In 2023, the FDA issued four warning letters for misclassified equipment changes in drug manufacturing. One mistake can halt production for months. For pharmaceutical companies, even small tweaks to how a drug is made can trigger major regulatory hurdles. These changes aren't just about updating equipment or processes-they're about ensuring patient safety and drug quality. Let's break down exactly what you need to know.
What Are Manufacturing Changes in Pharmaceuticals?
Pharmaceutical manufacturing changes are any modifications made to an approved drug product's composition, process, equipment, facilities, or quality controls after regulatory approval has been granted. This includes everything from swapping out a tablet press to changing the source of raw materials. The FDA the U.S. Food and Drug Administration, which oversees pharmaceutical manufacturing changes under 21 CFR 314.70 and 21 CFR 601.12 requires manufacturers to track these changes rigorously. Why? Because even minor adjustments can affect a drug's safety, strength, purity, or effectiveness. A change in the mixing speed of a vaccine could alter its shelf life. A new supplier for a raw ingredient might introduce impurities. The regulatory compliance system designed to ensure these changes don't compromise patient safety exists for one reason: to protect people taking these medications.
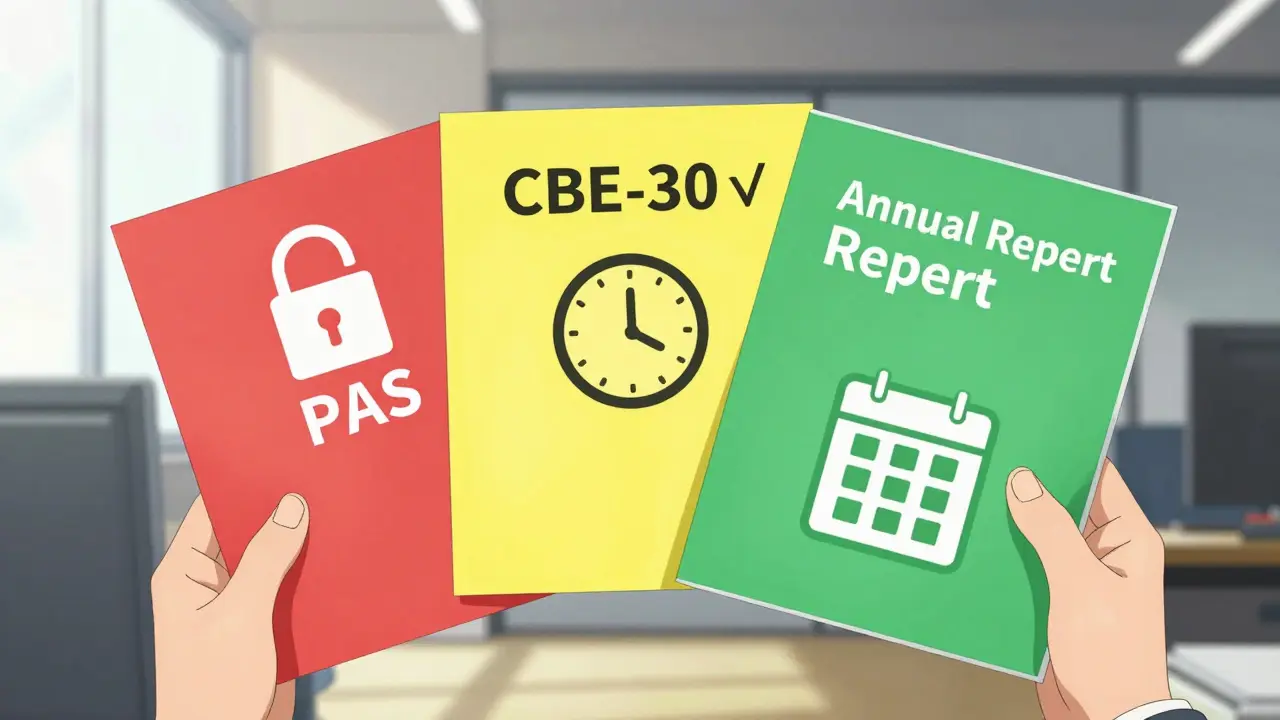
The FDA's Three-Tier System Explained
Under FDA regulations, changes fall into three categories based on risk. Prior Approval Supplement (PAS) is required for major changes that could significantly impact product quality, such as changing the synthesis route of an active ingredient or introducing a new manufacturing site for critical processes. These changes need FDA approval before any product is distributed. For example, if a company switches from a chemical synthesis method to a biotech process for a cancer drug, they must submit a PAS and wait for FDA sign-off.
