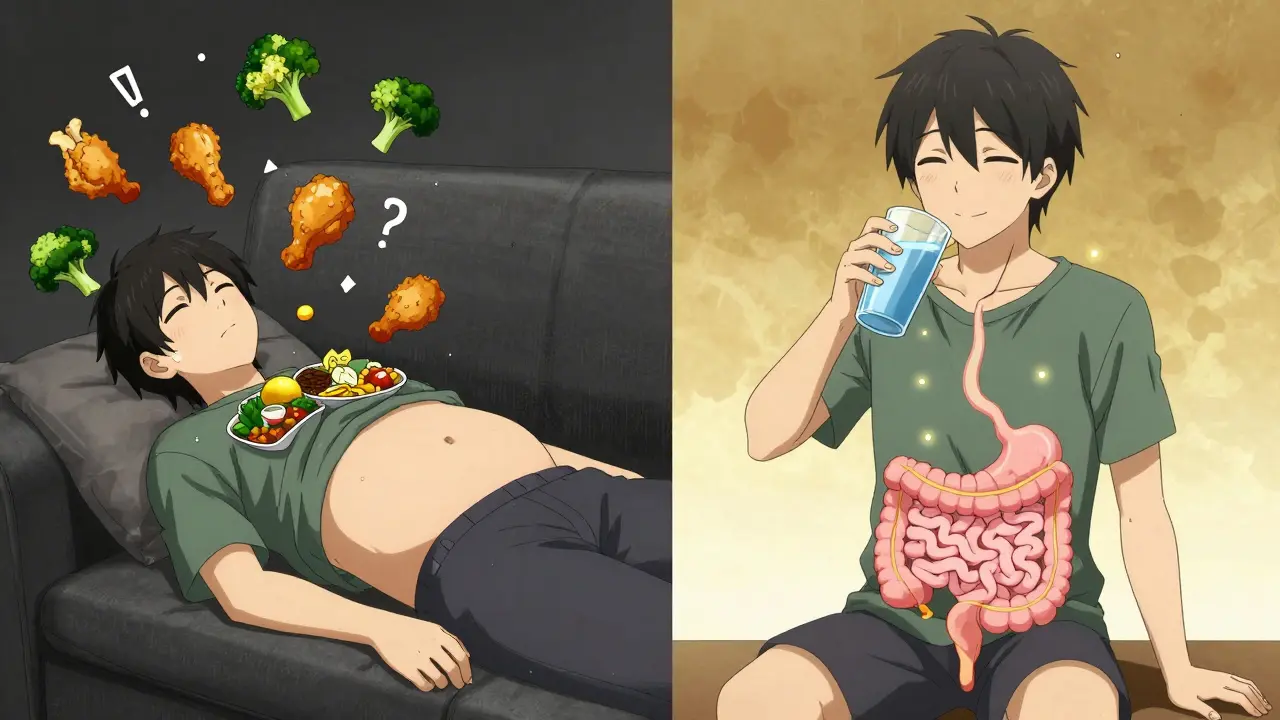
Gastroparesis isn’t just feeling full after a big meal. It’s when your stomach can’t move food into your small intestine like it should - even when there’s no blockage. Imagine eating a slice of chicken and salad, then hours later, it’s still sitting there, making you nauseous, bloated, and in pain. That’s gastroparesis. It affects about 4% of people, and if you have diabetes, your risk jumps significantly. For many, it’s a hidden condition that steals energy, sleep, and social life. But here’s the good news: diet and simple lifestyle changes can turn things around for most people.
What Exactly Happens in Your Stomach?
Your stomach isn’t just a bag that holds food. It’s a muscular pump that churns food into a fine slurry and pushes it out slowly. Gastroparesis breaks this system. The nerves controlling the stomach muscles - especially the vagus nerve - get damaged. This is common in long-term diabetes, after surgery, or sometimes for no clear reason at all. Without proper nerve signals, the stomach doesn’t contract right. Food lingers. And that’s when symptoms start.
