Steroid-Induced Osteoporosis Prevention Calculator
Personalized Prevention Guide
This tool calculates your specific calcium, vitamin D needs, and determines if you should consider bisphosphonate treatment based on the article's recommendations for steroid-induced osteoporosis prevention.
When you’re on long-term steroids-whether for asthma, rheumatoid arthritis, or an autoimmune condition-you’re not just managing inflammation. You’re also quietly putting your bones at risk. Steroid-induced osteoporosis isn’t a slow, distant threat. It can start within three to six months of starting treatment. And if you’re taking just 5 mg of prednisone a day or more, your fracture risk can jump up to 17 times higher than someone not on steroids. The scary part? Most people don’t even know it’s happening until they break a bone.
Why Steroids Attack Your Bones
Steroids don’t just calm your immune system. They mess with how your bones rebuild themselves. Your skeleton is always changing-old bone breaks down, new bone forms. That’s called remodeling. Steroids throw this process out of balance. They shut down the cells that build bone (osteoblasts), cutting bone formation by up to 70%. At the same time, they crank up the cells that break bone down (osteoclasts), increasing resorption by about 30%. The result? Your bones get thinner, weaker, and more likely to snap-even from something as simple as a fall or a cough.This isn’t just a problem for older adults. Even someone in their 30s or 40s on long-term steroids can lose bone density fast. And unlike regular osteoporosis, which develops over years, steroid-induced bone loss can be dramatic within the first year. Studies show that 12% of people taking 7.5 mg or more of prednisone daily will have a spine fracture within 12 months.
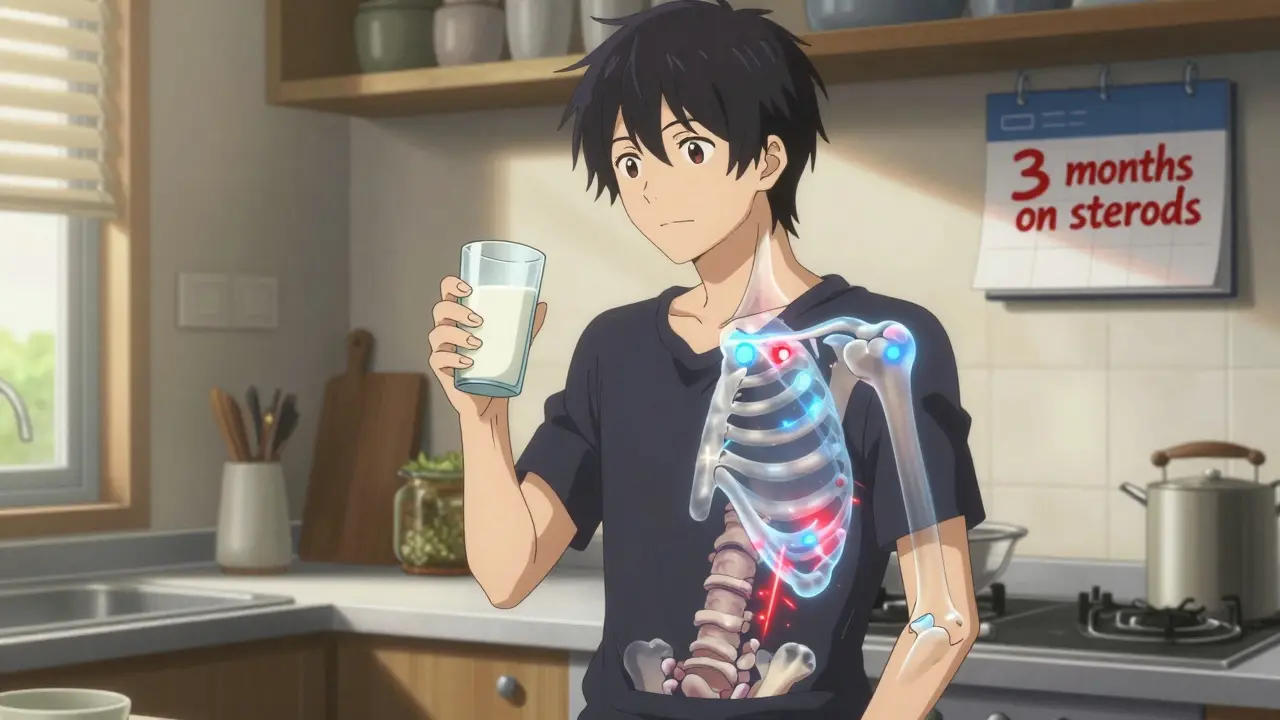
Step One: Calcium and Vitamin D-The Foundation
Before you even think about pills that stop bone loss, you need to give your bones the raw materials to stay strong. That means calcium and vitamin D. No exceptions. No "I’ll just eat more dairy." You need precise amounts.The American College of Rheumatology says everyone starting long-term steroids (3 months or longer at 2.5 mg prednisone or more) should take 1,000 to 1,200 mg of calcium daily. That’s not a suggestion-it’s a requirement. You can get it from food-yogurt, cheese, fortified plant milks, leafy greens-but most people need supplements to hit that target.
