When your liver starts acting strange-fatigue that won’t quit, itchy skin, blood tests showing odd patterns-it’s easy to assume it’s just one problem. But sometimes, it’s not. In some people, the immune system attacks the liver in more than one way at once. This is called an autoimmune overlap syndrome. It’s not rare. It’s not theoretical. It’s real, and it changes how you treat the disease.
What Happens When Autoimmune Diseases Overlap?
Most people with autoimmune liver disease have one clear diagnosis: either Primary Biliary Cholangitis (PBC), Primary Sclerosing Cholangitis (PSC), or Autoimmune Hepatitis (AIH). But about 1 in 10 people with PBC or AIH show signs of both. That’s not a mistake. It’s not a misdiagnosis. It’s an overlap. PBC targets the small bile ducts inside the liver. The body makes antibodies-called AMA-that attack the mitochondria in those cells. That leads to bile backing up, scarring, and eventually cirrhosis. AIH, on the other hand, attacks the liver cells themselves. It causes inflammation right in the liver tissue, with high ALT and AST levels and antibodies like ANA or SMA. PSC is rarer and more aggressive, attacking the larger bile ducts, often linked to inflammatory bowel disease. The overlap most often seen is AIH-PBC. About 2% to 19% of people with PBC have features of AIH too. That means they have high ALP and AMA (classic PBC), but also high IgG, elevated ALT, and interface hepatitis on biopsy (classic AIH). It’s like having two different autoimmune diseases living side by side in the same organ.Why AIH-PBC Is the Most Common Overlap
You won’t find a true PBC-PSC overlap in the medical literature-not really. Case reports exist, but experts agree: there’s no clear pattern. The bile duct damage in PSC looks different from PBC. The immune triggers don’t line up. PSC is more about fibrosis and strictures; PBC is about duct destruction and AMA. AIH and PBC, though, share something important: they both