CBE-30 is for moderate changes where the manufacturer can implement the change 30 days after submitting the notification. This includes replacing equipment with an equivalent model from the same manufacturer or adjusting a non-critical process parameter. A common example: swapping a tablet press with the same model from the same vendor. The company submits the CBE-30 form, then waits 30 days before using the new equipment.
Annual report covers minor changes with minimal risk, like changing the location of a non-critical step within the same facility. These are documented in the next annual report submitted to the FDA. For instance, moving a labeling station to a different part of the same production line without altering the process itself.
How Global Regulators Compare
| Regulatory Body | Change Type | Requirements | Example |
|---|---|---|---|
| FDA | Prior Approval Supplement (PAS) | Approval before distribution | Changing the synthesis route of an active ingredient |
| FDA | CBE-30 | Submit 30 days before distribution | Replacing tablet press with equivalent model |
| EMA | Type II | Full evaluation before implementation | Switching to a new bioreactor for monoclonal antibodies |
| EMA | Type IB | Approval before implementation | Modifying a sterilization process for injectables |
| Health Canada | Level I | Prior approval required | Changing the API supplier for a critical drug component |
| WHO | Comparability Protocol | Stability data and risk assessment | Adjusting equipment for a vaccine production line |
The European Medicines Agency (EMA) uses a different classification system, with Type II for major changes requiring full review before implementation, Type IB for moderate changes needing approval, and Type IA for minor changes notified after implementation. Health Canada's system is similar to the FDA's but with stricter timing for moderate changes. The WHO Prequalification program requires detailed comparability studies for any change affecting vaccine quality, including stability testing and bioequivalence data. This global patchwork means pharmaceutical companies must tailor their change management processes for each market.
Why Risk Assessment is Critical
Dr. Jane Axelrad, former FDA Deputy Center Director for Policy, explains: "The appropriate reporting category depends on the risk that the manufacturing change could have an adverse effect on the safety or effectiveness of the product." This risk assessment isn't just paperwork-it's the foundation of all change classification decisions. For example, replacing a mixer in a sterile injectable production line might seem minor, but if the new mixer alters particle size distribution, it could affect drug absorption. Experts like Dr. Mark Shearer emphasize that "comparability studies must demonstrate no impact on critical quality attributes through statistical analysis of critical quality data" to support change classifications.
Failure to properly assess risk leads to costly mistakes. In 2019, the FDA issued a warning letter to Apotex for misclassifying a major manufacturing change as moderate. The company changed a critical step in their drug synthesis without proper approval, risking product quality. This incident cost them months of production downtime and millions in lost revenue.

Common Pitfalls and Real-World Examples
One recurring issue is determining whether equipment changes are "equivalent." FDA's 2022 guidance clarifies that "equivalent" means same principle of operation, same critical dimensions, and same material of construction. But companies often skip this check. On Reddit's r/Pharmaceutical subreddit, a regulatory affairs specialist shared a story: "Classifying a tablet press replacement as CBE-30 versus PAS consumed 37 hours of cross-functional team time due to ambiguous API particle size specifications." The team had to run extra tests to confirm the change didn't affect critical quality attributes.
Documentation is another weak spot. FDA's Manufacturing Site Change Supplements guidance requires facility diagrams, process validation reports, and comparative batch data for at least three consecutive batches. Yet 22% of FDA warning letters in fiscal year 2022 cited incomplete documentation for manufacturing changes. A recent case involved a generic drug manufacturer that failed to update their process validation records after changing a filtration system. The FDA rejected their submission, delaying product release for six weeks.
Staying Compliant in 2026: Key Steps
Here's how to navigate these requirements effectively:
- Build cross-functional teams - Include quality assurance, manufacturing, regulatory affairs, and validation specialists. A 2021 PDA study found moderate changes require 120 hours of collective effort.
- Use risk assessment tools - Implement Failure Modes and Effects Analysis (FMEA) for equipment changes, as recommended by the Parenteral Drug Association's Technical Report No. 60.
- Document everything - Maintain detailed records of change requests, risk assessments, and validation data. The FDA's 2023 draft guidance emphasizes using ICH Q9 quality risk management principles to streamline this process.
- Stay updated on global trends - The ICH Q12 guideline, adopted in November 2020, aims to standardize post-approval change management. The European Commission's 2021 revision of the Variations Regulation introduced accelerated pathways for certain Type IB changes, reducing approval timelines from 60 to 30 days for specific equipment modifications.
