Rural Patients: Access, Medication Challenges, and Solutions
For rural patients, people living in remote or underserved areas who struggle to access timely medical care and medications. Also known as remote-area residents, they often travel dozens of miles just to fill a prescription or see a specialist. This isn’t just inconvenient—it’s dangerous. When the nearest pharmacy is 40 miles away and public transit doesn’t run on weekends, skipping a dose or delaying treatment becomes normal. A 2023 CDC study found that rural patients are 30% more likely to miss critical medications than urban ones, not because they don’t care, but because the system isn’t built for them.
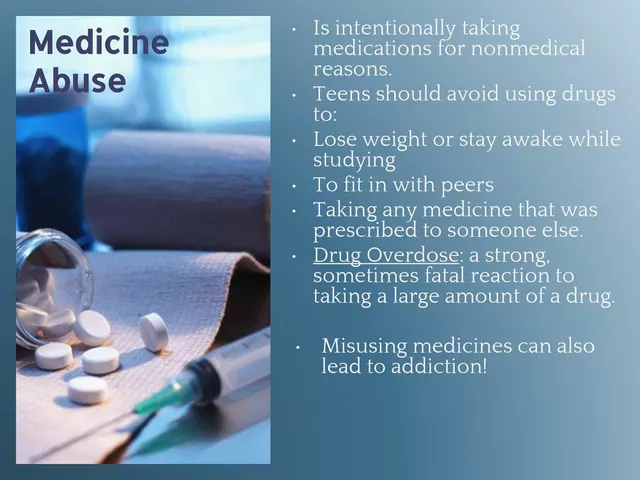
It’s not just about distance. pharmacy services, the system of dispensing, counseling, and managing medications through licensed professionals. Also known as community pharmacy care, it’s shrinking in rural areas. Over 1,200 rural pharmacies closed in the U.S. between 2010 and 2023. That means fewer pharmacists to explain how to use an inhaler, check for drug interactions, or help with prior authorizations. And when you’re managing asthma, diabetes, or warfarin, missing that face-to-face conversation can mean hospitalization. Then there’s medication access, the ability to obtain the right drugs at the right time without financial or logistical barriers. Also known as drug availability, it’s a daily battle for many rural families. Generics aren’t always stocked. Delivery services don’t cover all zip codes. And insurance networks rarely include the few clinics left in town. Meanwhile, healthcare disparities, systemic gaps in health outcomes between rural and urban populations due to resource inequality. Also known as rural health inequities, they show up in higher rates of uncontrolled hypertension, missed cancer screenings, and preventable ER visits.
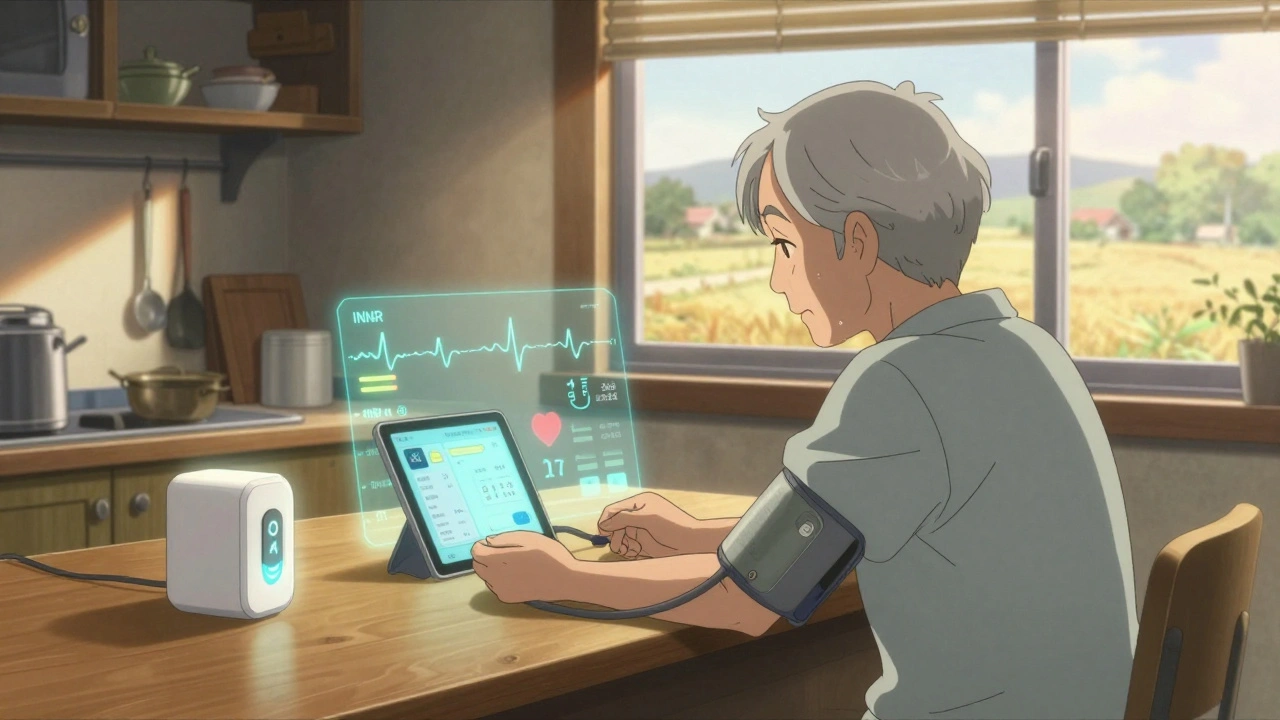
But change is happening. telepharmacy, remote pharmacy services delivered via video or digital platforms to connect patients with licensed pharmacists. Also known as virtual pharmacy care, it’s helping fill the gaps. Patients in Montana or Mississippi can now get their meds reviewed, learn how to use an inhaler correctly, or get help switching to an authorized generic—all from their kitchen table. Apps now let rural patients find nearby clinics, check medication prices, or even verify if an online pharmacy is licensed. And with more focus on health literacy, simple tools like pictogram labels and voice-guided dosing apps are making it easier to take meds safely—even if you’ve never read a prescription bottle before.
What you’ll find below isn’t just a list of articles—it’s a toolkit. From how to keep insulin stable on a long drive to why generic switching matters more in rural areas, these posts give real answers to real problems. No fluff. No jargon. Just what rural patients and their families need to stay safe, informed, and in control of their health.
Telehealth strategies are helping rural and remote patients monitor medication side effects in real time, reducing hospitalizations and improving safety. Learn how tools like smart devices, AI, and pharmacist-led programs are closing the care gap.
Read more