Vitamin D is just as critical. Your body needs it to absorb calcium. Without enough, calcium just passes through you. The guidelines recommend 600 to 800 IU per day. But if your blood test shows vitamin D below 30 ng/mL (which is common, especially in winter), you’ll need 800 to 1,000 IU daily. Some people need even more, especially if they’re older, overweight, or have darker skin. A simple blood test can tell you where you stand.
Don’t skip this step. Even if you take a powerful drug later, without calcium and vitamin D, it won’t work as well. Think of it like trying to build a house without bricks. The tools matter-but you still need the materials.
Step Two: Bisphosphonates-The First-Line Defense
If you’re on steroids long-term and you’re 40 or older, or you’ve had a fracture before, you need more than supplements. You need a medication that stops bone loss. That’s where bisphosphonates come in.These are the most studied, most proven drugs for steroid-induced bone loss. Alendronate (Fosamax) and risedronate (Actonel) are the most common. Both are taken once a week. They work by slowing down the bone-breakers (osteoclasts). In clinical trials, alendronate increased spine bone density by 3.7% in just one year-while the placebo group lost bone. Risedronate cut vertebral fracture risk by nearly 70%.
They’re not perfect. You have to take them right. Take them first thing in the morning, on an empty stomach, with a full glass of water. Stay upright for at least 30 minutes. Don’t lie down. Don’t eat or drink anything else for 30 minutes. Skip this, and you risk serious irritation to your esophagus. About 1 in 5 people have trouble with this. That’s why many switch to the yearly IV version: zoledronic acid.
Zoledronic acid is given once a year as a 15-minute infusion. It’s more effective than oral versions at preserving hip bone density and improves adherence-because you don’t have to remember a weekly pill. In one study, patients on zoledronic acid had 41% fewer hip fractures compared to placebo. It’s also safer for people with kidney issues, as long as their kidney function isn’t severely low.
When Bisphosphonates Aren’t Enough
Not everyone responds the same. If you’ve already had a fracture, your T-score is below -2.5, or you’re on high-dose steroids for more than a year, bisphosphonates might not be enough. That’s when doctors turn to teriparatide (Forteo).Teriparatide is different. Instead of slowing bone loss, it actually builds new bone. It’s a synthetic version of part of your natural parathyroid hormone. You inject it daily under the skin. It’s expensive-about $2,500 a month-and only approved for two years of use. But in the ACTIVE study, it cut new spine fractures from 6.1% to just 0.6% compared to alendronate. That’s a massive difference.
It’s not for everyone. You can’t use it if you’ve had radiation to your bones, Paget’s disease, or bone cancer. And while it’s safe in humans, there’s a black box warning because it caused bone tumors in rats. But after 15 years of real-world use, no such risk has been found in people.
Another option is denosumab (Prolia), given as a shot every six months. It reduces spine fracture risk by 79%. It’s great for people who can’t take bisphosphonates due to kidney problems or stomach issues. But it has a catch: if you stop it, you can lose bone fast. So you can’t just quit-it needs to be replaced with another drug, like a bisphosphonate.
