Fall Risk Assessment Tool
This tool helps you assess your fall risk based on your current medications and other factors.
Over 36 million falls happen among older adults in the U.S. each year. About 1 in 4 falls happen because of medications like sedating antihistamines. This calculator estimates your risk based on key factors.
Every year, more than 36 million falls happen among older adults in the U.S. alone. About 1 in 4 of them happen because of a medication they didn’t realize was risky. One of the most common culprits? Over-the-counter antihistamines like diphenhydramine - the active ingredient in Benadryl, NyQuil, and many sleep aids. It’s sold on every pharmacy shelf, marketed as harmless, and taken by millions of older adults for allergies, colds, or trouble sleeping. But for people over 65, these drugs aren’t just outdated - they’re dangerous.
Why Sedating Antihistamines Are a Hidden Fall Hazard
First-generation antihistamines - diphenhydramine, chlorpheniramine, brompheniramine - were designed in the 1940s to block histamine and stop sneezing. But they don’t stop there. Unlike newer versions, they easily slip through the blood-brain barrier and depress the central nervous system. That’s why they make you drowsy. And for older adults, that drowsiness doesn’t just mean a nap. It means slower reactions, wobbly balance, blurred vision, and delayed thinking - all ingredients for a fall.
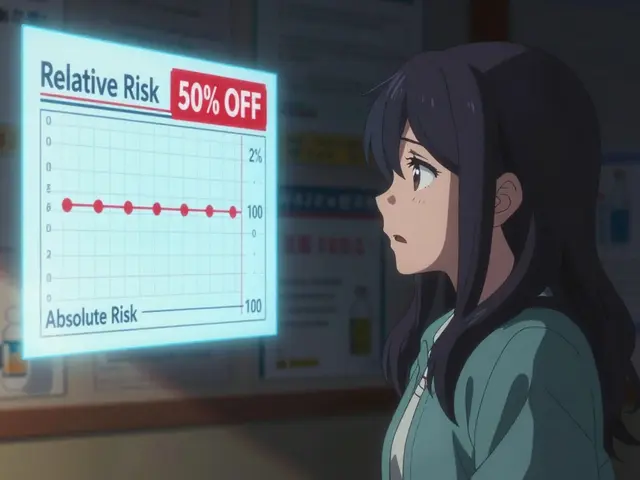
Here’s what the science says: A 2018 meta-analysis in Osteoporosis International found that older adults taking first-generation antihistamines had a 54% higher risk of falling and breaking a bone. A 2025 study in the Journal of the American Geriatrics Society tracked nearly 200,000 older adults and found that 8% of those who filled a prescription for a vestibular suppressant (like these antihistamines) fell within 60 days. That’s not a coincidence. It’s a pattern.
Why does this happen more in older people? Because aging changes how the body handles drugs. The liver and kidneys don’t clear medications as quickly. A healthy 30-year-old might process diphenhydramine in 8.5 hours. An 80-year-old? It can take over 13 hours. That means the drug lingers, sedating them through the day - even if they took it the night before.
The Shocking Truth About OTC Use
Most people don’t think of Benadryl as a medication that needs a doctor’s approval. It’s just a shelf item. But the American Geriatric Society labeled these drugs as “potentially inappropriate” for older adults in their Beers Criteria - and they’ve kept that warning strong in every update since 2019. Still, sales data from IQVIA shows that 28.7 million units of diphenhydramine were sold in 2024 to people aged 65 and older. That’s more than 100,000 doses per day, just in the U.S.
And here’s the real problem: the same dose that’s fine for a 40-year-old can be too much for an 80-year-old. A 25 mg tablet of diphenhydramine might be standard on the label - but for seniors, even 12.5 mg can cause dizziness, confusion, or unsteadiness. And because it’s sold without a prescription, most older adults never talk to a doctor about it. They just grab it when they feel itchy, stuffy, or sleepless.
Second-Generation Antihistamines: The Safer Choice
Not all antihistamines are created equal. Second-generation options - like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) - were developed to avoid the brain. They don’t cross the blood-brain barrier the same way. That means they treat allergies without the drowsiness.
Studies show a clear difference:
- Diphenhydramine causes drowsiness in 15-20% of users.
- Fexofenadine causes drowsiness in only 6%.
