Over a third of adults over 65 struggle with insomnia-not just tossing and turning, but waking up too early, unable to fall back asleep, or spending hours lying awake. It’s not just annoying; it’s dangerous. Poor sleep in older adults links directly to falls, memory problems, and even long-term disability. Yet, many still get prescribed sleeping pills that were never meant for their bodies. The truth? The safest options aren’t the ones you hear about on TV. They’re quieter, older, and often cheaper.
Why Old-School Sleep Pills Are Risky for Seniors
For decades, doctors reached for benzodiazepines like lorazepam or z-drugs like zolpidem (Ambien) when an older patient couldn’t sleep. These drugs work fast. But they also slow down brain activity too much. In older adults, that means dizziness, confusion, and a much higher chance of falling. One study found seniors on these medications had a 50% greater risk of hip fractures. Another showed they were 1.6 times more likely to fall overall. And it’s not just falls. These drugs can blur memory, make confusion worse in people with early dementia, and even cause sleepwalking or eating while asleep-without remembering it. The American Geriatrics Society flagged this back in 2012. They said: stop using benzodiazepines and z-drugs as first-line treatment for older adults. The risks outweigh the benefits. Yet, in 2023, nearly half of all insomnia prescriptions for Medicare patients were still for these high-risk drugs. Why? Because they’re familiar. Because patients ask for them. And because many doctors haven’t been trained on the safer alternatives.The Newer, Safer Options
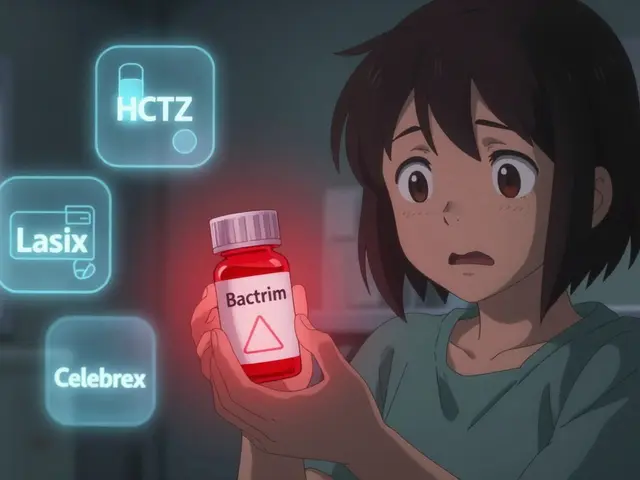
Two newer classes of sleep meds have changed the game: orexin receptor antagonists and low-dose doxepin. They don’t slam the brakes on your brain. They gently nudge it toward sleep. Lemborexant (Dayvigo) and suvorexant (Belsomra) block orexin, a brain chemical that keeps you awake. Think of it like turning down the volume on your brain’s alert system instead of knocking it out cold. Lemborexant, approved in 2019, has been studied in adults over 65 for up to a year. Results show it helps people fall asleep 15 minutes faster, stay asleep 21 minutes longer, and sleep 43 minutes more total-without the next-day grogginess that plagues older users of Ambien. In one survey, 72% of seniors using lemborexant reported being satisfied. The downside? Cost. Without insurance, it can run $750 a month. Low-dose doxepin (Silenor) is different. It’s the same drug used for depression-but at a tiny dose: 3 to 6 mg. At this level, it doesn’t affect mood. It only blocks histamine, a chemical that wakes you up. It’s FDA-approved specifically for sleep maintenance insomnia-meaning it helps you stay asleep, not just fall asleep. A 2024 study showed it improved sleep efficiency more than any other medication tested. Patients report feeling rested, not drugged. Only 12% of users on 3mg experienced next-day drowsiness. And it costs about $15 a month as a generic.Melatonin and Ramelteon: Gentle Starters
If you wake up too early and can’t fall back asleep, your body might not be making enough melatonin. That’s normal with age. Controlled-release melatonin (2mg) mimics your body’s natural sleep hormone pattern. It’s not a sedative. It’s more like a signal: “It’s time to wind down.” Studies show it helps people fall asleep about 10 minutes faster and adds 20 minutes of sleep total. It’s safe, cheap, and has almost no side effects. Ramelteon (Rozerem) works the same way but targets melatonin receptors more directly. It’s not strong enough to help you stay asleep all night, but it’s excellent for falling asleep faster-especially if you’re up late because your internal clock is off. A 2016 review found it reduced sleep onset time by nearly 10 minutes. Its biggest plus? Zero risk of dependence, no next-day fog, and no interaction with other meds. It’s ideal for seniors who just need a nudge to start sleeping.