happen more often in women, they both flare slowly, and they both respond to immune-suppressing drugs. That’s why they mix. A 2008 study of nearly 200 patients found that 8% had features of both. More recent data from the American Association for the Study of Liver Diseases confirms this trend: up to 7% of AIH patients show PBC markers. The real clue? Blood tests. If you have PBC but your ALT is sky-high instead of just mildly raised, or your IgG is climbing instead of staying normal, that’s a red flag. Same if you’re on ursodeoxycholic acid (UDCA) for PBC and your liver enzymes don’t improve. That’s not treatment failure-it’s a sign you might have AIH too.How Doctors Diagnose an Overlap
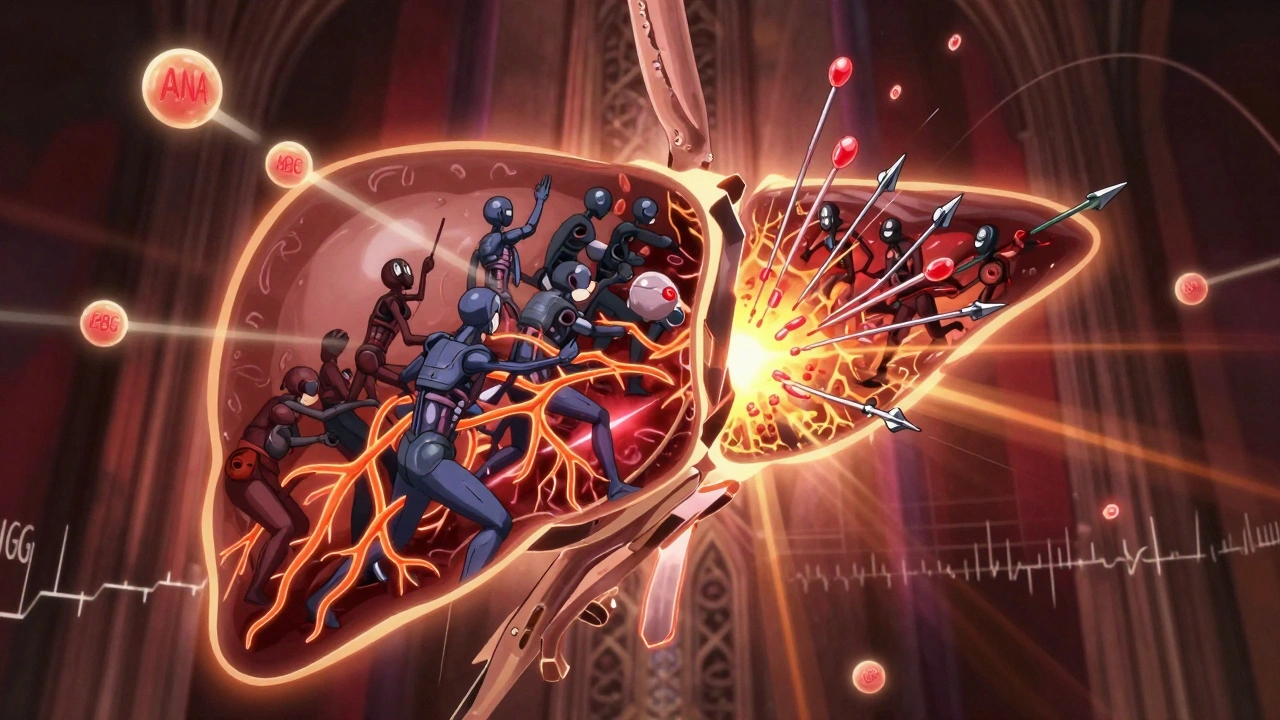
There’s no single test. No magic number. Diagnosis comes from stitching together four things: symptoms, blood work, antibodies, and liver biopsy. For PBC, you need two of these three: elevated ALP or γ-GT, positive AMA (or sp100/gp210 antibodies if AMA is negative), and biopsy showing bile duct damage. For AIH, the International Autoimmune Hepatitis Group scoring system looks at IgG levels, autoantibodies (ANA, SMA), and biopsy findings like interface hepatitis. An overlap diagnosis usually means meeting two or three criteria for each disease. Biopsy is key here. Many doctors skip it if AMA is positive and ALP is high-why bother? But in overlap cases, the biopsy tells the real story. You might see bile duct loss (PBC) right next to lymphocytic infiltration around liver cells (AIH). That’s the smoking gun. The problem? Most community doctors don’t look for this. AASLD estimates 15-20% of overlap cases get misdiagnosed as just one disease. That’s dangerous. Treating PBC alone with UDCA won’t fix the AIH part. And giving steroids to someone with pure PBC? Risky and unnecessary.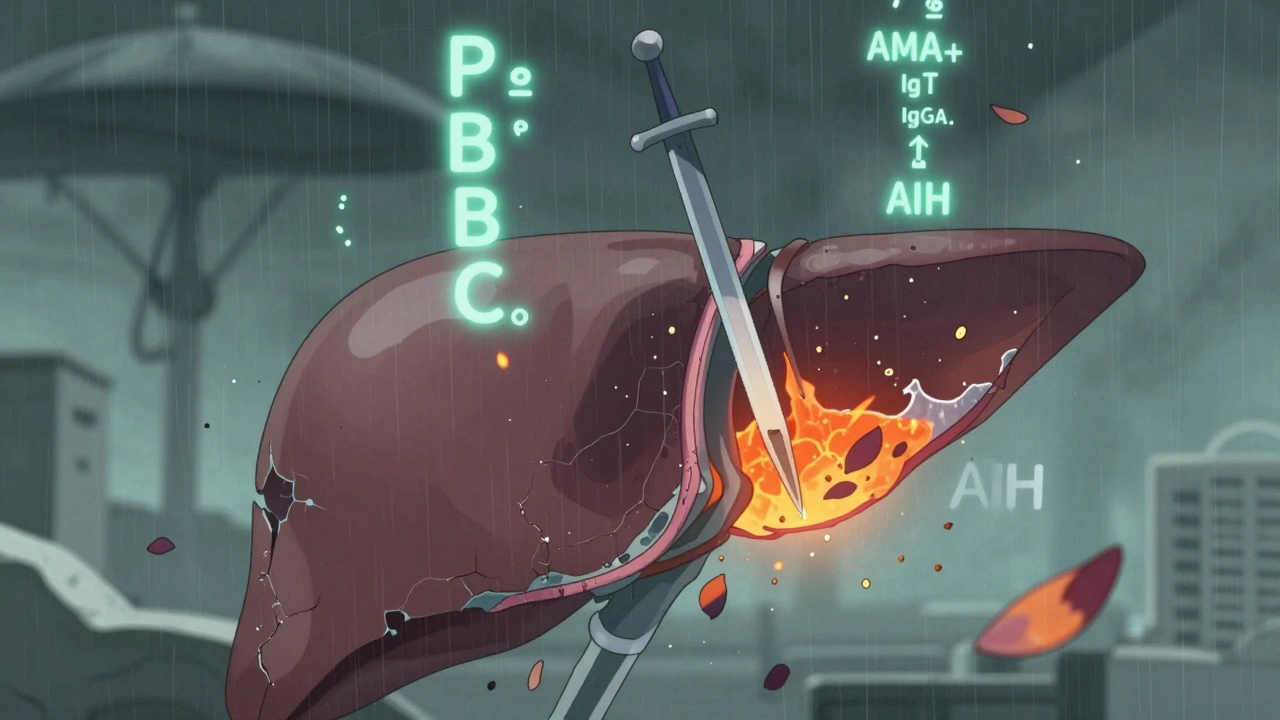
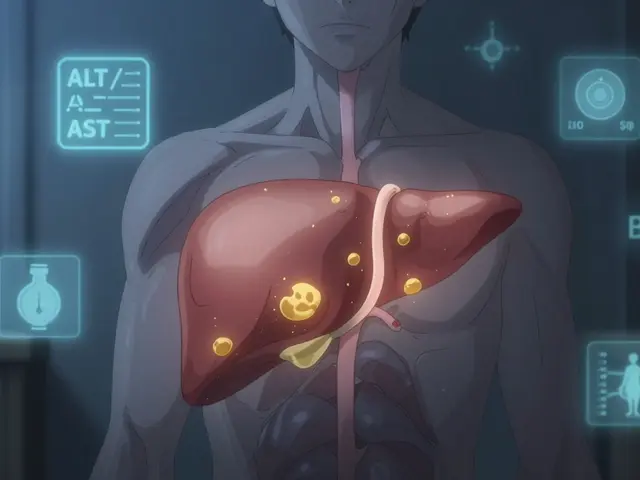
What Treatment Looks Like When Two Diseases Are at Play