Most people notice nausea first - up to 90% do. Then vomiting, early fullness (after just a few bites), and that heavy, bloated feeling after eating. Some get heartburn or belch a lot. These symptoms don’t come and go; they stick around for months. Doctors diagnose it when less than 40% of a meal leaves the stomach after two hours. That’s measured with a gastric emptying scan - a simple test where you eat food with a harmless tracer and get scanned over time.
Who’s Most at Risk?
Gastroparesis hits women four times more often than men. It’s also tightly linked to diabetes. Up to half of people with type 1 diabetes and about 30% of those with type 2 diabetes will develop it over time. That’s because high blood sugar damages nerves - including the vagus nerve. But it’s not just diabetics. People who’ve had stomach surgery, those with autoimmune diseases like scleroderma, or even some with viral infections can develop it. About one in three cases have no known cause - called idiopathic gastroparesis.
What makes it worse? Eating too fast, drinking with meals, or choosing foods that take forever to digest. Fat slows emptying by 30-50%. Fiber from raw veggies, whole grains, or tough meats doesn’t break down easily. Carbonated drinks puff up your stomach. All of these make symptoms flare.
The Diet That Actually Works
Most people with gastroparesis get better - not with pills, but with food. Studies show 65% of patients see big improvements just by changing what and how they eat. Here’s what works:
- Small meals, often. Eat 5 to 6 tiny meals a day instead of 3 big ones. Each meal should be no more than 1 to 1.5 cups. That’s about the size of a tennis ball.
- Low fat, low fiber. Avoid fried foods, fatty meats, butter, cream, and cheese. Skip raw broccoli, apples with skin, beans, and whole grains. Choose cooked vegetables, peeled fruits, lean ground meat, eggs, and soft tofu.
- Blend it. If chewing feels like too much work, blend your food. Smooth soups, pureed chicken, oatmeal, and yogurt are easier. Aim for particles smaller than 2mm - that’s the size of a grain of sand.
- Separate solids and liquids. Drink water 30 minutes before or after meals, not with them. Drinking while eating fills your stomach faster and makes bloating worse.
- Stay upright. Don’t lie down for at least two hours after eating. Gravity helps move food along.
Keep a food diary. Write down what you eat and how you feel two hours later. Most people find 3-5 trigger foods that make them sick - maybe it’s cabbage, nuts, or orange juice. Eliminate them one by one. Working with a dietitian who knows gastroparesis cuts your risk of malnutrition by 40%.
What to Eat and What to Avoid
| Good Choices | Bad Choices |
|---|---|
| Blended soups, broths | Fried chicken, pizza, burgers |
| Ground turkey or lean beef | Steak, pork chops, sausages |
| Cooked carrots, zucchini, squash | Raw broccoli, kale, corn |
| Peeled applesauce, bananas, melon | Apples with skin, berries, pears |
| White rice, pasta, refined bread | Brown rice, whole wheat bread, bran cereal |
| Water, weak tea, clear juices | Soda, sparkling water, alcohol |
| Yogurt, custard, pudding | Cheese, ice cream, heavy cream |
Hydration matters too. Sip 1-2 ounces of water every 15 minutes throughout the day. Don’t chug. Large volumes stretch your stomach and trigger nausea. Aim for 4-6 cups total per day.
When Diet Isn’t Enough
Some people need more. If symptoms don’t improve after 8-12 weeks of strict diet changes, talk to your doctor about medications. Metoclopramide can help the stomach empty faster - but it’s not for long-term use. It can cause serious muscle movements in the face and neck if taken too long. Domperidone is another option, though it’s harder to get in some countries.
For severe cases, there’s gastric electrical stimulation (GES). It’s like a pacemaker for your stomach. A small device is implanted under the skin and sends gentle pulses to help muscles contract. About 70% of people with stubborn symptoms get at least half their vomiting under control.
There’s also a newer procedure called per-oral pyloromyotomy (POP). A doctor uses a scope to cut the muscle at the bottom of the stomach - the pylorus - to let food pass more easily. Success rates are 60-70%.
In rare cases, when people can’t eat enough to survive, they need feeding tubes or IV nutrition. But that’s only for the most severe, advanced cases.