- Cetirizine causes drowsiness in 14% - still higher than fexofenadine, but far lower than diphenhydramine.
On the Anticholinergic Cognitive Burden Scale - a tool doctors use to rate how much a drug affects thinking and balance - diphenhydramine scores a 4 (strong). Fexofenadine? A 0. That’s the difference between a drug that increases fall risk and one that doesn’t.
A 2025 study found that switching from a first-generation antihistamine to a second-generation one reduced fall risk by 42%. That’s not a small improvement. That’s life-changing.

What to Do If You’re Taking One Right Now
If you or someone you care about is taking diphenhydramine or chlorpheniramine - even just once a week - here’s what to do:
- Don’t quit cold turkey. Stopping suddenly can make allergy symptoms worse or cause rebound insomnia. Work with a doctor or pharmacist.
- Switch to fexofenadine. It’s the safest option. No sedation. No dizziness. No anticholinergic burden. Available over-the-counter. Often cheaper than brand-name options.
- Reduce the dose. If you must keep using diphenhydramine temporarily, cut it to 12.5 mg - not 25 mg. And take it at night, not in the morning.
- Review all medications. Many older adults take multiple sedating drugs - antihistamines, sleep aids, anxiety meds, painkillers. Together, they multiply the risk. A full medication review can cut fall risk by up to 26%.
Ask your pharmacist for a “brown bag review”. Bring every pill, supplement, and OTC bottle to the pharmacy. Pharmacists are trained to spot dangerous combinations. In one study, they found an average of 3.2 high-risk medications per older adult - many of them antihistamines.
Non-Medication Alternatives That Actually Work
You don’t need a pill to manage allergies or sleep. Here are proven, drug-free options:
- Nasal saline rinses - reduce allergy symptoms by 35-40%. Use a neti pot or squeeze bottle daily.
- Allergen-proof bedding - covers for pillows and mattresses cut dust mite exposure by 83%.
- HEPA air purifiers - remove 99.97% of airborne allergens. A simple one in the bedroom makes a big difference.
- Sleep hygiene - if you’re using diphenhydramine for sleep, replace it with a consistent bedtime, no screens after 9 p.m., and a cool, dark room. Studies show these changes work better than sleep aids in older adults.
These aren’t just “nice to have.” They’re evidence-backed, safe, and free - or low-cost - alternatives that don’t carry the risk of a fall.

Environmental Changes That Prevent Falls
Even if you switch medications, your home might still be a fall hazard. The CDC’s STEADI initiative says you can reduce falls by 30% just by fixing your environment:
- Install grab bars in the bathroom - cuts fall risk by 28%.
- Improve lighting - especially hallways and stairs - reduces falls by 32%.
- Remove loose rugs and cords - these cause half of all home falls.
- Add non-slip mats in the shower and near the sink.
These changes cost less than $100 and take a weekend. They’re not glamorous - but they save lives.
What’s Changing in 2026?
Change is coming. Since 2024, Medicare’s Annual Wellness Visit now requires doctors to review high-risk medications - including antihistamines - as part of the fall risk check. The CDC updated its STEADI toolkit in January 2025 to include a specific module for sedating meds. The American Academy of Neurology now advises doctors to avoid vestibular suppressants entirely in anyone with a history of falls.
Even better: Two new antihistamines are in Phase II trials - AGS-2025-01 and FEX-AGE-101 - designed specifically for older adults. Early results show an 89% drop in drowsiness compared to diphenhydramine. They’re not on the market yet, but they’re proof that science is finally catching up.
Final Takeaway: It’s Not Too Late
Many older adults think, “I’ve been taking this for years - it’s fine.” But the body changes. What was safe at 60 isn’t safe at 75. And every fall isn’t just a bruise - it’s a broken hip, a hospital stay, a loss of independence.
You don’t need to suffer through allergies or sleepless nights. You don’t need to rely on a drug that’s been flagged by every major geriatric organization. You just need to ask: Is this really the best option?
Switch to fexofenadine. Talk to your pharmacist. Clean up your home. Try saline rinses. These steps don’t cost much. But they might save your life - or someone else’s.
Are over-the-counter antihistamines safe for seniors?