PBC? UDCA is the gold standard. It slows progression, improves survival, and is well-tolerated. AIH? Steroids like prednisone, often paired with azathioprine, bring inflammation under control. But in overlap? Neither drug alone works well enough. About 30-40% of AIH-PBC patients don’t respond to UDCA alone. Their ALT stays high. Their IgG doesn’t drop. That’s when you add immunosuppressants. A 2020 case study followed a 39-year-old man with asymptomatic enzyme elevations for six years. He was diagnosed with PBC, started on UDCA, but his ALT kept creeping up. A biopsy showed interface hepatitis. He was started on low-dose prednisone. Within six months, his liver enzymes normalized. He’s now on a mix of both drugs-lifelong. Treatment isn’t one-size-fits-all. Some patients respond better to steroids first, then add UDCA. Others start with UDCA and add azathioprine if ALT doesn’t budge. The goal isn’t to cure-it’s to stop progression. Left untreated, 30-40% of overlap patients develop cirrhosis within 10 years.What About PSC? Is There Any Overlap?
PSC is the odd one out. It’s not just autoimmune-it’s also linked to Crohn’s disease and ulcerative colitis. The bile duct damage looks different. The immune markers don’t match PBC. Even though there are scattered case reports of people with both PSC and PBC features, experts like those at the World Journal of Gastroenterology say: no true overlap exists. Why? Because PSC doesn’t respond to steroids or UDCA the way AIH or PBC do. If someone has PSC and elevated AMA, it’s more likely they have two separate conditions-PSC and PBC-coexisting by chance, not because the immune system is attacking in two ways at once. That’s why most guidelines don’t recognize PBC-PSC or PSC-AIH as official overlap syndromes. They’re rare, poorly defined, and don’t respond to the same treatments. Focus stays on AIH-PBC-it’s the only one with clear diagnostic criteria and proven treatment strategies.