What to Avoid
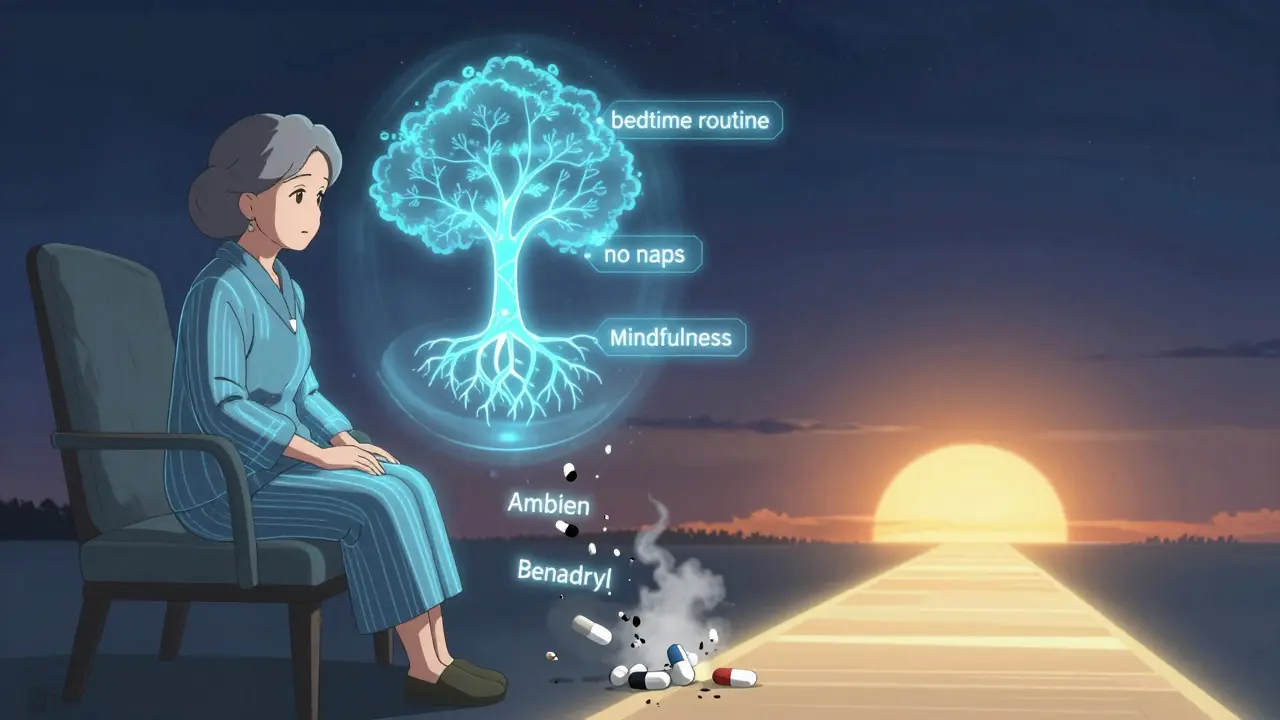
Even if a doctor says it’s “safe,” steer clear of these:- Benzodiazepines (lorazepam, diazepam, temazepam): High fall risk, memory fog, dependency.
- Z-drugs (zolpidem, eszopiclone, zaleplon): Still linked to sleepwalking, confusion, and increased fracture risk.
- Sedating antihistamines (diphenhydramine, doxylamine): Found in OTC sleep aids like Tylenol PM or Benadryl. They’re old, poorly studied in seniors, and can cause urinary retention, dry mouth, and worsen dementia symptoms.
- Tricyclic antidepressants (amitriptyline, nortriptyline): Used off-label for sleep, but they raise heart rhythm risks and cause dizziness.
These aren’t just outdated-they’re dangerous for older bodies. Your liver and kidneys don’t clear them as efficiently. Even small doses can build up and cause problems.