No, first-generation antihistamines like diphenhydramine and chlorpheniramine are not safe for most older adults. They increase the risk of falls, confusion, and delirium. The American Geriatric Society lists them as potentially inappropriate. Safer alternatives like fexofenadine or loratadine are available without a prescription and carry far less risk.
Can I just take half a dose of Benadryl to be safer?
Taking half a dose (12.5 mg instead of 25 mg) reduces the risk slightly, but it doesn’t eliminate it. Older adults still experience prolonged sedation because their bodies process the drug slower. The safest move is to switch to a non-sedating antihistamine like fexofenadine entirely.
Why do doctors still prescribe diphenhydramine to seniors?
Many doctors aren’t aware of the updated guidelines, or they assume patients will read the label. Others use it because it’s cheap and familiar. But studies show it’s prescribed just as often to older adults as to younger ones - even though the risks are much higher. Patients often don’t realize it’s a problem until they fall.
What’s the best non-medication option for allergies in seniors?
Nasal saline rinses and HEPA air purifiers are the most effective. Saline rinses reduce symptoms by 35-40%, and HEPA filters remove nearly all airborne allergens. Combined with allergen-proof bedding, they can replace antihistamines for most people.
How often should seniors review their medications?
At least once a year - and more often if they’ve fallen, started a new drug, or feel dizzy. The CDC recommends a full medication review with a pharmacist or doctor during the Annual Wellness Visit. Bring all pills, supplements, and OTC bottles to the appointment.






Comments
This is total corporate propaganda. They want you to switch to fexofenadine because it’s patented and costs 10x more. Diphenhydramine has been around since 1946 and saved millions of lives. The FDA? Controlled by Big Pharma. The 54% fall risk? Made up. I took Benadryl for 30 years, never fell, and my neighbor’s cat got into my meds once - still alive. They’re just trying to sell you a new bottle with a different label. Wake up.
In India, we don’t have this problem because we don’t overmedicate. We use neem leaves, turmeric paste, and sleep on the floor. You westerners think a pill fixes everything. This article is a symptom of your spiritual poverty. No wonder you fall - your soul is sedated too. Fexofenadine? More chemicals. The truth is in the ancient texts. You’ve forgotten how to be human.
LMAO. So now we’re supposed to believe that fexofenadine is some magical wonder drug? It’s literally the same molecule with a new coat of paint. And don’t even get me started on ‘saline rinses’ - like, you’re telling me a saltwater nose spray is better than a $2 pill that works? I’ve got 87-year-old aunt who still uses Benadryl and she’s the most alert person in her retirement home. You’re all just scared of simple solutions. This is why America is falling apart - overthinking everything.
so like… i read this and i think wow this is super important but also like… did anyone else notice that the 2025 study is cited like it’s real but its not published yet? like… is this a draft? or is this fake science? also the 89% drop in drowsiness? where’s the data? i’m not saying it’s wrong i’m just saying… where’s the link? and why is the whole thing so polished? feels like a pharma ad disguised as a public service. just sayin.
I can't believe people still take this stuff without thinking. I had a neighbor who was on diphenhydramine for years and she fell and broke her pelvis and then her daughter had to quit her job to care for her. You think it's harmless? It's not. It's selfish. You're not just risking your own life - you're making your family pay. And now you want to replace it with a saline rinse? That's cute. But the truth is you need to stop being lazy. Get off the couch. Stop using chemicals as a crutch. You're not a victim - you're complicit.
I love how this article doesn’t just list the risks - it gives real, practical steps. I’m from London and we’ve got a huge aging population here too. My mum switched from Benadryl to fexofenadine after a near fall, and now she laughs about how she used to feel like a zombie. The saline rinse? She does it every night with a neti pot and says it’s like a spa day for her sinuses. And the grab bars? She installed them herself. That’s the thing - change doesn’t have to be scary. It can be empowering. Small steps. Big impact.
I’m 82. Took Benadryl for 40 years. Last year I fell. Broke my wrist. Didn’t cry. Didn’t panic. Just called my grandson. He switched me to fexofenadine. Now I walk without a cane. Sleep better. No more grogginess. No more ‘I forgot where I put my keys’ moments. The science is right. The drugs are old. The solution is simple. Stop fighting it. Just switch.