 2%. It doesn’t matter if you’re diagnosed with NASH-if your fibrosis is still mild, your risk is low. But if you’ve got bridging fibrosis, you’re in the danger zone.
And here’s something most don’t realize: you can have NASH without fibrosis. Or you can have fibrosis without NASH. But the combination? That’s when the clock starts ticking.
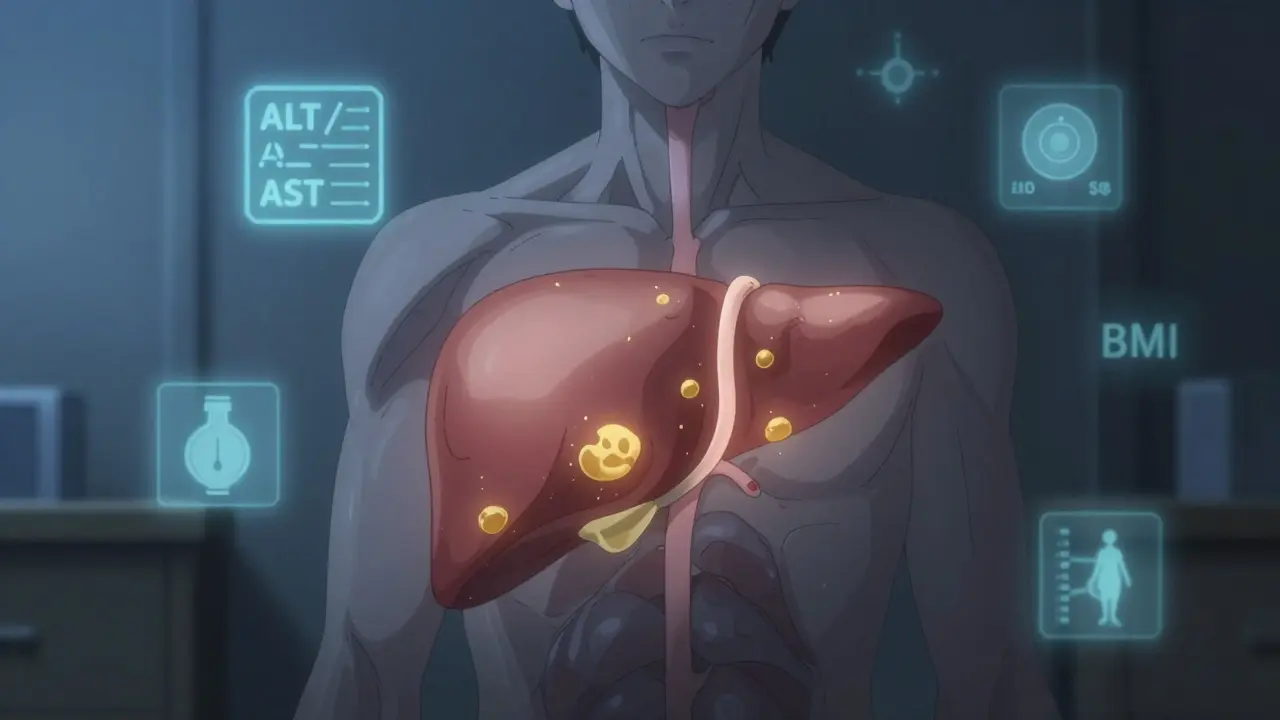
Who’s most at risk of turning NAFLD into NASH?
It’s not random. There’s a clear pattern. The people who go from simple fatty liver to NASH almost always have metabolic trouble.
- Obesity (BMI over 30): 70-90% of NASH patients have it
- Type 2 diabetes: Half to 70% of NASH cases
- High blood pressure: 60-75%
- High triglycerides, low HDL: Almost universal
- Obstructive sleep apnea: 30-50% of NASH patients
If you have three or more of these, you have metabolic syndrome. And if you have metabolic syndrome plus elevated liver enzymes? You’re in the high-risk group. That’s not a coincidence. Your liver is drowning in fat because your body can’t process sugar and fat properly. Insulin resistance is the engine driving this whole thing.
It’s not about willpower. It’s not about eating too much pizza. It’s biology. Your liver is overwhelmed. And if you keep feeding it sugar, refined carbs, and saturated fats, it starts to break down.
How do you know if you’ve crossed the line?
Most people have no symptoms until it’s too late. Fatigue? Maybe. Mild discomfort under the right rib cage? Sometimes. But often, the first sign is a blood test.
ALT and AST levels are the first red flags. Normal ALT is 7-55 U/L. If yours is consistently above 40, especially with high triglycerides or waist size over 40 inches (men) or 35 inches (women), it’s time to dig deeper.
Non-invasive tests help:
- FIB-4 score: Uses your age, ALT, AST, and platelet count. Over 1.3? Possible advanced fibrosis. Over 2.67? High risk.
- APRI score: ALT over AST? Above 0.5? Red flag.
- FibroScan: Measures liver stiffness. Over 7.1 kPa? Suggests fibrosis. Over 10 kPa? Strong sign of advanced scarring.
