Blood Thinner Side Effects: What You Need to Know Before It's Too Late
When you take a blood thinner, a medication that reduces your blood’s ability to form clots. Also known as anticoagulant, it’s prescribed to prevent strokes, heart attacks, and dangerous clots in your legs or lungs. But these drugs don’t just stop bad clots—they also make normal bleeding harder to control. That’s why understanding blood thinner side effects isn’t optional. It’s survival.
Not all bleeding is obvious. A cut that won’t stop, nosebleeds that last more than 10 minutes, or bruising without injury are red flags. But the real danger is internal bleeding—like blood in your stool, vomit that looks like coffee grounds, or sudden headaches that feel different than any you’ve had before. These aren’t just side effects. They’re emergencies. And they happen more often than people realize. A 2023 study in the Journal of the American Heart Association found that nearly 1 in 10 people on long-term anticoagulants had a major bleed within two years. Most didn’t see it coming.
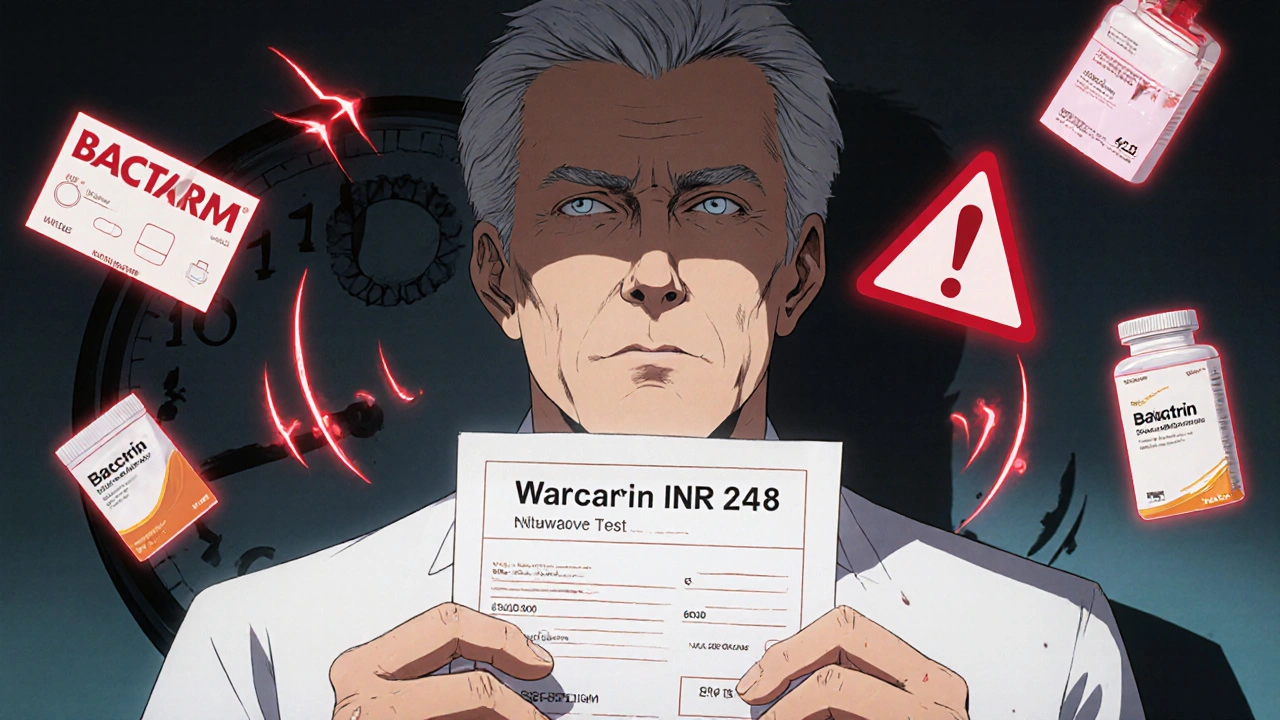
There are different kinds of blood thinners, and each has its own risks. Warfarin, an older anticoagulant that requires regular blood tests. Also known as Coumadin, it interacts with food, alcohol, and other meds, making it tricky to manage. Newer drugs like DOACs (direct oral anticoagulants)—including apixaban, rivaroxaban, and dabigatran—don’t need constant monitoring, but they still carry bleeding risks, especially if you’re over 75, have kidney issues, or take NSAIDs like ibuprofen. Even a simple fall can turn dangerous. One person on a DOAC might walk away from a bump on the head. Another might end up in surgery because of a slow brain bleed.
What most people don’t realize is that side effects don’t just happen overnight. They build up. A little extra bruising here, a bit more fatigue there, a weird feeling in your stomach—these aren’t "just aging." They’re signals. Ignoring them doesn’t make them go away. It just makes treatment harder. And if you’re on blood thinners because of atrial fibrillation, a past clot, or a mechanical heart valve, the stakes are even higher. You can’t afford to guess.
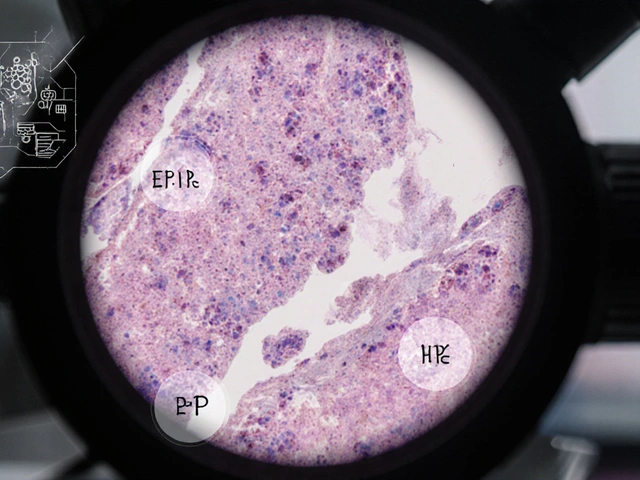
Some side effects are rare but deadly. Like methemoglobinemia from prilocaine (yes, even local anesthetics can interfere), or severe drops in platelets from certain drugs. Others are more common: dizziness, nausea, or feeling unusually cold. None of these should be shrugged off. Your pharmacist isn’t just there to hand out pills. They’re your first line of defense when something feels off.
This collection of posts doesn’t just list side effects. It shows you how to spot the quiet warnings, what tests to ask for, when to rush to the ER, and how to talk to your doctor without sounding paranoid. You’ll find real stories from people who thought it was just a bad day—until it wasn’t. You’ll learn what’s normal, what’s dangerous, and what to do next. No fluff. No fearmongering. Just clear, practical steps you can use today to protect yourself.
Warfarin and antibiotics can dangerously interact, raising bleeding risk. Learn which antibiotics are high-risk, when to check your INR, and how to safely manage both without stopping either medication.
Read more