Every year, over 1.5 million people in the U.S. suffer preventable harm from medication errors. Many of these mistakes happen because someone didn’t stop to check the medication name, strength, or dosage form before giving or taking a drug. It’s not always a mistake by a doctor or pharmacist. Sometimes, it’s a quick glance at a label, a misread abbreviation, or a rushed decision. You don’t need to be a nurse or pharmacist to spot these red flags. If you’re taking medications, helping a loved one, or even just picking up a prescription, knowing how to verify these three things can save your life.
Why Checking Medication Details Isn’t Optional
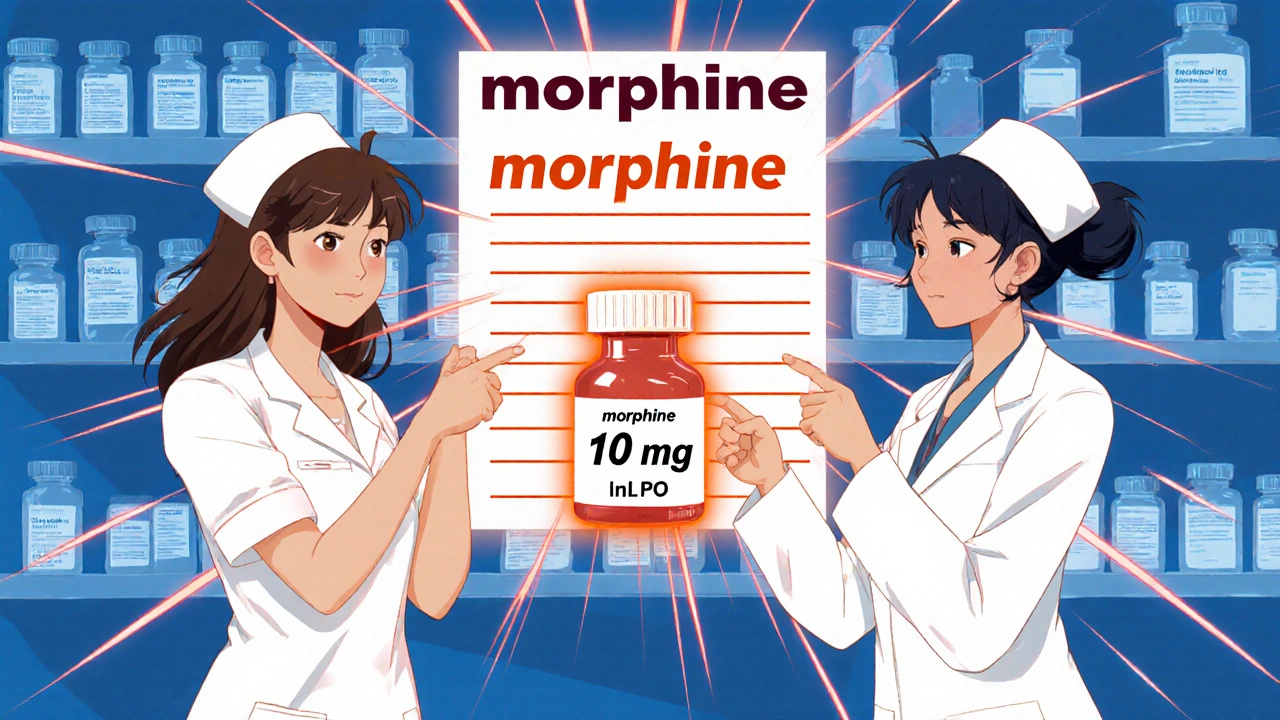
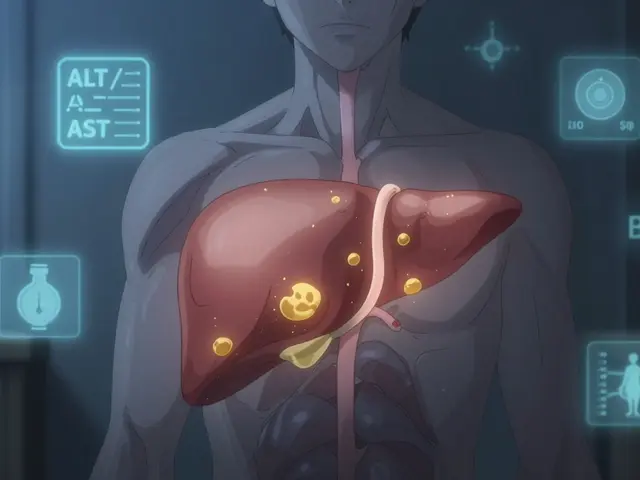
Medication errors aren’t rare. They’re common - and often deadly. The Agency for Healthcare Research and Quality (AHRQ) reports that about 7,000 people die each year in U.S. hospitals from preventable medication mistakes. Many of these happen because someone confused one drug for another. Think of it like this: if you handed someone a bottle labeled "Lunesta" but meant "Lisinopril," they’d be taking a sleep aid instead of a blood pressure pill. That’s not just a mix-up. That’s dangerous. The biggest culprits? Look-alike and sound-alike names. Prednisone and Prednisolone. Hydralazine and Hydroxyzine. Insulin U-100 and Insulin U-500. These aren’t theoretical risks. In 2023, Reddit users shared over 140 real stories of errors caused by these confusions. One person accidentally took 10 times their insulin dose because they misread "U-100" as "U-10." Another received oral morphine instead of an injectable version because the dosage form wasn’t written clearly. The fix isn’t high-tech. It’s simple: slow down. Check the name. Check the strength. Check the form. Do it every time.Step 1: Verify the Medication Name