What You Should Watch For
If you have PBC and you’re feeling more tired than usual, or your skin is itchy even on UDCA, don’t brush it off. If your ALT or AST levels are rising, or your IgG is climbing, ask for a full autoimmune panel. Check for ANA, SMA, and IgG-not just AMA. If you have AIH and your ALP is high, or your liver biopsy shows bile duct damage, that’s another signal. Don’t assume it’s just inflammation. Ask if PBC could be hiding in plain sight. Symptoms like joint pain, muscle aches, or dry eyes and mouth can also point to overlap. These aren’t just random-they’re signs your immune system is running wild in multiple directions.The Bigger Picture: A Spectrum, Not Separate Boxes
The old way of thinking-PBC, AIH, PSC as three clean categories-is fading. Experts now see autoimmune liver disease as a spectrum. Some people have pure PBC. Others have pure AIH. But many fall in between. Overlap syndromes aren’t anomalies-they’re proof that the immune system doesn’t follow our labels. That’s why research is shifting. The European Association for the Study of the Liver and the International Autoimmune Hepatitis Group are working on new, validated diagnostic criteria for overlap syndromes. Early data from 2024 suggests we’ll soon have clearer guidelines for when to test, when to biopsy, and when to combine treatments. For now, the message is simple: if your liver disease doesn’t fit neatly into one box, it might be because it’s sitting right on the line between two. Don’t settle for a single diagnosis if the data doesn’t add up. Push for the full picture. Your liver depends on it.Can you have both PBC and AIH at the same time?
Yes. AIH-PBC overlap is the most common autoimmune liver disease overlap. It happens in 2% to 19% of people with PBC and up to 7% of those with AIH. You’ll see signs of both: AMA and high ALP from PBC, plus elevated IgG, ANA, and interface hepatitis from AIH. Treatment usually requires both UDCA and immunosuppressants.
Is PBC-PSC overlap real?
No, not in the clinical sense. While rare case reports exist, experts agree there’s no consistent pattern or diagnostic criteria for PBC-PSC overlap. The bile duct damage in PSC is different from PBC, and the immune markers don’t align. Most doctors consider these separate conditions occurring together by chance, not a true overlap syndrome.
How is an overlap syndrome diagnosed?
Diagnosis requires combining four elements: clinical symptoms, blood tests (like ALP, ALT, IgG, AMA, ANA), autoantibody profiles, and a liver biopsy. Meeting two or three diagnostic criteria for both PBC and AIH is the current standard. A biopsy showing bile duct loss alongside interface hepatitis is often the key to confirming the overlap.
What happens if overlap syndrome is missed?
If you’re only treated for one disease-say, PBC with UDCA-you might not control the AIH component. That means ongoing liver inflammation, rising enzymes, and faster progression to cirrhosis. Studies show up to 40% of untreated overlap patients develop cirrhosis within 10 years. Early detection and dual therapy can stop that.
Are there new treatments for autoimmune overlap syndromes?
Current treatment still relies on combining UDCA for PBC and corticosteroids or azathioprine for AIH. But research is underway. New autoantibodies like sp100 and gp210 are helping diagnose AMA-negative PBC cases. Clinical trials are testing targeted biologics, and new diagnostic criteria are being validated by EASL and AASLD. The goal is personalized treatment based on which features dominate.






Comments
Been dealing with this for years - my ALP was high, AMA positive, but ALT kept climbing. Docs kept saying it’s just PBC. Biopsy finally showed interface hepatitis. Turned out to be AIH-PBC overlap. Started on UDCA + azathioprine. Enzymes normalized in 4 months. If you’re not getting better on UDCA alone, push for a biopsy. Don’t let them dismiss it.