Who Gets Treatment-and Who Doesn’t
Here’s the hard truth: most people on steroids don’t get the bone protection they need. A 2021 study of over 150,000 patients found only 19% received any kind of osteoporosis prevention within three months of starting steroids. That’s not because doctors don’t know better. It’s because the system fails. Patients don’t get tested. They don’t get warned. They don’t get follow-up.The guidelines are clear. If you’re 40 or older and taking ≥2.5 mg prednisone daily for ≥3 months, you should get a bone density scan (DXA) and start treatment. If you’re under 40 but have had a fracture before, or you smoke, have low body weight, or take other bone-weakening drugs, you still qualify.
But here’s what many don’t realize: you need to get scanned again after one year. If your bone density drops more than 5%, you need to switch or upgrade your treatment. Many people get one scan and think they’re done. They’re not.
What to Watch Out For
No drug is without risk. Bisphosphonates carry a tiny chance of atypical femur fractures-about 1 in 10,000 people per year. That’s rare, but real. If you get new thigh or groin pain that doesn’t go away, tell your doctor. It could be a warning sign.Another rare issue is osteonecrosis of the jaw-bone death in the jaw. It’s extremely uncommon with oral bisphosphonates (less than 1 in 10,000), but more likely if you’re getting dental work while on the drug. Always tell your dentist you’re on steroids and a bisphosphonate. They may delay major procedures until you’ve been off the drug for a while.
Teriparatide’s main risk is its cost and the fact that you can only use it for two years. After that, you need to switch to something else-usually a bisphosphonate-to keep the gains.
What’s Next? The Future of Bone Protection
New drugs are coming. Abaloparatide, approved in 2022, is similar to teriparatide but may build bone even better. And researchers are now testing sequences: start with teriparatide to rebuild, then switch to zoledronic acid to maintain. Early results suggest this combo could give you more bone density than either drug alone.But for now, the best approach is still simple: start early, use what works, and stick with it. Calcium and vitamin D are non-negotiable. Bisphosphonates are the go-to for most people. Teriparatide is the upgrade for those at highest risk. And regular monitoring? That’s your safety net.
Don’t wait for a fracture to realize your bones are in trouble. If you’re on steroids, talk to your doctor now. Get your bone density tested. Start the right supplements. Ask if you need a bisphosphonate. It’s not just about feeling well-it’s about staying strong enough to live well for years to come.
Can you reverse steroid-induced osteoporosis?
You can’t fully reverse it, but you can stop it from getting worse-and even rebuild some bone. Bisphosphonates prevent further loss. Teriparatide can actually increase bone density by up to 16% in the spine over 18 months. The key is starting early. The longer you wait, the harder it is to recover lost bone.
Do I need a bone scan if I feel fine?
Yes. Steroid-induced bone loss happens without pain or symptoms. You won’t feel your bones thinning. A DXA scan is the only way to know your bone density. Guidelines recommend one at the start of long-term steroid therapy and again after 12 months. If your bone density drops more than 5%, your treatment plan needs to change.
Can I just take more calcium instead of a bisphosphonate?
No. Calcium and vitamin D are essential, but they’re not enough on their own if you’re on long-term steroids. Studies show that supplements alone don’t prevent bone loss or fractures in this group. Bisphosphonates or other medications are needed to actively block the bone breakdown caused by steroids.
Are bisphosphonates safe for people with kidney problems?
Oral bisphosphonates like alendronate should be avoided if your kidney function is below 30 mL/min. For mild to moderate kidney issues (eGFR 30-50), your doctor may reduce the dose. If your kidneys are severely impaired, IV zoledronic acid or denosumab are safer options. Always get your kidney function checked before starting any osteoporosis drug.
How long do I need to take these medications?
It depends. For most people, treatment lasts 3-5 years. After that, your doctor will reassess your bone density and fracture risk. If your risk is still high, you may continue. If it’s low, you might stop. Teriparatide is limited to two years. Zoledronic acid can be given yearly for several years. Never stop abruptly without medical advice-especially with denosumab.
What if I can’t afford bisphosphonates?
Generic alendronate and risedronate cost as little as $10-$25 a month in the U.S., and even less in countries with public healthcare. If you’re struggling with cost, talk to your doctor or pharmacist. Many pharmaceutical companies offer patient assistance programs. Calcium and vitamin D supplements are inexpensive and should be taken regardless of your ability to pay for stronger drugs.