The first thing you need to confirm is the exact drug name. Don’t assume. Don’t guess. Don’t rely on memory. Start with the prescription or the label on the bottle. Compare it to what your doctor told you. If the name looks unfamiliar, look it up. Use trusted sources like the FDA’s DailyMed database or MedlinePlus - not random websites or chatbots. Watch out for abbreviations. "MS" could mean morphine sulfate or magnesium sulfate. "U" for units can be mistaken for "0" or "cc." That’s why the FDA and ISMP banned these abbreviations in 2003. If you see them, ask for clarification. Always write out "units," "micrograms," and "milligrams." Never use "mcg," "μg," or "U." Also, pay attention to capitalization. The FDA recommends "Tall Man" lettering for similar drugs: predniSONE vs. predniSOLONE. The uppercase letters help your brain catch the difference. If the label doesn’t use this formatting, ask if it’s available.Step 2: Confirm the Strength - Numbers and Units Matter
Strength tells you how much of the drug is in each unit. Get this wrong, and you’re either underdosing or overdosing. For tablets and capsules, strength is always in milligrams (mg) per tablet. A 5 mg tablet of lisinopril is not the same as a 20 mg tablet. For liquids, it’s mg per mL. Heparin might be 5,000 units per mL - or 50 units per mL. That’s a 100-fold difference. One mistake, and you could bleed out. Always check the unit. Never assume. If the label says "10mg," make sure there’s a space: "10 mg." No space? That’s a red flag. The Institute for Safe Medication Practices found that simply adding a space between the number and unit reduces errors by 12%. That’s because "10mg" can look like "100 mg" if the font is small. Also, never trust a decimal without a leading zero. Write "0.5 mg," not ".5 mg." That tiny zero prevents misreading the dose as 5 mg - ten times too strong. For injectables, avoid ratio formats. Epinephrine 1:10,000 should be written as 0.1 mg/mL. Ratios are confusing. Numbers with units are clear. If you see a ratio, ask for the concentration in mg/mL or units/mL.Step 3: Identify the Dosage Form - Oral, Injected, Topical?