Most of these so-called ‘overlap syndromes’ are just lazy diagnostics. You don’t need a biopsy if your AMA is positive and ALP is elevated. Stop overcomplicating things with fancy immunology. In India, we treat what we see - not what some American journal says.
Let’s be real - the liver doesn’t care about our diagnostic boxes. It just screams when it’s under attack. AIH-PBC overlap isn’t a curiosity - it’s a wake-up call that autoimmunity is messy, dynamic, and deeply personal. The fact that we’re still arguing over whether it’s ‘real’ is why patients suffer. We need to treat the patient, not the label.
Of course they’re pushing overlap syndromes - it’s how pharma makes more money. UDCA + steroids? That’s two expensive drugs instead of one. And don’t get me started on biopsies - they’re invasive, risky, and often misread. They’re selling fear disguised as science.
Did you know the AMA antibody test was only standardized in the 90s? Before that, half the PBC cases were misdiagnosed as ‘chronic hepatitis.’ Now they’re inventing overlap syndromes to justify more tests. I’ve seen 3 patients with ‘overlap’ - all had viral hepatitis that was missed. The real culprit? Poor screening. Not autoimmune chaos.
So… if someone has PBC and suddenly develops interface hepatitis, is that a new disease or just the immune system getting bored? Because honestly, if my liver started throwing a tantrum with two different attack plans, I’d be impressed. And slightly terrified.
Let’s be brutally honest: 90% of community hepatologists don’t know what interface hepatitis looks like. They see AMA+, ALP+, and they check ‘PBC’ and move on. Biopsy? Too expensive. Too much work. Too inconvenient. So patients get half-treated - and then wonder why they’re cirrhotic in 5 years. This isn’t medicine. It’s negligence dressed up in white coats.
I’ve worked with patients across the UK and Southeast Asia - and I’ve seen this pattern repeat. The overlap isn’t just clinical. It’s cultural. In places with limited access to advanced diagnostics, patients are left with incomplete answers. We need global awareness, not just academic debates. Knowledge shouldn’t be a privilege.
If you’re on UDCA and your ALT hasn’t budged in 6 months - stop waiting. Ask for IgG, ANA, SMA. Request a biopsy. Don’t let anyone tell you it’s ‘just PBC.’ You’re not being difficult - you’re being your own best advocate. Your liver doesn’t have a second chance. Neither do you.
Just got my biopsy results back - bile duct loss AND lymphocytic infiltration. My GI doc said, ‘That’s unusual.’ I said, ‘That’s the overlap.’ He called the liver specialist. Two days later, I was on steroids. I’m not cured - but I’m not dying either. This isn’t theoretical. It’s my liver. And it’s real.
My cousin had this. Told the doc her skin was itching like crazy. Doc said, ‘Take antihistamines.’ She went to a specialist 6 months later. Biopsy showed overlap. Now she’s on two meds. Still tired, but alive. Don’t wait. Push. Ask. Repeat.
I’ve seen this in my practice - patients who were told they had ‘just’ PBC, then ended up needing transplant because no one checked for AIH markers. It’s not about being right. It’s about being thorough. We owe our patients more than a checkbox diagnosis.
What fascinates me is how the immune system orchestrates this - not with a single target, but with layered, overlapping assaults. It’s like a symphony where two instruments are playing different scores in the same key. We’re only beginning to understand the harmony - and dissonance - of autoimmune disease. This isn’t noise. It’s a message.
OMG I had this!! My doctor said I had PBC, but my joints were killing me and my IgG was through the roof. I went to a second doctor and begged for a biopsy - and guess what? Interface hepatitis!! Now I’m on UDCA + azathioprine and I actually have energy again. I cried when they told me it wasn’t just ‘bad PBC’ - it was something we could treat. If you’re not getting better, don’t give up. Keep pushing. Your life depends on it!! 💪❤️🩺
Overlap syndrome? More like overlap scam. All this ‘biopsy needed’ nonsense is just to pad hospital bills. AMA positive + ALP high = PBC. End of story. Stop wasting money on useless tests. If you’re not jaundiced, you’re fine.