For companies adopting continuous manufacturing systems-a growing trend-the FDA's 2022 guidance on continuous manufacturing states that equipment changes often require PAS submissions due to interconnected process steps. This means pharmaceutical companies must rethink change control strategies for next-generation production systems.
What happens if I misclassify a manufacturing change?
Misclassification can lead to FDA warning letters, product recalls, or orders to cease distribution. For example, in Q2 2023, the FDA issued a warning letter to Lupin Pharmaceuticals for implementing a major lyophilizer replacement without PAS approval. This resulted in a 90-day production halt and $2.4 million in lost revenue. Always consult the FDA if unsure about classification.
How long does a PAS submission take?
FDA review times for PAS submissions average 6-12 months. Complex changes, like those involving new active ingredients or biologics, can take up to 18 months. The FDA's 2021 final guidance for biologics recommends early consultation with the agency to avoid delays. For time-sensitive changes, consider submitting a CBE-30 if the change qualifies as moderate.
What's the difference between CBE-30 and CBE-0?
CBE-30 requires submission 30 days before distribution, while CBE-0 is for immediate changes affecting product strength, identity, or purity. CBE-0 allows you to implement the change immediately after submitting the notification, but you must notify the FDA within 30 days. This is typically used for urgent safety issues, like correcting a labeling error that could cause patient harm.
Do small manufacturers have different requirements?
No, the regulatory requirements are the same regardless of company size. However, small and mid-sized companies often struggle with resource constraints-only 63% compliance rate per FDA inspection data compared to 98% for large companies. The FDA offers free guidance documents and workshops specifically for small businesses to help navigate these requirements.
How does the ICH Q12 guideline simplify change control?
ICH Q12 introduces a "Product Lifecycle Management" framework that allows companies to pre-approve certain changes through a Master File. This means you can submit a single application for multiple similar changes, reducing submission frequency. For example, a company could pre-approve all future equipment replacements within a specific class of machinery, cutting review times by up to 40% for routine changes.






Comments
The FDA's three-tier system for manufacturing changes is a critical framework for ensuring drug safety. While it may seem bureaucratic, each category-PAS, CBE-30, and Annual Report-is designed to mitigate risks based on the change's potential impact. For instance, a minor change like relocating a labeling station within the same facility only requires documentation in the annual report, whereas a major change like switching synthesis routes needs prior approval. Proper classification prevents costly delays and ensures patient safety. In 2023 alone, the FDA issued four warning letters for misclassified equipment changes, which can halt production for months. Companies often underestimate how small tweaks can trigger major regulatory hurdles. Even something as simple as changing a tablet press supplier can affect critical quality attributes. This is why thorough risk assessment is non-negotiable. The Parenteral Drug Association recommends using Failure Modes and Effects Analysis (FMEA) for equipment changes. Documentation is key; the FDA requires facility diagrams, process validation reports, and comparative batch data. Without proper records, submissions get rejected, causing delays. For example, a generic drug manufacturer recently faced a six-week delay due to incomplete documentation. The ICH Q12 guideline aims to simplify this process by allowing pre-approval of certain changes. But many companies still struggle with resource constraints, especially smaller ones. Compliance isn't optional; it's the foundation of patient trust.
FD warning letters are just the start Big Pharma controls the system They push minor changes through without proper oversight You think it's safe but it's not Always question authority
When handling manufacturing changes, it's vital to involve all departments. Quality assurance, manufacturing, and regulatory teams need to collaborate. For example, replacing a tablet press requires checking particle size distribution. Using FMEA helps assess risks properly. Documenting every step saves time in the long run.
I completely agree with Jennifer. Cross-functional teams are essential. In my experience, having QA, manufacturing, and regulatory all on the same page prevents delays. It's a team effort to keep patients safe. Let's work together!
Oh sure, 'Big Pharma controls the system'-because nothing says 'patient safety' like a $2 million loss from a misclassified change. FDA's warning letters are exactly what we need. Maybe instead of conspiracy theories, let's focus on proper documentation.
Brendan is right about cross-functional teams. But companies often skip the risk assessment. Like when they change a supplier for excipients. It can cause dissoulution issues. Always validate thoroughly. Document everything.
USA has the best regulatory system. Other countries don't have the same standards. FDA warnings are necessary to protect American patients. Always follow the rules strictly. No excuses for non-compliance.
Document everything.
American pharma leads the world. FDA rules keep us safe. Always follow regulations. Safety first. We've got the best system here.
Companies that misclassify changes are reckless Patient safety must come first There's no excuse for negligence Always comply with regulations
This is all a setup. FDA and big pharma collude to crush small companies. Warning letters are tools to maintain control. Always be skeptical of official stories.