The dosage form tells you how the drug is meant to be used. Taking a pill meant for injection can kill you. Putting a liquid meant for the eye into your mouth is dangerous too. Common dosage forms:- Tablet
- Capsule
- Oral liquid (syrup, solution)
- Injection (IV, IM, SC)
- Topical (cream, ointment, patch)
- Inhaler
- Suppository
When to Double-Check - The Three Critical Moments
You don’t check medication details once. You check them three times:- When you receive the prescription - Does it include the full name, strength, dosage form, route (e.g., PO, IV), and frequency? If any part is missing, call the prescriber. Don’t assume.
- When you prepare the medication - Compare the label on the bottle or vial to the written order. Does the name match? The strength? The form? Use the "five rights": right patient, right drug, right dose, right route, right time.
- Before you give or take it - Look at the medication one last time. Read the label out loud. Say the name, strength, and form. If you’re helping someone else, have them repeat it back. This "read-back" method is used in 89% of successful error prevention stories reported by nurses.
Technology Helps - But Doesn’t Replace You
Hospitals use barcode scanners, electronic health records, and AI systems to flag errors. Epic and Cerner systems can catch look-alike names and incorrect doses. Barcode scanning reduces dispensing errors by 83%. But technology fails. A 2020 study by The Joint Commission found that 18% of errors happened because staff trusted the system too much. They ignored a mismatch because the computer said "approved." That’s called automation bias. Your eyes, your brain, your voice - those are still the most reliable tools. If the system says "10 mg" but the vial says "100 mg," don’t press "confirm." Stop. Ask. Verify.What to Do If Something Doesn’t Look Right
You’re not overreacting if you’re unsure. You’re being smart. Here’s what to do:- Don’t take it. Don’t give it.
- Compare the label to the original prescription or order.
- Call the pharmacy or prescriber. Say: "I’m verifying this medication. Can you confirm the name, strength, and form?"
- If you’re in a hospital, ask to speak with the pharmacist on duty. Pharmacists are trained to catch these errors.
- Document what you saw. Write down the discrepancy. It protects you and helps prevent future mistakes.
Common Mistakes Even Professionals Make
Even trained staff slip up. Here are the top errors seen in hospitals and pharmacies:- Confusing insulin strengths (U-100 vs. U-500)
- Misreading "mcg" as "mg" - a 1,000-fold overdose risk
- Using "U" for units instead of writing "units"
- Missing the dosage form - giving an oral liquid as an injection
- Assuming the dose is right because "it’s what they usually get"
How to Build a Safety Habit
You don’t need to memorize every drug. You just need to make checking a habit. Start with these three rules:- Read it out loud. Say the full name, strength, and form. Your ears catch what your eyes miss.
- Never trust abbreviations. If it’s not spelled out, ask.
- Check every time. Even if you’ve taken this drug for years. Doses change. Formulations change. Labels change.
Final Thought: You’re the Last Line of Defense
Doctors prescribe. Pharmacists dispense. Nurses administer. But you - the person taking the medicine - are the last person who sees it before it goes in your body. No system is perfect. No computer catches every mistake. But you can. All it takes is slowing down, reading carefully, and speaking up. Medication safety isn’t about being perfect. It’s about being present. And if you’re reading this, you’re already on the right path.What should I do if a medication label doesn’t include the strength or dosage form?
Never take or give a medication if the label is missing the strength (e.g., 5 mg) or dosage form (e.g., tablet, liquid). Contact the pharmacy or prescriber immediately. A missing strength or form is a serious safety violation. In the U.S., the American Society of Health-System Pharmacists (ASHP) requires all orders to include these details. If they’re not there, the order is incomplete and unsafe.
Is it safe to rely on the pharmacy’s label instead of the doctor’s prescription?
No. Always compare the pharmacy label to the original prescription or electronic order. Pharmacists make mistakes too. A 2020 study found that 83% of dispensing errors were caught by patients or caregivers who double-checked. The label is a guide - not a guarantee. Verify the name, strength, and form yourself.
Can I use a pill splitter to change the dosage if the strength is wrong?