- MRI-PDFF: The most accurate way to measure fat in the liver-up to 95% accurate.
But here’s the catch: none of these can confirm NASH. Only a biopsy can. That’s why doctors only recommend it if your non-invasive tests suggest advanced fibrosis. Biopsies carry a tiny risk (0.01-0.1%), and they’re not perfect-sampling error can miss the damaged areas.
What happens if you do nothing?
NAFL? For most, nothing. Life goes on. No treatment needed. Just keep your weight stable and avoid sugar.
NASH? That’s different. Without change, 20-40% will develop cirrhosis in 10-20 years. 5-12% will get liver cancer. And your risk of heart disease? It’s already higher than the general population. In fact, heart disease kills more people with fatty liver than liver disease does.
One 2019 study followed 1,245 people for 15 years. Only 12% of NAFL patients developed serious fibrosis. But 42% of NASH patients did. That’s a four-fold increase in risk.
And here’s the grim part: once you hit stage 3 fibrosis, your chances of reversing it drop sharply. The liver can heal-but only if the damage hasn’t become permanent.
Can you reverse it?
Yes. But only if you act early.
Weight loss is the most powerful treatment we have. Losing 7-10% of your body weight can reverse NASH in most people. In one study, 90% of patients who lost that much saw their NASH turn back into simple fatty liver. Fibrosis improved in 85%.
It’s not about extreme diets. It’s about consistency:
- Drop sugary drinks-soda, juice, sweetened coffee
- Swap white bread and pasta for whole grains
- Reduce saturated fats-fried food, fatty meats, butter
- Move daily-even a 30-minute walk helps
Medications? There’s finally one approved. In March 2023, the FDA approved resmetirom (Rezdiffra) for NASH patients with moderate to advanced fibrosis. It’s not a cure. But in trials, 26% of patients saw fibrosis improve, compared to 10% on placebo.
More drugs are coming. Over 30 are in phase 3 trials. But none replace lifestyle change. They’re add-ons-for those who’ve already done the hard work.

The big shift: NAFLD is now MASLD
In June 2023, liver experts around the world agreed: the term "non-alcoholic" was outdated and stigmatizing. So they changed it.
NAFLD is now MASLD-Metabolic Dysfunction-Associated Steatotic Liver Disease. NASH is now MASH-Metabolic Dysfunction-Associated Steatohepatitis.
Why? Because it’s not about what you *don’t* drink. It’s about what you *do* have: insulin resistance, belly fat, high blood sugar, high blood pressure. The new name focuses on the real cause: metabolism.
Diagnosis now requires at least one of five metabolic traits:
- BMI ≥25
- Waist circumference over 94 cm (men) or 80 cm (women)
- Type 2 diabetes
- High blood pressure
- Dyslipidemia (high triglycerides or low HDL)
This change makes it easier to spot risk early. If you have metabolic syndrome, your liver is on the line.
What should you do now?
If you’ve been told you have fatty liver:
- Don’t panic. Most cases are simple and harmless.
- Ask for your ALT, AST, platelet count, and triglyceride levels.
- Calculate your FIB-4 score: (Age × AST) / (Platelets × √ALT). Use an online calculator.
- If FIB-4 is above 1.3, ask about a FibroScan.
- If you’re overweight or have diabetes, aim to lose 7-10% of your body weight.
- Get screened for sleep apnea if you snore or feel tired all day.
- Don’t wait for symptoms. By then, it’s often too late.
And if you’re healthy? Start now. Cut the sugar. Move more. Get your blood work done every year. Fatty liver doesn’t come out of nowhere. It builds quietly. And the best time to stop it? Before you even know it’s there.
Can NAFLD turn into NASH even if I’m not overweight?
Yes. While obesity is the biggest risk factor, people with normal weight can still develop NASH if they have insulin resistance, high blood sugar, or high triglycerides. This is called "lean NAFLD" and accounts for about 10-20% of cases. Genetics, gut health, and sedentary lifestyle play a role too.
Is a liver biopsy always necessary to diagnose NASH?
No. Most people don’t need one. Doctors use blood tests and FibroScan first. A biopsy is only recommended if those tests suggest advanced fibrosis (FIB-4 > 2.67 or FibroScan > 10 kPa). Biopsies are invasive and carry small risks, so they’re reserved for high-risk cases.
Can I drink alcohol if I have NAFLD or NASH?
The safest answer is no. Even small amounts of alcohol can worsen liver damage in people with fatty liver disease. While NAFLD is defined as "non-alcoholic," any alcohol adds stress to an already overloaded liver. Most experts recommend complete abstinence if you have NASH or fibrosis.
How long does it take for NAFLD to become NASH?
There’s no set timeline. For some, it takes 10-15 years. For others with strong metabolic risk factors-like uncontrolled diabetes or rapid weight gain-it can happen in just a few years. Progression depends on how many risk factors you have and whether you make lifestyle changes.
Are there any supplements that help with NASH?
