Medication Equivalence: What Makes Drugs Interchangeable and Safe
When you hear medication equivalence, the point at which two drugs produce the same clinical effect and safety profile in patients. Also known as therapeutic equivalence, it’s the quiet rule that lets pharmacies swap brand-name pills for cheaper generics without asking your doctor—every single day. But here’s the catch: not all drugs labeled as "equivalent" are created equal. Some substitutions work perfectly. Others? They can throw off your entire treatment plan.
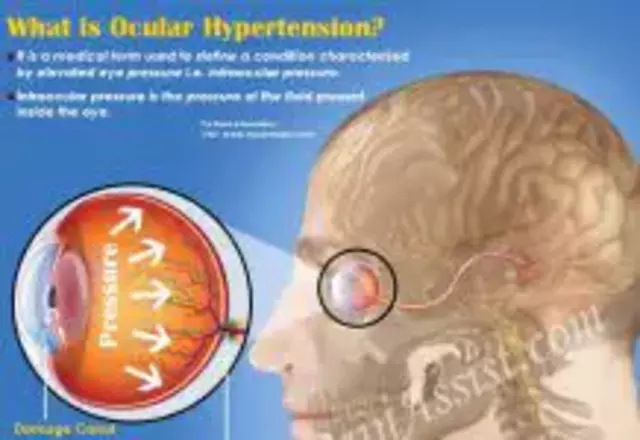
Generic drugs, chemically identical versions of brand-name medications approved by the FDA after patents expire make up over 90% of prescriptions in the U.S. But behind that number are real-world stories: someone switching from brand-name Lipitor to a generic atorvastatin and suddenly feeling dizzy, or a patient on warfarin whose INR spikes after a pharmacy change. Why? Because even tiny differences in fillers, coatings, or release timing can matter—especially for drugs with narrow therapeutic windows like seizure meds, thyroid pills, or blood thinners.
Biosimilar switching, the process of replacing a complex biologic drug with a highly similar but not identical version adds another layer. Unlike simple chemical generics, biosimilars like adalimumab or infliximab copies are made from living cells. They’re not exact duplicates. That’s why studies show some patients stop responding after a switch—not because the drug is bad, but because their body reacted to a subtle change in protein structure. The FDA says they’re safe. Real patients? They’ve learned to track every change.
Then there’s drug interactions, how one medication changes how another works in your body. Grapefruit juice turning statins toxic. Antibiotics making warfarin dangerous. Antifungals boosting cholesterol meds to harmful levels. These aren’t rare edge cases. They’re daily risks that can turn a simple switch into an emergency. Medication equivalence doesn’t mean "safe to swap"—it means "clinically similar under controlled conditions." Real life? It’s messier.
You might think all this is just pharmacy paperwork. But it’s not. It’s about whether your asthma inhaler works the same after a refill, if your hair loss treatment still helps after switching brands, or if your new generic antidepressant leaves you feeling flat. These aren’t theoretical concerns. People lose sleep over them. Families stress over them. Pharmacists spend hours explaining them.
The posts below cut through the noise. You’ll find real stories from people who’ve been through generic switches, biosimilar changes, and dangerous interactions. You’ll learn how to check if your meds are truly interchangeable, what to ask your pharmacist before accepting a substitute, and which drugs demand extra caution. No fluff. No jargon. Just what you need to know to stay safe, save money, and not get caught off guard by a pharmacy decision you never asked for.
Learn how to use travel health apps to find pharmacies and clinics abroad, translate medications, and connect with doctors overseas. Essential tools for safe, stress-free travel.
Read more