Never use a pill splitter to adjust a dose unless your doctor or pharmacist specifically says it’s safe. Many pills are designed to release medication slowly (extended-release). Cutting them can cause a dangerous overdose. Also, not all pills can be split evenly. If you need a different strength, ask for the correct tablet - don’t try to make one yourself.
Why do some medications have "Tall Man" lettering on the label?
Tall Man lettering uses uppercase letters to highlight differences between similar drug names - like predniSONE and predniSOLONE. This visual cue helps prevent confusion. The Institute for Safe Medication Practices found this practice reduces errors by 76%. If your medication doesn’t use it, ask if a version with Tall Man lettering is available.
What should I do if I notice a recurring error with a specific medication?
Document the error - write down what happened, when, and what you saw. Report it to your pharmacist, doctor, or hospital safety team. In the U.S., you can also report medication errors to the FDA’s MedWatch program. Your report helps improve safety systems for everyone. Don’t assume it’s just you - if you saw it, others may have too.






Comments
Just took my insulin and noticed the label said U-100 but the bottle looked weird. Didn’t check. Now I’m sweating. Should’ve read the damn thing. Fuck.
Thank you for writing this. I’m a caregiver for my mom and I never realized how easy it is to make a mistake. I started reading every label out loud now. It feels silly but it’s saved us twice. You’re right - slowing down isn’t boring, it’s brave.
The FDA’s so-called "Tall Man" lettering is a pathetic Band-Aid on a systemic failure. The real issue? Pharmaceutical companies deliberately design drug names to be confusing - it’s a monetization strategy. Look at the patent filings for "Lunesta" vs. "Lisinopril" - both were intentionally engineered for phonetic ambiguity. This isn’t negligence. It’s corporate malfeasance. And don’t get me started on how the DEA allows U-100 to still exist alongside U-500. This is how people die in plain sight.
Okay but have you heard about the secret FDA memo from 2021 that says they’re actually encouraging look-alike names because it increases prescription volume? I found a redacted PDF on a dark web forum from a whistleblower who used to work at a compounding pharmacy - they were told to "optimize for confusion" to boost sales. And now they’re telling us to just "read the label"? That’s like telling people to check if their car’s brakes are working after the manufacturer installed fake pads. I’ve been taking my blood pressure med for 8 years and I just found out it was supposed to be a patch. My doctor never told me. I think I’ve been poisoned. I’m going to the ER. Someone call the news.
i just started helping my dad with his meds and i didn’t know about the leading zero thing. i’ve seen .5mg so many times. i always thought it was just how they wrote it. now i’m double checking every bottle. also, i think i saw a "U" on one of his pills… should i be worried?
Read it out loud. Every time. Changed everything.
The pharmacokinetic implications of misidentifying dosage form are nontrivial - particularly with extended-release formulations. Oral ingestion of an IV-administered agent bypasses first-pass metabolism and can precipitate acute toxicity. The five rights framework remains the gold standard, though I’ve observed increasing noncompliance in outpatient settings due to workflow inefficiencies and EHR interface design flaws.
It is regrettable that the general populace must assume the burden of error prevention that ought to rest squarely upon institutional safeguards. The onus should not be on the layperson to decipher typographical ambiguities in pharmaceutical labeling. The absence of standardized, legible, and unambiguous nomenclature across all dispensing systems is a failure of regulatory oversight - not a personal failing of the patient.
YOU ARE THE LAST LINE OF DEFENSE 💪🩺✨
Yes, you. The one scrolling Reddit at 2am with a pill in your hand. You’re not paranoid. You’re a superhero. 🦸♀️
Read it out loud. Say it like you’re reading a spell. "Fifteen milligrams of lisinopril. Oral tablet. Not the liquid. Not the patch. NOT THE INJECTION."
Now take it. You got this. And if you’re ever unsure? Call the pharmacy. They won’t judge. They’ll be proud of you. 🌟