Vitamin E has shown modest benefit in non-diabetic NASH patients in clinical trials, but it’s not recommended for everyone due to potential risks. Omega-3s may help lower liver fat, but they don’t reverse fibrosis. No supplement replaces weight loss or medical treatment. Always talk to your doctor before taking anything-some supplements can harm the liver.
If I lose weight, will my liver heal completely?
If you lose 7-10% of your body weight and keep it off, you can reverse NASH in most cases and reduce fibrosis significantly. Some people even return to a completely normal liver. But if fibrosis is already stage 3 or 4, complete reversal is rare-though progression can still be stopped. The earlier you act, the better your chances.
What’s next?
The future of fatty liver disease is changing. New drugs are coming. Screening is getting better. But the core truth hasn’t changed: your liver responds to what you do every day. Eat better. Move more. Lose weight. Control your blood sugar. Those aren’t just "good habits." They’re the only proven treatments we have right now.
And if you’re reading this because your doctor mentioned "fatty liver"-don’t ignore it. Don’t assume it’s harmless. Ask the right questions. Get the right tests. Take action before your liver starts to scar. Your future self will thank you.






Comments
Man, this hit different coming from India where we're seeing more and more young folks with fatty liver from too much biryani and soda. No one talks about it until their ALT is through the roof. We need more awareness here.
I got diagnosed last year and thought I was fine until I read this. Now I'm cutting out juice, walking after dinner, and actually checking my FIB-4. My liver is gonna thank me 😊
Thank you for writing this in plain English. So many docs just say 'lose weight' and leave it at that. You actually gave actionable steps - FIB-4, FibroScan, ditching soda. This is what real patient education looks like.
Oh wow, another 'eat less pizza' manifesto. How revolutionary. I'm sure the 30-year-old with a BMI of 22 and NASH just needed to stop eating croissants. Meanwhile, the real issue - gut microbiome dysbiosis and endocrine disruptors - gets buried under lazy lifestyle advice. But sure, blame the carbs.
So i read this whole thing and like 90% of it is true but i think people dont realize that its not just about weight its about insulin resistance like if you got diabetes and your liver is screaming for help and you still eat white rice and sugar every day you are basically asking your liver to die. Also fibroscan is way better than biopsy like why would you stick a needle in someone if you can just scan it? And resmetirom is a game changer but its like 1000 bucks a month and insurance wont cover it so good luck if you dont have good benefits
Another feel-good article from someone who clearly never had to deal with stage 3 fibrosis. You talk about weight loss like it’s a choice. Try losing 10% when you’re on 12 medications, have sleep apnea, and your job requires you to sit 12 hours a day. This isn’t a wellness blog. It’s a death sentence for the working poor.
As someone from India who's seen family members get diagnosed with MASLD, I'm glad this is getting attention. We need more public health campaigns here - especially in small towns where people think 'liver problem' means only alcoholics get it. This info should be in schools and workplaces.
Metabolic dysfunction is the key term here - and it's systemic. The liver is the canary in the coal mine. The real tragedy is that primary care providers still don't screen for it unless the patient is obese. We need routine ALT + FIB-4 in annual panels for anyone over 30 with metabolic risk factors. Period.
So you're saying if I drink diet soda and do yoga I'm fine? What about the guy who eats clean but has PCOS and insulin resistance? This article ignores genetics and epigenetics. Also fibrosis stage 3 isn't reversible? That's not what the 2023 Lancet paper said
Let’s be honest - this whole NAFLD to MASLD rebranding is just corporate medicine repackaging failure as a new diagnosis. We’ve been here before: cholesterol, hypertension, diabetes - all renamed, all monetized. The real solution? Stop subsidizing corn syrup. Stop letting Big Pharma sell us drugs for problems they helped create. But no, let’s just give people another pill and call it progress.
The liver doesn’t care about your FIB-4 score. It cares about your insulin levels. Your cortisol. Your sleep. Your stress. Your trauma. You can’t biopsy that. You can’t scan that. And yet here we are, reducing a systemic metabolic collapse to a liver test.
People are dying because we treat symptoms instead of root causes. We call it MASLD now, but it’s still the same disease of abundance - and we’re treating it like a personal failure, not a societal one.
And don’t get me started on resmetirom. A drug that improves fibrosis by 16% over placebo? That’s not a cure. That’s a Band-Aid on a ruptured artery. We need policy change. We need food justice. We need to stop treating the liver like it’s separate from the rest of the body.
But sure, keep calculating your FIB-4 and buying organic kale. The system loves that.
Resmetirom approval was based on surrogate endpoints not hard outcomes. FIB-4 isn't validated for all populations. FibroScan has high inter-operator variability. And you didn't mention that 40% of NASH patients have normal ALT. So this entire framework is built on shaky science.
Back home in Nigeria, people think liver disease is from too much palm oil or bad water. No one knows about insulin or belly fat. This post should be translated. We need this info where the problem is growing fast.
Actually, you’re right - the real enemy isn’t fat. It’s the belief that this is just a personal problem. The system designed this. Processed food is cheaper than broccoli. A gym membership costs more than a month’s rent in some places. And we’re blaming people for being sick in a world that makes them sick. But hey, at least we’ve got a new acronym.