What Happens If You Ignore It?
Left untreated, gastroparesis doesn’t just make you feel bad - it can be dangerous. Undigested food can harden into bezoars - solid masses that block the stomach. About 6% of people develop them, and 2% need surgery to remove them.
Dehydration is common from constant vomiting. You lose potassium and sodium, which can cause dizziness, heart rhythm problems, or even hospitalization. About 25% of moderate to severe cases end up in the hospital for this.
For diabetics, it’s a nightmare. Food sitting in the stomach means sugar doesn’t enter the bloodstream on time. Blood sugar swings wildly - high one hour, low the next. This makes diabetes harder to control and increases long-term damage to eyes, kidneys, and nerves.
Weight loss is another risk. About 20% of people lose more than 10% of their body weight. Malnutrition can lead to muscle loss, fatigue, and weaker immunity.
Living With It - Real Life Tips
It’s not just about food. Gastroparesis affects your whole life. Seventy-five percent of people say it limits daily activities. Forty percent can’t work full-time. Anxiety around eating is common - 65% avoid meals with friends because they’re scared of vomiting.
Start small. Don’t try to overhaul your diet overnight. Pick one change: maybe stop drinking soda, or switch to blended meals. Track your progress. Celebrate when you eat a full meal without nausea. That’s a win.
Connect with others. Online support groups for gastroparesis are full of people sharing recipes, tips, and encouragement. You’re not alone.
And don’t give up. Most people who stick with the diet see big improvements in 8-12 weeks. Some even get back to normal life - cooking, traveling, eating out. It takes patience, but it’s possible.
What’s Next in Treatment?
Research is moving fast. A new drug called relamorelin, which mimics a natural stomach hormone, showed 35% improvement in emptying in recent trials. It’s not approved yet, but it’s coming. Scientists are also testing probiotics - good bacteria that may help regulate gut movement. Early results show 30% fewer symptoms.
Artificial intelligence is being used to read gastric scans faster and more accurately. And one day, doctors may match your treatment to your genetics - knowing ahead of time which drug or diet will work best for you.
For now, the best tool you have is your fork. What you eat matters more than any pill. Stick with the plan. Your stomach will thank you.
Can gastroparesis go away on its own?
In rare cases, especially after a viral infection, gastroparesis can improve over months without treatment. But if it’s caused by diabetes or nerve damage, it’s usually chronic. That doesn’t mean it’s untreatable - most people control symptoms well with diet and lifestyle changes. Don’t wait to see if it gets better. Start managing it now.
Is a liquid diet the only option?
No. While liquids are easier to digest and often used early on, most people can move to soft, blended solid foods. Think mashed potatoes, ground chicken in sauce, smooth yogurt, or cooked oatmeal. The goal isn’t to live on shakes forever - it’s to find textures your stomach can handle. Many people return to eating normal-looking meals, just smaller and softer.
Can I still eat fruit?
Yes - but not raw. Avoid apples, pears, berries, and citrus with skin or seeds. Instead, choose peeled, cooked, or blended fruits like applesauce, banana, melon, or canned peaches in juice. Pureeing breaks down the fiber so your stomach doesn’t have to work as hard.
Does stress make gastroparesis worse?
Yes. Stress slows digestion and can worsen nausea and bloating. Many people report flare-ups during stressful times. Managing stress through gentle exercise, breathing techniques, or counseling helps. You don’t need to be perfect - just consistent. Even 10 minutes of deep breathing before meals can make a difference.
Can I drink alcohol with gastroparesis?
It’s not recommended. Alcohol slows stomach emptying and irritates the gut lining. It can also worsen dehydration and interfere with blood sugar control if you have diabetes. If you choose to drink, limit it to a tiny amount - like half a glass of wine - and never on an empty stomach. But for best results, avoid it altogether.
How long until I feel better on a gastroparesis diet?
Most people start noticing improvements within 2-4 weeks - less nausea, less bloating. But full results take 8-12 weeks. That’s because your stomach needs time to adjust to smaller, softer meals. Stick with it. If you don’t see progress by 12 weeks, talk to your doctor about adding medication or seeing a specialist.








