Biosimilar Switching: What You Need to Know About Switching to Biosimilar Medications
When you hear biosimilar switching, the process of replacing a brand-name biologic drug with a highly similar, lower-cost version approved by health regulators. Also known as biologic substitution, it’s becoming common in treating conditions like rheumatoid arthritis, Crohn’s disease, and certain cancers. Unlike regular generics, biosimilars aren’t exact copies—they’re made from living cells, so they’re more complex. But they’re not guesswork. Regulatory agencies like the FDA and EMA require them to match the original in safety, purity, and potency before approval.
Biosimilar switching isn’t random. It’s often guided by doctors, pharmacists, and health systems trying to cut costs without losing effectiveness. In the U.S., many states allow pharmacists to substitute biosimilars unless the doctor says no. But patients don’t always know when the switch happens. That’s why clear communication matters. If you’ve been on a biologic like Humira or Enbrel and suddenly get a different name on your prescription, ask: Is this a biosimilar? Has it been studied in people like me? Will my insurance cover it the same way?
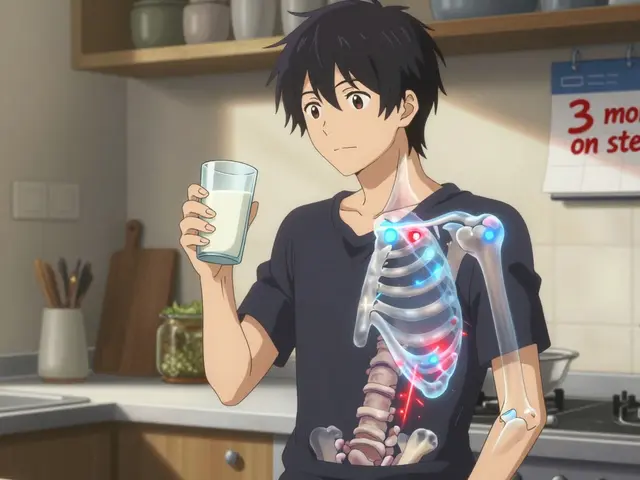
There’s a lot of confusion around biosimilar drugs, medications designed to mimic complex biologics with no clinically meaningful differences in safety or effectiveness. Some worry they’re "inferior"—but studies show they work just as well for most people. The biggest risks? Rare immune reactions or loss of effectiveness over time. That’s why monitoring matters. If you switch and notice new fatigue, swelling, or worsening symptoms, tell your doctor. It’s not always the drug—it could be stress, diet, or something else. But you need to rule out a reaction.
Generic medications, chemically identical copies of small-molecule drugs, are different from biosimilars. You can swap generics for brand-name pills like metformin or lisinopril without much concern. Biosimilars? They’re trickier. You can’t just swap them like candy. They need careful handling, tracking, and sometimes patient consent. That’s why drug substitution, the act of replacing one medication with another at the pharmacy level isn’t automatic with biosimilars. Many places require the prescriber to approve it first.
And then there’s medication safety, the practice of preventing harm from drugs through proper prescribing, dispensing, and monitoring. With biosimilar switching, safety means knowing exactly what you’re taking. Keep a list. Check labels. Ask your pharmacist to confirm the name and manufacturer. Don’t assume your refill is the same. A small change in packaging or pill color can be a sign of a switch.
Most people who switch to biosimilars do fine. Many save hundreds—or even thousands—of dollars a year. But it’s not one-size-fits-all. If you’re stable on your current drug, switching might not be needed. If you’re struggling with cost, it could be a game-changer. The key is being informed, not afraid. You have the right to ask questions. You have the right to know what’s in your prescription. And you have the right to speak up if something feels off.
Below, you’ll find real-world guides on how to check your meds, spot dangerous interactions, and talk to your pharmacist about cost-saving options. These aren’t theory pieces. They’re tools people use every day to stay safe, save money, and take control of their treatment.
Biosimilar switching lets patients move from expensive originator biologics to cheaper, equally effective versions. Learn what happens when you switch, why some people stop, and how to do it safely with proven data.
Read more