Comments
Man, I wish someone told me this when I was on prednisone for my asthma. I thought popping a few calcium gummies was enough. Turns out I was just feeding my bones junk food. Got a spine fracture at 38. Never again. Start the supplements early, get the scan, don't be dumb.
so like... if you're on steroids you're basically just waiting for your skeleton to give up? that's wild. i thought it was just about weight gain and mood swings. turns out your bones are doing the silent scream thing. yikes.
Most people don't realize that even 2.5mg/day of prednisone triggers bone loss. The ACR guidelines are clear, but primary care docs still treat it like a suggestion. I've seen patients on 10mg for two years with zero bone density screening. That's not negligence-it's systemic failure.
OMG this is so important!! 🙌 I’m on low-dose steroids for lupus and I just got my DXA scan-T-score of -2.8. I thought I was fine because I didn’t feel any pain. Turns out my bones were screaming and I was too busy scrolling TikTok to hear them. Going to ask my rheum about zoledronic acid now!! 💪
Why are we even talking about this? In America we just take pills for everything. You want strong bones? Lift weights. Eat meat. Stop being weak. This whole osteoporosis thing is just another way for Big Pharma to sell you expensive junk.
nah bro this is all lies. my uncle in Lagos took steroids for 10 years and he still lifts 100kg. you just scared of the truth. bones don't break if you eat yam and pray hard. this is western fear-mongering.
why do they even make these drugs if they dont work? i mean like i took alendronate and still broke my wrist falling off my bike so what was the point? i think this whole thing is a scam
Let me break this down simply: Calcium and Vitamin D are the foundation-no ifs, ands, or buts. If you’re on long-term steroids, skipping them is like trying to build a house with no nails. Bisphosphonates? They’re not magic, but they’re the most proven tool we have. Zoledronic acid is a game-changer for people who can’t swallow pills or have kidney issues. And yes, you need follow-up scans. One scan isn’t enough. Bone density changes. Your treatment should too. Don’t treat this like a checklist. Treat it like your future mobility.
In India, many don’t even know what a DXA scan is. My cousin’s father was on steroids for rheumatoid arthritis for 4 years and never got tested. Broke his hip at 58. We need better awareness here. This info should be in every clinic pamphlet, not just hidden in medical journals.
Ugh. Another overwrought, fear-driven medical essay. People need to stop treating their bodies like fragile porcelain. If you're on steroids, maybe you should reconsider your diagnosis. Or just stop being so dependent on pharmaceuticals. This whole osteoporosis panic is just another way to monetize anxiety.
Thanks for laying this out so clearly. I’ve been on 5mg prednisone for 18 months and just got my first DXA scan last week. T-score -2.4. I’m starting alendronate next week. I didn’t know about the 30-minute upright rule-thank you. Also, I didn’t realize generic risedronate costs less than my coffee subscription. That’s a no-brainer.
The way steroids hijack osteoblasts and osteoclasts is terrifyingly elegant-like a biological sabotage. What’s even more chilling is how silent it is. No pain, no warning, just gradual structural collapse. And yet, we have tools to fight it. Calcium, vitamin D, bisphosphonates-they’re not glamorous, but they’re the unsung heroes of bone survival. This isn’t just medicine. It’s a quiet rebellion against decay.
i just started steroids last month and already feeling tired but didn't know about bones. gonna ask my doc about calcium and scan. thanks for the heads up ❤️
How can you trust Western medicine when they keep changing their guidelines? One year they say bisphosphonates are safe, next year they say they cause jaw death. And now teriparatide? It caused tumors in rats! Why are we experimenting on humans? We should be using traditional herbs like ashwagandha and turmeric. That’s what my grandmother did.
Replying to @6616: The rat tumor data is from a 20-year-old study using doses 100x higher than human use. No human case has ever shown that. Teriparatide is FDA-approved, studied in over 10,000 patients, and has saved thousands from spinal fractures. Ashwagandha might help with stress, but it doesn’t rebuild bone. Don’t confuse natural with effective.