Comments
I was diagnosed last year and honestly, this post saved my life. Started with blended soups and cutting out soda - within two weeks, I wasn’t vomiting after dinner anymore. Small wins matter. Keep going.
The gastric emptying scan protocol you referenced is outdated. Modern protocols now use scintigraphy with a 13C-octanoic acid breath test as the gold standard for quantifying gastric emptying kinetics - particularly in diabetic gastroparesis cohorts. The 40% threshold is arbitrary; the 2-hour retention metric lacks sensitivity for partial motility disorders. You should update your diagnostic criteria.
Nobody talks about how the pharmaceutical industry pushes meds like metoclopramide because they make billions while the real solution - diet - is free and ignored because it doesn't have a patent
i tried the blended thing and it was a game changer honestly like i didnt think i could eat anything without feeling like i was gonna die but now i can have oatmeal and applesauce and it doesnt feel like a battle
It is imperative to underscore, with the utmost gravity, that the pathophysiological underpinnings of gastroparesis are not merely a matter of dietary modification, but rather a profound dysregulation of the enteric nervous system - specifically, the vagal efferent fibers that govern gastric peristalsis. When these neural pathways are compromised - whether by chronic hyperglycemia, post-surgical adhesions, or idiopathic degeneration - the stomach's intrinsic pacemaker activity becomes erratic, leading to stasis, fermentation, and the resultant cascade of gastrointestinal distress. Therefore, one must approach this condition not as a culinary inconvenience, but as a neurogastroenterological emergency requiring systematic, multidisciplinary intervention.
In Nigeria, we have a traditional remedy called 'ogiri' - fermented melon seed paste - used in soups. It’s naturally low-fiber, fermented, and helps with gut motility. Some patients with mild gastroparesis report less bloating when it’s added to blended stews. Not scientifically proven, but culturally rooted. Worth a try if you’re open to it.
You don’t need to overhaul everything at once. Start with one thing - maybe swap your morning bagel for oatmeal. Just one change. Then another. You’re not failing if you slip. You’re learning. Progress isn’t linear. It’s messy. And that’s okay.
I used to think I was just a slow digester until I read this. Then I found a Reddit group called 'Gastroparesis Warriors' and everything changed. I made a banana-coconut smoothie with chia seeds soaked overnight - turned out it was actually digestible because the chia was gelatinized. Who knew? I’m now eating actual food, not just liquids. Thank you for this.
This is why people are weak today. In my village we ate raw vegetables and heavy meat and never complained. If your stomach cannot handle food then you are not strong enough. The body is a temple. You must suffer to be purified.
I mean... if you're eating blended food and avoiding carbs... are you even living? 😭 I used to have Sunday roast with mashed potatoes and gravy. Now I'm sipping pea soup like some sad monk in a monastery. This isn't management. This is a culinary prison. 🥲
I must say, I find it deeply concerning that this article promotes a 'diet-first' approach without mentioning the role of gut microbiome dysbiosis. The fact that you did not reference the 2023 study from Johns Hopkins linking gastroparesis to reduced Faecalibacterium prausnitzii levels suggests a dangerous lack of scientific rigor. You are misleading vulnerable people.
You know what they don’t tell you? The FDA approved metoclopramide because Big Pharma paid off the regulators. And the gastric pacemaker? It’s made by a company owned by the same people who make insulin. Diabetes + gastroparesis = double profit. They want you dependent. Don’t fall for it. 🕵️♀️💧 #GastroparesisConspiracy
The assertion that 65% of patients improve with dietary intervention is statistically dubious. The cited study lacks a control group, has no long-term follow-up, and was conducted by a non-peer-reviewed wellness blog. This is anecdotal evidence masquerading as medical guidance. You are doing more harm than good.
In my culture, we say: 'The stomach is the first heart.' When it suffers, the whole body weeps. But we also believe healing comes from rhythm - not force. Eat at the same time. Sit quietly. Breathe before each bite. Let food come to you, not the other way around. This is not just diet. It is sacred practice.