Non-Medication First
Before any pill, try Cognitive Behavioral Therapy for Insomnia (CBT-I). It’s the gold standard. It doesn’t involve drugs. It teaches you how to fix your sleep habits: limiting time in bed, avoiding naps, managing racing thoughts, and resetting your internal clock. Studies show it works better than pills for older adults-and the effects last longer. Yet, only 22% of seniors with insomnia are ever offered it. Most doctors don’t know where to refer them. But if you can access a CBT-I program-even online-it’s the smartest move you can make.How to Talk to Your Doctor
If you’re on a sleeping pill now and feel groggy in the morning, or you’ve had a near-fall, bring this up. Say: “I’m worried about the risks. Are there safer options?” Ask for:- A sleep diary review (track bedtimes, wake times, nighttime awakenings)
- A fall risk test (Timed Up and Go test)
- A cognitive screen (MoCA test)
- Lab work to check liver and kidney function
Then ask: “Could we try low-dose doxepin or ramelteon first? Or start with CBT-I?”
Many seniors are told, “Just take this pill.” But you have the right to ask for safer, evidence-based options. Don’t settle for a drug that makes you feel worse the next day.
Real Stories, Real Results
One 71-year-old woman in Florida switched from zolpidem to 3mg doxepin after falling twice. She said: “I slept through the night for the first time in years. No morning fog. No dizziness. I feel like myself again.” A 68-year-old man in Ohio tried lemborexant after years of poor sleep. He paid $700 a month out of pocket. “It worked,” he said. “But I couldn’t keep it up. I switched to melatonin and CBT-I. Now I sleep fine without spending half my pension.” These aren’t outliers. They’re examples of what’s possible when you choose safety over speed.What’s Coming Next
New drugs are on the horizon. Danavorexton, an orexin agonist, is in late-stage trials and may offer even better safety for seniors by helping the brain wake up naturally-instead of just forcing sleep. But even if it arrives, the real breakthrough isn’t a new pill. It’s changing how we think. Sleep isn’t something you drug yourself into. It’s something you rebuild, gently, with time and the right tools.For older adults, the goal isn’t to sleep like a 30-year-old. It’s to sleep safely, wake refreshed, and stay independent. That’s not asking too much.
What’s the safest sleeping pill for seniors?
The safest options are low-dose doxepin (3-6mg) and ramelteon (8mg). Both have minimal risk of falls, confusion, or next-day drowsiness. Lemborexant is also safe but much more expensive. Avoid benzodiazepines, z-drugs like Ambien, and OTC antihistamines like Benadryl.
Can seniors take melatonin safely?
Yes. Controlled-release melatonin (2mg) is safe for seniors and helps with falling asleep faster. It doesn’t cause dependency or grogginess. It’s not a strong sedative, so it won’t help if you wake up in the middle of the night-but it’s perfect for those who struggle to fall asleep at the start of the night.
Why are benzodiazepines dangerous for older adults?
Benzodiazepines slow brain activity too much in older adults, increasing the risk of falls, hip fractures, confusion, and memory problems. Studies show they raise fall risk by 50-60%. They also build up in the body because the liver and kidneys process them slower with age. The American Geriatrics Society recommends avoiding them entirely for insomnia in seniors.
Is CBT-I really better than medication?
Yes. CBT-I is the most effective long-term treatment for insomnia in older adults. It improves sleep quality without side effects and the benefits last years after treatment ends. Medications only work while you’re taking them-and come with risks. Most seniors who try CBT-I see better results than with pills.
How can I get CBT-I if my doctor doesn’t offer it?
Look for online programs like Sleepio, CBT-I Coach (free app from the VA), or programs through local hospitals or senior centers. Many are covered by Medicare Advantage plans. Ask your doctor for a referral to a sleep psychologist. You don’t need to wait for your doctor to offer it-you can seek it out.
What should I do if I’m already on a sleeping pill?
Don’t stop suddenly. Talk to your doctor about switching to a safer option or starting CBT-I. Many seniors can reduce or stop sleep meds safely with a slow taper and support. Keep a sleep diary to track your progress. If you feel dizzy, confused, or unsteady, mention it immediately-those are red flags.
Next Steps for Seniors and Families
If you or a loved one is struggling with sleep:- Stop using OTC sleep aids like Benadryl or Tylenol PM.
- Start a sleep diary for one week: note bedtime, wake time, and how many times you woke up.
- Ask your doctor for a fall risk test and cognitive screen.
- Request CBT-I as the first option-before any pill.
- If a pill is needed, ask for low-dose doxepin or ramelteon.
- Check insurance coverage: generic doxepin is often under $20/month.
Sleep isn’t a luxury. It’s a pillar of health. For older adults, choosing the right path isn’t about finding the strongest drug-it’s about finding the safest one.






Comments
Bro, I just switched from Ambien to lemborexant after my hip almost said goodbye to me 😅. Now I sleep like a baby-no groggy mornings, no walking to the fridge at 3 a.m. (yes, that happened). Worth every penny if you can afford it. Also, CBT-I is the real MVP. No pills, no drama. Just sleep. 🙌
This is such a needed post. My mom was on lorazepam for years and no one ever told us the risks. She started falling constantly. We switched her to low-dose doxepin and it’s like night and day. She actually remembers our birthdays now. 🥹 Thank you for sharing this.
Been reading up on this since my dad got prescribed zolpidem last year. Turns out the doc didn't even know about the AGS guidelines. Scary stuff. I printed this out and gave it to his GP. Hope it sticks.
They don't want you to know this but Big Pharma is pushing these dangerous pills because they make billions. The real solution? Sleep in a dark room, no screens, and pray to the moon. They don't want you to know that melatonin is a natural hormone they could patent if they wanted to. 😡
So let me get this straight… we’re supposed to believe that a $750 pill is better than Benadryl? 😏 Meanwhile my grandma takes one Tylenol PM and sleeps like a log. Maybe she just has better genes? Or maybe we’re overcomplicating sleep like it’s rocket science.
I cried reading this. My aunt went from screaming at the ceiling at 2 a.m. to actually sleeping through the night after CBT-I. She said it felt like someone handed her back her life. No pills. No side effects. Just… peace. If you’re even slightly curious-just try it. You’ve got nothing to lose but sleepless nights.
It’s funny how we treat sleep like a broken machine you fix with a wrench. But sleep isn’t mechanical-it’s biological, emotional, spiritual. We’ve outsourced rest to pharmaceuticals because we’re too busy, too anxious, too disconnected. Maybe the real medicine isn’t a pill-it’s stillness. 🌿
Wait wait wait-so you’re saying we shouldn’t use diphenhydramine? But it’s in EVERYTHING! My neighbor’s dog takes it for anxiety! And my cousin’s 80-year-old uncle swears by it! You can’t just take away our little sleep helpers!! 😭
lol at people paying $700 for a pill when you can just drink chamomile tea and whisper ‘sleep now’ to your pillow. Also, CBT-I? Sounds like a cult. I’ll stick with my 50mg of Benadryl and my 3 a.m. Netflix binges. #Priorities
Anyone else notice how the ‘safe’ options are all brand-name and expensive? Meanwhile, the cheap stuff is labeled ‘dangerous’? Coincidence? Or is this just another way to push people toward insurance-dependent care? I’m not buying it.
Hey everyone-just wanted to say thank you to the OP for putting this together. This is the kind of info we need to spread like wildfire. I’m sharing this with my senior center. If you’re reading this and you’re a caregiver, a nurse, a family member-please, please, please-bring this up with your doctor. We can do better. We owe it to our elders.
I’m 73 and started CBT-I last month. I was skeptical. Now I’m sleeping 7 hours straight. No meds. No regrets. My husband says I’ve stopped moaning in my sleep. That’s a win. If you’re tired of being tired-you’ve got options. Start with the diary. Just one week. You won’t regret it.
they say melatonin is safe but what if it’s just a gateway? what if they’re slowly replacing our natural rhythms with synthetic signals? who even made these rules anyway? the FDA? big pharma? the sleep-industrial complex?? i don’t trust any of it…
My mom in India takes a 2mg melatonin tablet every night and says it’s the only thing that’s helped in 10 years. No side effects. No cost. Just quiet sleep. We need more of this kind of info globally-not just in the US. Thank you for writing this.